Abstract
Purpose
Multiple miliaryosteoma cutis (MMOC) is a rare nodular skin disease, characterized by tiny bone nodules in the dermis and subcutaneous tissue, presenting clinically as multiple normochromic papules and nodules, usually on the face. We described the case of MMOC of the face in a woman, ultrasonically evaluated with very high frequency probe.
Materials and methods
A 45-year-old patient with multiple papules, 3–5 mm in diameter, grouped in the frontal region. Skin ultrasound examination, cutaneous biopsy and laboratory evaluation were performed.
Results
High-frequency ultrasound showed the presence of multiple hyperechogenic linear and roundish structures, associated by hypoechogenic shadow. The histology revealed a normal orthokeratotic stratified epithelium with fragment of mature lamellar bone localized at level of the reticular dermis. Laboratory evaluation was normal. According to the clinical, pathological, laboratory and instrumental analyses, a final diagnosis of miliaryosteoma cutis (or primary osteoma cutis not associated with Albright’s hereditary osteodystrophy) was made.
Conclusion
In case of multiple papules of subcutaneous tissue, the diagnosis of MMOC, although rare, should be considered and high-frequency sonography, identifying the calcifications, suggests diagnosis.
Keywords: Osteoma cutis, High-frequency sonography, Multiple calcifications
Introduction
Osteoma cutis (OS) can be considered as an aberrant development or deposit of bone tissue within the skin. This condition can be classified as primary or secondary. Primary osteoma can be associated with rare genetic disorders (as Albright’s hereditary osteodystrophy) or not be associated to multiple miliaryosteoma of the face, widespread osteoma, and plaque-like osteoma. Secondary osteoma cutis represents about 85 % of cases and may occur in various conditions including acne, scleroderma, panniculitis, dermatomyositis, and tumors such as basal cell carcinoma and pilomatricoma [1]. Multiple miliaryosteoma cutis (MMOC) is a rare nodular skin disease, characterized by tiny bone nodules in the dermis and subcutaneous tissue in middle age, presenting clinically as multiple normochromic papules and nodules usually on the face. An extra-facial involvement occurs in 15 % of patients [2]. To date, only 51 cases are reported in the literature showing high prevalence in female patients (about 88 % of cases) versus male patients (12 %). Its etiology is still unknown, although about 55 % of patients have a personal medical history positive for acne [3]. A correct clinical, laboratory, pathological, and radiological examination plays a pivotal role in the identification of this rare cutaneous disorder. Frequently, MMOC can be considered as a diagnosis of exclusion. We described the case of MMOC of the face in a woman ultrasonically evaluated with very high frequency probe, performing also a review of the main differential diagnosis.
Case description
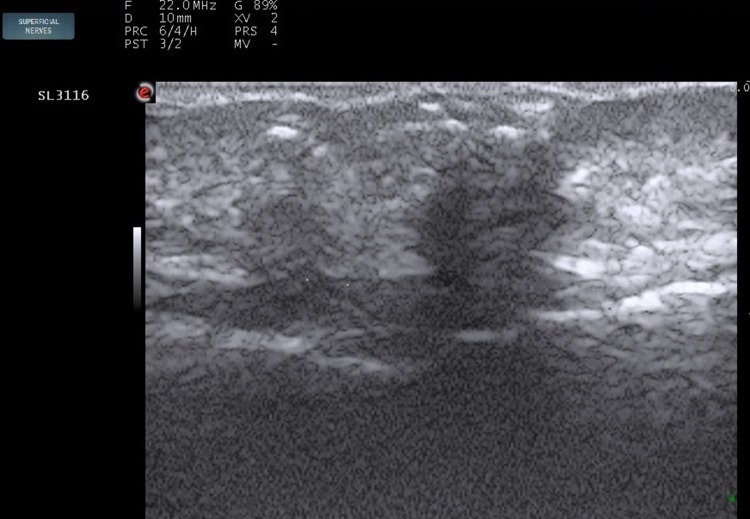
A 45-year-old patient was presented to our Ultrasound Department with multiple normochromic mildly hardened papules, on palpation, 3–5 mm in diameter, grouped in the frontal region (Fig. 1). The lesions had appeared 5 years before and were not painful and gave no itching; however, a significant subjective cosmetic discomfort was present. The patient denied any familial or personal history of acne, dermatological disorders, and genetic or acquired disorders. A skin ultrasound examination (22 MHz probe; EsaoteMyLab One, Genoa, Italy) showed the presence of multiple hyperechoic linear and roundish structures associated by a hypoechoic shadow; these aspects were compatible with multiple calcifications mainly disposed at the level of superficial parts of the dermis (Fig. 2). After our examinations, the patient was sent to the dermatological unit, where according to the clinical features, a cutaneous biopsy was performed. The histology revealed a normal orthokeratotic stratified epithelium with fragments of mature lamellar bone localized at the level of the reticular dermis. In the bone, collagen fibers were arranged in parallel arrays, while cartilaginous materials and/or chondrocytes were not observed (Fig. 3). Laboratory evaluation was normal. In particular, count blood cells (CBC), creatinine, alkaline phosphatase, calcium serum levels, parathormone and phosphorus serum levels, TSH resistance, and hand X-ray were all in normal ranges. According to the clinical, pathological, laboratory, and instrumental analyses, a final diagnosis of miliaryosteoma cutis (or primary osteomacutis not associated with Albright’s hereditary osteodystrophy) was made.
Fig. 1.

Multiple skin-colored popular-nodular lesions 861 × 460 mm
Fig. 2.
Evidence of numerous linear and roundish calcifications in superficial planes 230 × 159 mm
Fig. 3.
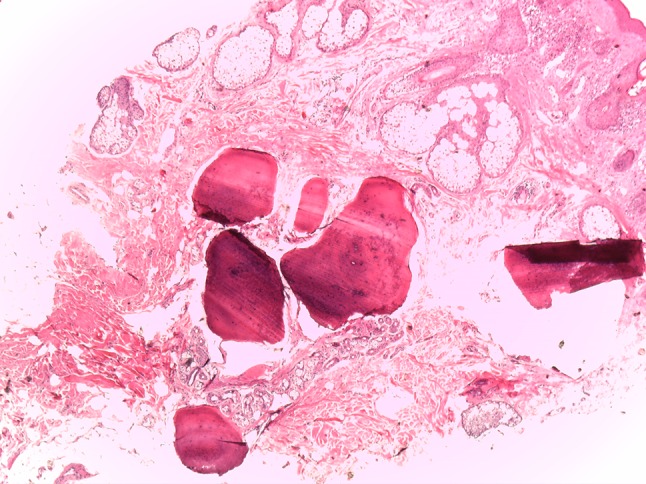
Fragment of mature lamellar bone localized on the dermis 541 × 406 mm
Discussion
OS is usually divided into primary and secondary. At the same time, primary OS is divided into primary OS associated or not associated with Albright’s hereditary osteodystrophy [4]. Primary OS associated with Albright’s hereditary osteodystrophy (caused by a mutation in the GNAS gene) includes two syndromes: pseudohypoparathyroidism and pseudopseudohypoparathyroidism. The first syndrome is characterized by the presence of a resistance to the parathyroid hormone and clinically shows hypocalcemia, hyperphosphatemia, increased serum concentration of parathyroid hormone (PTH), insensitivity to the biologic activity of PTH, obesity, mental disability, short stature, round faces, ganglia calcification, and osteoma cutis. The second one is characterized by the presence of normal laboratory investigations (compared with pseudohypoparathyroidism), but the same clinical features of the pseudohypoparathyroidism. Primary OS not associated with Albright’s hereditary osteodystrophy includes multiple miliaryosteoma of the face, isolated osteoma, widespread osteoma, and plaque-like osteoma. Secondary OS represents 85 % of the cases of cutaneous ossification, and they appear in association with other antecedent cutaneous diseases such as connettivitis (dermatomyositis, scleroderma, lupus erythematosus, CREST syndrome), primary cutaneous proliferations (basal cell carcinoma, pilomatricoma, hemangioma), cutaneous infections and inflammations (folliculitis, syphilis, pyogenic granuloma), and cutaneous metastases (metastatic bronchogenic carcinoma of the lung). Ultrasound cannot replace the histological examination as it cannot differentiate the calcifications by the neoformation of bone tissue. However, the ultrasonographic pattern associated with clinical characteristics (mainly sex and anatomical site) oriented toward this diagnosis, being the differential diagnosis to be placed mainly against comedones, sebaceous nevus, cutaneous calcinosis, and pseudoxantoma elasticus. Laboratory, bioptical examinations, and skin ultrasound can play a pivotal role in the diagnosis. According to our knowledge, to date, only Thielen et al. reported the use of ultrasonography in the diagnosis of multiple osteoma cutis, but using a probe of the older generation with lower frequency and a field of view definitely largest. In this regard and according to our radiological finding, the main characteristics of MMOC are hyperechoic structures associated by hypoechoic shadow. Our patient can be classified as primary OS not associated with Albright’s hereditary osteodystrophy. In fact, her personal medical history was negative for acne and/or other conditions included in the secondary forms of OS.
Miliaryosteoma cutis (MMOC) was described for the first time by Virchow, and subsequently, a pathogenesis role of acne was described for the first time in 1928 by Hopkins. Although the pathogenesis is currently unknown, Myllylä et al. showed that dermal fibroblasts have the ability to differentiate into osteoblasts producing also osteonectin, while the erroneous localization of mesenchymal cells in the contest of the dermis, differentiating in osteogenic lineage, could be another important point in the pathogenesis. However, in the same paper, authors concluded that the etiology of this disease is not associated with GNAS-related disorders and, therefore, it remains still unknown. Although our patient refused any treatments, various medical and surgical therapies have recently been found for this class of patients (after excluding an underlying disease). In this regard, the surgical excision of the larger lesions is the treatment of choice for symptomatic patients, and a sonography study may help in localizing smaller lesions. While microincision extirpation, CO2 laser, and topical application of tretinoin are other useful treatments for the small lesions [5], synthetic bisphosphonates (as etidronate disodium) are not very effective as treatment.
Compliance with ethical standards
Conflict of interest
The authors declare tha t they have no conflict of interest.
Ethical standard
All human and animal studies have been approved by the appropriate ethics committee and have, therefore, been performed in accordance with the ethical standards laid down in the Helsinki Declaration of 1975 and its late amendments. Additional informed consented was obtained from all patients for which identifying information is not included in this article.
References
- 1.Aguinaga F, Trope B, Piñeiro-Maceira J, Ramos-e-Silva M. Miliary osteoma cutis: a case report. Case Rep Dermatol Med. 2014 doi: 10.1155/2014/347829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myllylä RM, Haapasaari M, Palatsi R, et al. Multiple miliary osteoma cutis is a distinct disease entity: four case reports and review of the literature. Br J Dermatol. 2011;164(3):544–552. doi: 10.1111/j.1365-2133.2010.10121.x. [DOI] [PubMed] [Google Scholar]
- 3.Thielen AM, Stucki L, Braun RP, et al. Multiple cutaneous osteomas of the face associated with chronic inflammatory acne. J Eur Acad Dermatol Venereol. 2006;20(3):321–326. doi: 10.1111/j.1468-3083.2006.01425.x. [DOI] [PubMed] [Google Scholar]
- 4.Fazeli P, Harvell J, Jacobs MB. Osteoma cutis (cutaneous ossification) West J Med. 1999;171(4):243–245. [PMC free article] [PubMed] [Google Scholar]
- 5.Kim SY, Park SB, Lee Y, Seo YJ, Lee JH, Im M. Multiple miliary osteoma cutis: treatment with CO(2) laser and hook. J Cosmet Laser Ther. 2011;13(5):227–230. doi: 10.3109/14764172.2011.613481. [DOI] [PubMed] [Google Scholar]