Abstract
Depression and falls have a significant bidirectional relationship. Excessive fear of falling, which is frequently associated with depression, also increases the risk of falls. Both depression and fear of falling are associated with impairment of gait and balance, an association that is mediated through cognitive, sensory, and motor pathways. The management of depression in fall-prone individuals is challenging, since antidepressant medications can increase the risk of falls, selective serotonin reuptake inhibitors may increase the risk of fragility fractures, and data are lacking about the effect of fall rehabilitation programs on clinically significant depression. Based on the current state of knowledge, exercise (particularly Tai Chi) and cognitive–behavioral therapy should be considered for the first-line treatment of mild depression in older fallers. Antidepressant medications are indicated to treat moderate to severe depression in fall-prone individuals, but with appropriate precautions including low starting dose and slow dose titration, use of psychotropic monotherapy whenever possible, and monitoring for orthostatic hypotension and hyponatremia. To date, there have been no recommendations for osteoporosis monitoring and treatment in individuals prescribed antidepressant medications, beyond the usual clinical guidelines. However, treatment of the older depressed person who is at risk of falls provides the opportunity to inquire about his or her adherence with osteoporosis and fracture-prevention guidelines.
Keywords: Antidepressants, depression, falls, fear of falling, fractures
One-third of community-dwelling seniors fall each year, with half of these individuals falling more than once. Ten percent of all falls result in a major injury, which can lead to institutionalization and death.1 Falls often result in a fear of further falls, leading to fear-related restriction of activities: this activity restriction has been associated with subsequent impairment in balance, mobility, and disability.2,3
This clinical review examines falls from the perspective of depression and its treatment, as well as associated anxiety. Like falls, depression is common in old age, with 15% of community-dwelling seniors reporting clinically significant depressive symptoms.4 There is a close relationship between anxiety and depression in old age,5 making it difficult to examine their effects independently. Fear of falling and worries about the consequences of falling are common manifestations of anxiety in older adults and are associated with a variety of avoidance and safety behaviors. This article aims to provide a selected overview of literature most pertinent to the clinician and will highlight gaps in the evidence and areas for future research.
DEPRESSION AND FALLS
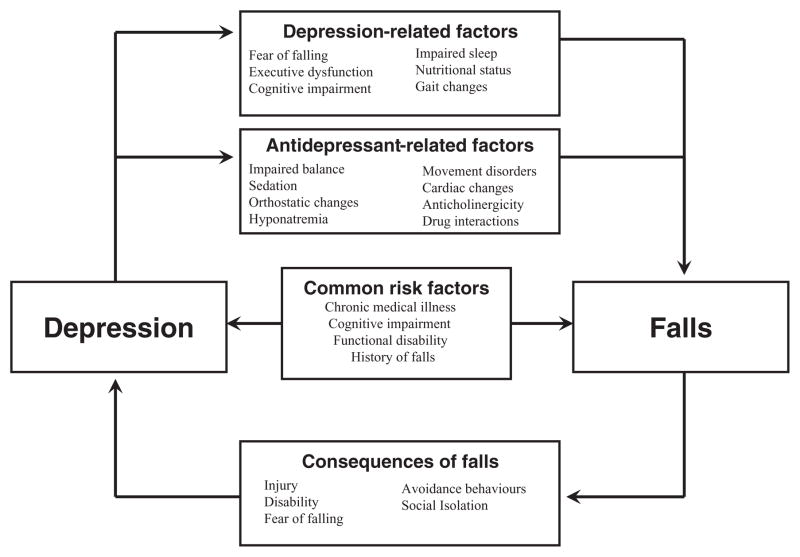
Depression and falls are frequently associated. A recent meta-analysis summarized the findings of 17 prospective studies and found an odds ratio for the association of depression with falls of 1.63 (95% CI: 1.36–1.94).6 The relationship between depression and falls is complex and bidirectional (Figure 1). Depression is an independent risk factor for falls. In one prospective study, there were four determinants of recurrent falls: postural sway, history of falls, handgrip strength, and depressive symptoms.7 Individually, symptoms of depression may have a direct role in promoting falls. Older women with insomnia and sleep fragmentation have an increased risk of falling, even when controlling for the use of sedatives.8 Poor appetite and weight loss are commonly seen in geriatric depression and nutritional deficiencies in vitamin D and folate may be related to falls.9 In addition, cross-sectional studies have identified an association between lower vitamin D levels and symptoms of depression but it is not known whether low vitamin D levels are a cause, consequences, or indirect correlate of depression.10
FIGURE 1.
The association between depression and falls involves factors related to the symptoms of depression, the treatment of depression, and the effect of falls on mood. The interaction is further complicated by common risk factors for falls and depression in older adults.
Depression is also associated with a characteristic pattern of cognitive deficits, affecting mainly attention, executive function, and processing speed.11 Walking is a complex process in which the motor, sensory, and cognitive functions interact. In particular, the cognitive domains of attention and executive function are central to gait performance.12 In general, older adults need to allocate greater attention to walking to compensate for changes in their sensory and motor function. When walking with distractions, depressive symptoms and deficits in executive function are associated with increased unsteadiness.13 Balance-impaired individuals with depression are slower when given a cognitively challenging gait task, and this correlates with measures of executive function.14 Depression is thus associated with neurocognitive changes in the ability to attend to one’s environment and to coordinate motor output.
Psychomotor slowing is a common feature of major depression: related gait disturbances have been found in depression. In particular, individuals with depression walk slowly with a shorter stride length, longer standing phase, and increased gait variability.15,16 These gait patterns characteristic of depression have been shown to be associated with falls.17,18
The complex relationship between depression, cognitive performance, motor performance, and risk of falls is illustrated by a recent study that found that the association between depression and slowed choice stepping reaction time (which is a composite measure of fall risk) was mediated by two paths: one through quadriceps strength and the other through executive function, with both mediating variables then influencing choice stepping reaction time via simple reaction time and balance.19
Depression and falls are also linked indirectly through several common risk factors. Functional decline, history of falls, and cognitive impairment have been separately linked to both depression and falls.20 Poor physical health is also a notable risk factor for both falls and depression. Vascular disease, in particular, and its related burden of white matter lesions, may produce concurrent changes in balance, gait, and mood.21
The interaction between depression and falls may also be self-perpetuating. Depressive symptoms are particularly high in those who are recurrent fallers,22 which may be related to the demoralizing effect of repeated falling. In a prospective study over an 8-year period, increase in depressive symptoms was associated with an increased rate of falls.23 Conversely, a lower rate of falls was associated with improvement in morale scores over the follow-up period.23 Depressive cognitive–affective symptoms seen in repeat fallers include a lower sense of self-efficacy and negative expectations of the future. Activity restriction and decreased social participation can be a complication of recurrent falls24: the resulting social isolation is known to be a significant risk factor for depression in older adults.25
FEAR OF FALLING
Fear and anxiety is another significant cognitive–affective response to falling. Fear of falling can be an expected and adaptive response to having experienced a fall. However, fear of falling can be excessive and disabling, to the point where an individual may be agoraphobic. It is not always easy to distinguish between an adaptive and an unhealthy fear of falling. For example, in a study of hospitalized fallers, only 1 of 48 individuals with moderate to severe fear of falling felt that this fear was excessive or unreasonable, even though the fear frequently resulted in avoidance of activities.26 However, a clear discrepancy between perception of fall risk and objectively determined fall risk (as determined by history of falls, balance and gait performance, lower extremity strength, and physical conditions such as visual impairment and Parkinson’s disease that increase the risk of falls) points to fear of falling as being excessive. Delbaere et al.27 found that community-dwelling residents who had low “physiologic” fall risk but high perceived fall risk were significantly more likely to have depressive symptoms, neurotic personality traits, and impaired executive functioning compared with persons whose perceived risk was congruent with physiologic risk.
The term “fear of falling” is often used interchangeably with low falls self-efficacy. Nevertheless, it is becoming clearer that fear of falling, although related to falls efficacy, is a distinct concept.28 Falls self-efficacy reflects an individual’s cognitive appraisal of his or her abilities and has been found to be related to one’s functional abilities.29 On the other hand, fear of falling is an emotional response that can be measured physiologically in threatening situations30 and is associated with neuroticism and trait anxiety.31,32
Fear of falling is common in community-dwelling seniors, with most studies reporting a prevalence of 25%–50%; about half of those who are fearful will curtail their activities as a result.33,34 The incidence of fear of falling over a 2-year period was found to be 45% in a community sample and was associated with female gender, falls, gait abnormalities, and depressive symptoms35 Fear of falling is persistent, with 80% of affected seniors continuing to report fear of falling over a 3-year follow-up.36
Given the close relationship between depression and anxiety in late life, it is not surprising that depression is closely linked to excessive fear of falling. In hospitalized fallers who had moderate to severe fear of falling, 38% met criteria for a depressive disorder, compared with 4% of those who were not fearful: depressive disorder accounted for more of the explained variance in fear of falling than other known risk factors for this fear.26 Individuals with moderate to severe depressive symptoms are more likely to be severely afraid of falling than those without depression (OR: 2.74; 95% CI: 1.69–4.47).37 Depressive symptoms predict the persistence of fear of falling36 and whether someone will restrict their activity level.34 In a prospective study, activity restriction in the nondepressed was most strongly associated with physical factors such as balance, strength, and vision. In the depressed group, activity restriction was associated only with fear of falling, suggesting that psychological factors were more at play.38
Fear of falling is associated with an increased risk of future falls,39 possibly through an effect on gait and balance. Fearful or cautious gait is a common gait disturbance in older adults. Anxious elders walk more slowly, take shorter strides, have a wider base, and have a longer double limb support time and higher gait variability.40,41 Those who are most concerned about falling tend to make disproportionate adjustments to gait speed in response to postural threat.30 There is some evidence that a slowed gait is maladaptive and reduces, rather than improves, stability.42 Fearful gait may improve when the fearful person feels more secure; for example, handholding, while not offering any objective support of gait, can temporarily decrease fear of falling with simultaneous improvement in gait.43 Balance and postural control are also affected by fear. Abnormal fear-related protective responses take different forms including stiffening and postural over adjustment.44,45 Thus, while a certain amount of caution is appropriate for someone who is fall-prone, there is likely an individual optimal range of arousal and vigilance for falls.
ANTIDEPRESSANTS AND FALLS
Antidepressants are a commonly prescribed medication in older adults, in 9% of community-dwelling seniors to as high as 31% of nursing home residents.46 Their use has been associated with falls. A recent meta-analysis found that the odds ratio of falls with antidepressants was 1.68 (1.47–1.91),47 similar to the risk associated with benzodiazepines and antipsychotics. These data are based on pharmacoepidemiologic studies, which are subject to “confounding by indication,” that is confounding by the clinical condition for which the drug is prescribed. Notwithstanding this important caveat, risk of falls has been reported with tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs);48 other specific antidepressants have not yet been studied. The highest risk of falls appears to be within the first few weeks after initiation of an antidepressant.48 There is little known about whether there are differences between individual medications in the SSRI class and whether there is a dose effect.
Multiple antidepressant-related adverse effects have been implicated in falls (Figure 1). In a study of paroxetine, 38% of subjects fell during the 21-week trial. Orthostatic changes in blood pressure during treatment and memory impairment at baseline were associated with falls.49 Hyponatremia, a common and potentially serious adverse event complicating the use of SSRIs in older adults, has been implicated in fractures in a small case–control study.50 Antidepressants may also directly impair postural control. Increased postural sway was noted in depressed patients in the first week of treatment with sertraline, when compared with nortriptyline and controls.51 However, in a similar study, there was no change in balance over the course of 6 weeks of treatment with paroxetine or nortriptyline.52
From a clinical point of view, it can be difficult to weigh the risk of falls from untreated depression against the risk of falls associated with antidepressant medication. Unfortunately, there are no prospective controlled data available to offer guidance. In a small uncontrolled study, antidepressant treatment after 10 weeks improved both depressive symptoms and gait parameters, including gait speed, variability, asymmetry, and stride length.53 However, this study did not directly assess for gait changes during the higher-risk early treatment period.
DEPRESSION, ANTIDEPRESSANTS, AND FRACTURES
SSRI antidepressants have been found to be associated with fragility fractures, more so than other classes of psychotropic medications.54,55 This association was first observed in a series of case–control studies using large administrative databases54–56 but has since been replicated with prospective cohort studies.57,58 In a multivariate analysis, controlling for such factors as depressive symptoms, falls history, visual and cognitive impairment, comorbidities, postural hypotension, other medications, alcohol and smoking, the risk of fragility fracture over 8 years with current SSRI use was found to be 2.35 (1.3–4.2).57
SSRIs also have been found to have a dose relationship with fractures.54,58 Similar to the risk for falls, the risk of fracture associated with SSRI use is the highest in the first 2 weeks of treatment (OR: 6.30; CI: 2.65–14.97) but remains elevated with continuous antidepressant use beyond the first month of use (OR: 1.32; CI: 1.19–1.48).59 This pattern is in contrast to the risk of fractures with tricyclic antidepressants, which is highest with a new prescription, but decreases significantly with continuous use.56
Older adults are thus at highest risk for falls and fractures shortly after starting an SSRI antidepressant but break bones at a higher rate throughout their treatment. The role of serotonin in bone metabolism may be a mechanism for this long-term association between fractures and SSRI use. Serotonin transporters are known to be present on bone cells, and central serotonin has a role in regulating bone mass through sympathetic outflow.60 In animal studies, the disruption of the serotonin transporter gene decreases bone density, as does administering SSRI medication.61 To date, clinical evidence for an association between SSRIs and bone loss is striking but somewhat inconsistent—while some have observed a significant decrease in bone mineral density in patients taking SSRIs, this has not been confirmed in other large studies.62
As is the case with studies of antidepressants and falls, studies of SSRIs, bone loss, and fractures are subject to “confounding by indication.” Depression itself has been associated with decreased bone mineral density63 and has also been associated with fractures.64 Multiple factors may be involved in the loss of bone density and fractures in depression, including the effects of inactivity, hypercortisolemia, inflammatory processes associated with depression, smoking, and alcohol abuse. Interestingly, the only study to specifically examine the effect of treatment of depression with an SSRI on bone turnover (albeit in premenopausal women) found that improvement in severity of depression was significantly associated with suppression of markers of bone turnover, although whether this finding translates to a reduced risk of fracture is not known.65 Other uses for SSRI antidepressants may also confound this research. In particular, SSRIs are being more frequently used in cognitively impaired and institutionalized older adults,46 presumably for neuropsychiatric symptoms of dementia. Behaviorally disturbed individuals with dementia are at increased risk of fractures.
Fractures themselves are associated with the development of depression. Hip fractures are a particular threat to independence and well-being, leading to institutionalization in 20%–30% and with a 1-year mortality rate of 26%.66 In the period after a hip fracture, 15% of older adults meet criteria for major depression, and half will have elevated depressive symptoms.67 In some individuals, a high level of distress immediately after the injury improves over time.68 In a smaller proportion, depressive symptoms seem to arise as their recovery plateaus and they are faced with enduring deficits.69
Depression is associated with a slower recovery, poorer functional status, and higher levels of disability after a hip fracture. When depressed, persons who have suffered a hip fracture are less likely to participate in rehabilitation activities and recover more slowly.70 Improvement in level of disability during rehabilitation is associated with improved mood.71
Age, medical comorbidity, level of disability before and after the fracture, apathy, delirium, cognitive impairment, and poor social support are all risk factors for the development of depression after hip fracture.67 Use of an antidepressant at baseline, perhaps an indicator of a history of depression, is also a risk factor.67 Gene polymorphisms in serotonin transporter and 5HT-1A receptor, markers of vulnerability to stress, have also been implicated in the development of depression and impaired function after a hip fracture.72,73 The presence of depressive symptoms prefracture may also be a risk factor for loss of functional status.74
DEPRESSION, FEAR OF FALLING, FALLS PREVENTION, AND EXERCISE
Preventative programs for falls are now widespread, often incorporating some or all of the components of falls risk assessment, education, and exercise to improve balance and strength. A recent meta-analysis reported that fall-prevention programs are effective in reducing falls by an average of 14% over at least 5 months of observation.75 An earlier Cochrane Review, however, found significant heterogeneity in the outcomes of falls-prevention interventions, with some randomized controlled trials reporting a 30% reduction in the rate of falls.76
Exercise has been found to have modest short-term benefit in the treatment of mild-moderate depressive disorder, including older individuals.77 However, fall-prevention programs, which usually incorporate an exercise component, have not shown a beneficial effect on depression rating scale scores.78,79 Although clinically significant depressive symptoms are common in community-dwelling fallers, they tend to be less frequent in clinical trials of fall-prevention programs; this may represent a selection bias in individuals presenting to and participating in these programs or studies. Thus, the apparent lack of benefit of fall-prevention programs on depression may be due to the paucity of clinically depressed persons in the studies that have examined this question.78 In addition to a selection bias, there is also the issue of program non-adherence and dropouts; individuals with depression and/or fear of falling are less likely to adhere to a falls or exercise program, and they drop out at a higher rate.80
Cognitive-behavioral approaches tailored to fear of falling have been designed and implemented with some success. Through cognitive restructuring and behavioral changes, these programs aim to reduce fear of falling by improving self-efficacy and the sense of control over falling. This approach has shown improvement in fear of falling and falls efficacy, although mixed results in preventing falls and increasing activity levels.81,82 Unfortunately, there have not been any studies examining the effect of these interventions on concurrent depressive symptoms. Given the fact that antidepressant medications have been associated with an increased risk of falls, and the depression associated with fear of falling is often of mild-moderate severity, further research in psychotherapeutic interventions is warranted.
DEPRESSION AND FALLS: CLINICAL IMPLICATIONS
An overall assessment for falls risk is important when starting psychotropic medication in fall-prone individuals. This would include an assessment of other falls promoting medications, checking for drug interactions, observing gait and tone, and inquiring about falls history. Given that most falls occur early in treatment and may potentially be dose-related, SSRI medications should be started at a low dose and increased slowly in older adults to minimize their effect on falls. Cognitive impairment, orthostatic hypotension, extrapyramidal effects, and hyponatremia should be monitored during treatment. Given the possibility of skeletal changes with long-term use of SSRIs, it is important for the risk–benefit of antidepressant treatment to be evaluated on an ongoing basis.
To date, there have been no recommendations for osteoporosis monitoring and treatment in individuals prescribed SSRI medications beyond the usual clinical guidelines. However, individuals with depression make less use of preventative services.83 No studies have specifically looked at adherence to osteoporosis screening and treatment in depressed older adults. When prescribing an SSRI, it is therefore useful to inquire about the older patient’s adherence with osteoporosis and fracture-prevention guidelines. These vary internationally but tend to include a recommendation for screening dual-energy x-ray absorptiometry in those older than 65 years, the use of bisphosphonates in individuals with diagnosed osteopenia or osteoporosis, and repeat dual-energy x-ray absorptiometry scans every 2 years.84 Recommended lifestyle modifications include adequate elemental calcium (1000 mg/day) and vitamin D (400–800 IU/day), for which supplements are often required, stopping smoking, decreasing caffeine intake, and regular weight-bearing exercise.
FUTURE DIRECTIONS
As this review indicates, research evidence suggests that both depression and antidepressant medication are associated with falls and fractures. Moreover, while exercise and cognitive–behavioral therapy have benefit in treating mild-moderate depression in the general older adult population, there are currently no data pertaining to the efficacy and feasibility of these interventions in persons who both are at high risk of falls and are clinically depressed. Thus, clinicians currently find themselves between Scylla and Charybdis in deciding on the optimal management of this group of patients. Confounding biases are arguably the main limitation in interpreting pharmacoepidemiologic data pertaining to the contribution of antidepressant medication to falls and fractures. It is unlikely that adequately powered randomized controlled trials that are specifically focused on the use of antidepressants in persons at high risk of falls will be conducted. We believe that incorporating falls as an adverse outcome into clinical trials that study antidepressants in older persons should be standard practice, but biases in the types of patients selected for these studies (which typically focus on cognitively intact, medically stable, young-old patients without comorbid neurologic conditions) will likely mean that the risk of falls will be low. A more feasible line of research will be to examine the effect of antidepressants on sophisticated measures that are valid “markers” for increased risk of falls and fractures, in well-designed RCTs that not only account for potential confounding variables but also explore the interaction between the antidepressant and these variables. This line of research should examine not only whether antidepressant use per se independently predicts risk of falls and fractures but also whether and how the method of use of antidepressants, such as starting dose, speed of dose titration, and concomitant use of anxiolytics and hypnotics in the early stage of treatment, affects the risk of falls.
There is also a need for research in nonpharmacologic interventions. Given that the presence of a depressive disorder and/or severe fear of falling may interfere with a person attending a falls-prevention program, cost-effective home-based interventions for depressed and anxious older fallers warrant investigation. There is also the need to determine whether the presence of clinically significant depressive symptoms has a moderating effect on the treatment of fear of falling and whether depression contributes to persistence in fear of falling, despite improvement in falls efficacy.
TABLE 1.
Practice Points
| Depression and fear of falling are independent risk factors for falls, each mediated through multifactorial pathways. |
| Antidepressant medications are associated with a 70% increased risk of falls; SSRIs are associated with risk of fractures. These findings are, however, limited by the possibility of confounding biases, such as the reason for initiation of the antidepressant. |
| Antidepressant medications are indicated to treat moderate to severe depression in fallers, but be wary of the potential increased risk of falls and prescribe accordingly (e.g., low starting dose, gradual titration, avoid more than one psychotropic at a time whenever possible, monitor orthostatic blood pressure and serum sodium). |
| Consider exercise, particularly Tai Chi, and cognitive–behavioral therapy for the first-line treatment of mild depression in older fallers. |
| When treating the older depressed patient, inquire about his or her adherence with osteoporosis and fracture-prevention guidelines. |
Acknowledgments
This study was supported by Canadian Institutes of Health Research and a grant from the Department of Psychiatry, University Health Network.
Footnotes
Financial disclosures: Dr. Iaboni does not have financial disclosures to report. Dr. Flint: honoraria from Lund-beck Canada and Pfizer Canada.
References
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 2.Deshpande N, Metter EJ, Lauretani F, et al. Activity restriction induced by fear of falling and objective and subjective measures of physical function: a prospective cohort study. J Am Geriatr Soc. 2008;56:615–620. doi: 10.1111/j.1532-5415.2007.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol. 1991;46:M123–M131. doi: 10.1093/geronj/46.4.m123. [DOI] [PubMed] [Google Scholar]
- 4.Beekman AT, Deeg DJ, van Tilburg T, et al. Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord. 1995;36:65–75. doi: 10.1016/0165-0327(95)00061-5. [DOI] [PubMed] [Google Scholar]
- 5.Beekman ATF, De Beurs E, Van Balkom AJLM, et al. Anxiety and depression in later life: co-occurrence and communality of risk factors. Am J Psychiatry. 2000;157:89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- 6.Deandrea S, Lucenteforte E, Bravi F, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–668. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 7.Stalenhoef PA, Diederiks JPM, Knottnerus JA, et al. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55:1088–1094. doi: 10.1016/s0895-4356(02)00502-4. [DOI] [PubMed] [Google Scholar]
- 8.Stone KL, Ancoli-Israel S, Blackwell T, et al. Actigraphy-measured sleep characteristics and risk of falls in older women. Arch Intern Med. 2008;168:1768–1775. doi: 10.1001/archinte.168.16.1768. [DOI] [PubMed] [Google Scholar]
- 9.Shahar D, Levi M, Kurtz I, et al. Nutritional status in relation to balance and falls in the elderly: a preliminary look at serum folate. Ann Nutr Metab. 2009;54:59–66. doi: 10.1159/000207356. [DOI] [PubMed] [Google Scholar]
- 10.Parker G, Brotchie H. D for depression: any role for vitamin D? Acta Psychiatr Scand. 2011;124:243–249. doi: 10.1111/j.1600-0447.2011.01705.x. [DOI] [PubMed] [Google Scholar]
- 11.McDermott LM, Ebmeier KP. A meta-analysis of depression severity and cognitive function. J Affect Disord. 2009;119:1–8. doi: 10.1016/j.jad.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 12.Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23:329–342. doi: 10.1002/mds.21720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hausdorff JM, Schweiger A, Herman T, et al. Dual-task decrements in gait: contributing factors among healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63:1335–1343. doi: 10.1093/gerona/63.12.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright SL, Kay RE, Avery ET, et al. The impact of depression on dual tasking among patients with high fall risk. J Geriatr Psychiatry Neurol. 2011;24(3):142–150. doi: 10.1177/0891988711409408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michalak J, Troje NF, Fischer J, et al. Embodiment of sadness and depression—gait patterns associated with dysphoric mood. Psychosom Med. 2009;71:580–587. doi: 10.1097/PSY.0b013e3181a2515c. [DOI] [PubMed] [Google Scholar]
- 16.Hausdorff JM, Peng CK, Goldberger AL, et al. Gait unsteadiness and fall risk in two affective disorders: a preliminary study. BMC Psychiatry. 2004;4:39. doi: 10.1186/1471-244X-4-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 18.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45:313–320. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 19.Kvelde T, Pijnappels M, Delbaere K, et al. Physiological and cognitive mediators for the association between self-reported depressed mood and impaired choice stepping reaction time in older people. J Gerontol A Biol Sci Med Sci. 2010;65:538–544. doi: 10.1093/gerona/glp195. [DOI] [PubMed] [Google Scholar]
- 20.Biderman A, Cwikel J, Fried AV, et al. Depression and falls among community dwelling elderly people: a search for common risk factors. J Epidemiol Community Health. 2002;56:631–636. doi: 10.1136/jech.56.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hajjar I, Yang F, Sorond F, et al. A novel aging phenotype of slow gait, impaired executive function, and depressive symptoms: relationship to blood pressure and other cardiovascular risks. J Gerontol A Biol Sci Med Sci. 2009;64:994–1001. doi: 10.1093/gerona/glp075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Somadder M, Mondal S, Kersh R, et al. Are recurrent fallers depressed? J Am Geriatr Soc. 2007;55:2097–2099. doi: 10.1111/j.1532-5415.2007.01449.x. [DOI] [PubMed] [Google Scholar]
- 23.Anstey KJ, Burns R, von Sanden C, et al. Psychological well-being is an independent predictor of falling in an 8-year follow-up of older adults. J Gerontol B Psychol Sci Soc Sci. 2008;63:P249–P257. doi: 10.1093/geronb/63.4.p249. [DOI] [PubMed] [Google Scholar]
- 24.Miller RR, Ballew SH, Shardell MD, et al. Repeat falls and the recovery of social participation in the year post–hip fracture. Age Ageing. 2009;38:570–575. doi: 10.1093/ageing/afp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vink D, Aartsen MJ, Schoevers RA. Risk factors for anxiety and depression in the elderly: a review. J Affect Disord. 2008;106:29–44. doi: 10.1016/j.jad.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Gagnon N, Flint AJ, Naglie G, et al. Affective correlates of fear of falling in elderly persons. Am J Geriatr Psychiatry. 2005;13:7–14. doi: 10.1176/appi.ajgp.13.1.7. [DOI] [PubMed] [Google Scholar]
- 27.Delbaere K, Close JCT, Brodaty H, et al. Determinants of disparities between perceived and physiological risk of falling among elderly people: Cohort study. BMJ. 2010;341:c4165. doi: 10.1136/bmj.c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health. 2011;23:3–23. doi: 10.1177/0898264310378039. [DOI] [PubMed] [Google Scholar]
- 29.Tinetti ME, Mendes de Leon CF, Doucette JT, et al. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol. 1994;49:M140–M147. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 30.Delbaere K, Sturnieks DL, Crombez G, et al. Concern about falls elicits changes in gait parameters in conditions of postural threat in older people. J Gerontol A Biol Sci Med Sci. 2009;64:237–242. doi: 10.1093/gerona/gln014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharaf AY, Ibrahim HS. Physical and psychosocial correlates of fear of falling: among older adults in assisted living facilities. J Gerontol Nurs. 2008;34:27–35. doi: 10.3928/00989134-20081201-07. [DOI] [PubMed] [Google Scholar]
- 32.Mann R, Birks Y, Hall J, et al. Exploring the relationship between fear of falling and neuroticism: a cross-sectional study in community-dwelling women over 70. Age Ageing. 2006;35:143–147. doi: 10.1093/ageing/afj013. [DOI] [PubMed] [Google Scholar]
- 33.Howland J, Lachman ME, Peterson EW, et al. Covariates of fear of falling and associated activity curtailment. Gerontologist. 1998;38:549–555. doi: 10.1093/geront/38.5.549. [DOI] [PubMed] [Google Scholar]
- 34.Murphy SL, Williams CS, Gill TM. Characteristics associated with fear of falling and activity restriction in community-living older persons. J Am Geriatr Soc. 2002;50:516–520. doi: 10.1046/j.1532-5415.2002.50119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oh-Park M, Xue X, Holtzer R, et al. Transient versus persistent fear of falling in community-dwelling older adults: incidence and risk factors. J Am Geriatr Soc. 2011;59(7):1225–1231. doi: 10.1111/j.1532-5415.2011.03475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Austin N, Devine A, Dick I, et al. Fear of falling in older women: a longitudinal study of incidence, persistence, and predictors. J Am Geriatr Soc. 2007;55:1598–1603. doi: 10.1111/j.1532-5415.2007.01317.x. [DOI] [PubMed] [Google Scholar]
- 37.van Haastregt JC, Zijlstra GA, van Rossum E, et al. Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. Am J Geriatr Psychiatry. 2008;16:186–193. doi: 10.1097/JGP.0b013e3181591c1e. [DOI] [PubMed] [Google Scholar]
- 38.Deshpande N, Metter EJ, Bandinelli S, et al. Psychological, physical, and sensory correlates of fear of falling and consequent activity restriction in the elderly: the InCHIANTI study. Am J Phys Med Rehabil. 2008;87:354–362. doi: 10.1097/PHM.0b013e31815e6e9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Friedman SM, Munoz B, West SK, et al. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 40.Rochat S, Büla CJ, Martin E, et al. What is the relationship between fear of falling and gait in well-functioning older persons aged 65 to 70 years? Arch Phys Med Rehabil. 2010;91:879–884. doi: 10.1016/j.apmr.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 41.Chamberlin ME, Fulwider BD, Sanders SL, et al. Does fear of falling influence spatial and temporal gait parameters in elderly persons beyond changes associated with normal aging? J Gerontol A Biol Sci Med Sci. 2005;60:1163–1167. doi: 10.1093/gerona/60.9.1163. [DOI] [PubMed] [Google Scholar]
- 42.Menz HB, Lord SR, Fitzpatrick RC. A structural equation model relating impaired sensorimotor function, fear of falling and gait patterns in older people. Gait Posture. 2007;25:243–249. doi: 10.1016/j.gaitpost.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 43.Balash Y, Hadar-Frumer M, Herman T, et al. The effects of reducing fear of falling on locomotion in older adults with a higher level gait disorder. J Neural Transm. 2007;114:1309–1314. doi: 10.1007/s00702-007-0771-z. [DOI] [PubMed] [Google Scholar]
- 44.Nagai K, Yamada M, Uemura K, et al. Effects of the fear of falling on muscular coactivation during walking. Aging Clin Exp Res. 2011 doi: 10.3275/7716. [DOI] [PubMed] [Google Scholar]
- 45.Davis JR, Campbell AD, Adkin AL, et al. The relationship between fear of falling and human postural control. Gait Posture. 2009;29:275–279. doi: 10.1016/j.gaitpost.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 46.Karkare SU, Bhattacharjee S, Kamble P, et al. Prevalence and predictors of antidepressant prescribing in nursing home residents in the United States. Am J Geriatr Pharmacother. 2011;9:109–119. doi: 10.1016/j.amjopharm.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 47.Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 48.Thapa PB, Gideon P, Cost TW, et al. Antidepressants and the risk of falls among nursing home residents. N Engl J Med. 1998;339:875–882. doi: 10.1056/NEJM199809243391303. [DOI] [PubMed] [Google Scholar]
- 49.Joo JH, Lenze EJ, Mulsant BH, et al. Risk factors for falls during treatment of late-life depression. J Clin Psychiatry. 2002;63:936–941. doi: 10.4088/jcp.v63n1012. [DOI] [PubMed] [Google Scholar]
- 50.Sandhu HS, Gilles E, DeVita MV, et al. Hyponatremia associated with large-bone fracture in elderly patients. Int Urol Nephrol. 2009;41:733–737. doi: 10.1007/s11255-009-9585-2. [DOI] [PubMed] [Google Scholar]
- 51.Laghrissi-Thode F, Pollock BG, Miller M, et al. Comparative effects of sertraline and nortriptyline on body sway in older depressed patients. Am J Geriatr Psychiatry. 1995;3:217–228. doi: 10.1097/00019442-199522330-00005. [DOI] [PubMed] [Google Scholar]
- 52.Mamo DC, Pollock BG, Mulsant B, et al. Effects of nortriptyline and paroxetine on postural sway in depressed elderly patients. Am J Geriatr Psychiatry. 2002;10:199–205. [PubMed] [Google Scholar]
- 53.Paleacu D, Shutzman A, Giladi N, et al. Effects of pharmacological therapy on gait and cognitive function in depressed patients. Clin Neuropharmacol. 2007;30:63–71. doi: 10.1097/01.wnf.0000240949.41691.95. [DOI] [PubMed] [Google Scholar]
- 54.Bolton JM, Metge C, Lix L, et al. Fracture risk from psychotropic medications: a population-based analysis. J Clin Psychopharmacol. 2008;28:384–391. doi: 10.1097/JCP.0b013e31817d5943. [DOI] [PubMed] [Google Scholar]
- 55.Vestergaard P, Rejnmark L, Mosekilde L. Selective serotonin reup-take inhibitors and other antidepressants and risk of fracture. Calcif Tissue Int. 2008;82:92–101. doi: 10.1007/s00223-007-9099-9. [DOI] [PubMed] [Google Scholar]
- 56.Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors of tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351:1303–1307. doi: 10.1016/s0140-6736(97)09528-7. [DOI] [PubMed] [Google Scholar]
- 57.Ziere G, Dieleman JP, van der Cammen TJ, et al. Selective serotonin reuptake inhibiting antidepressants are associated with an increased risk of nonvertebral fractures. J Clin Psychopharmacol. 2008;28:411–417. doi: 10.1097/JCP.0b013e31817e0ecb. [DOI] [PubMed] [Google Scholar]
- 58.Richards JB, Papaioannou A, Adachi JD, et al. Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med. 2007;167:188–194. doi: 10.1001/archinte.167.2.188. [DOI] [PubMed] [Google Scholar]
- 59.Hubbard R, Farrington P, Smith C, et al. Exposure to tricyclic and selective serotonin reuptake inhibitor antidepressants and the risk of hip fracture. Am J Epidemiol. 2003;158:77–84. doi: 10.1093/aje/kwg114. [DOI] [PubMed] [Google Scholar]
- 60.Rosen CJ. Bone: serotonin, leptin and the central control of bone remodeling. Nat Rev Rheumatol. 2009;5:657–658. doi: 10.1038/nrrheum.2009.231. [DOI] [PubMed] [Google Scholar]
- 61.Warden SJ, Haney EM. Skeletal effects of serotonin (5-hydroxytryptamine) transporter inhibition: evidence from in vitro and animal-based studies. J Musculoskelet Neuronal Interact. 2008;8:121–132. [PMC free article] [PubMed] [Google Scholar]
- 62.Haney EM, Warden SJ, Bliziotes MM. Effects of selective serotonin reuptake inhibitors on bone health in adults: time for recommendations about screening, prevention and management? Bone. 2010;46:13–17. doi: 10.1016/j.bone.2009.07.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yirmiya R, Bab I. Major depression is a risk factor for low bone mineral density: a meta-analysis. Biol Psychiatry. 2009;66:423–432. doi: 10.1016/j.biopsych.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 64.Spangler L, Scholes D, Brunner RL, et al. Depressive symptoms, bone loss, and fractures in postmenopausal women. J Gen Intern Med. 2008;23:567–574. doi: 10.1007/s11606-008-0525-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aydin H, Mutlu N, Akbas NB. Treatment of a major depression episode suppresses markers of bone turnover in premenopausal women. J Psychiatr Res. 2011;45:1316–1320. doi: 10.1016/j.jpsychires.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 66.Bentler SE, Liu L, Obrizan M, et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol. 2009;170:1290–1299. doi: 10.1093/aje/kwp266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lenze EJ, Munin MC, Skidmore ER, et al. Onset of depression in elderly persons after hip fracture: implications for prevention and early intervention of late-life depression. J Am Geriatr Soc. 2007;55:81–86. doi: 10.1111/j.1532-5415.2006.01017.x. [DOI] [PubMed] [Google Scholar]
- 68.Mossey JM, Knott K, Craik R. The effects of persistent depressive symptoms on hip fracture recovery. J Gerontol. 1990;45:M163–M168. doi: 10.1093/geronj/45.5.m163. [DOI] [PubMed] [Google Scholar]
- 69.Scaf-Klomp W, Sanderman R, Ormel J, et al. Depression in older people after fall-related injuries: a prospective study. Age Ageing. 2003;32:88–94. doi: 10.1093/ageing/32.1.88. [DOI] [PubMed] [Google Scholar]
- 70.Lenze EJ, Munin MC, Dew MA, et al. Adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture. Int J Geriatr Psychiatry. 2004;19:472–478. doi: 10.1002/gps.1116. [DOI] [PubMed] [Google Scholar]
- 71.Barbisoni P, Bertozzi B, Franzoni S, et al. Mood improvement in elderly women after in-hospital physical rehabilitation. Arch Phys Med Rehabil. 1996;77:346–349. doi: 10.1016/s0003-9993(96)90082-9. [DOI] [PubMed] [Google Scholar]
- 72.Lenze EJ, Shardell M, Ferrell RE, et al. Association of serotonin-1A and 2A receptor promoter polymorphisms with depressive symptoms and functional recovery in elderly persons after hip fracture. J Affect Disord. 2008;111:61–66. doi: 10.1016/j.jad.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lenze EJ, Munin MC, Ferrell RE, et al. Association of the serotonin transporter gene-linked polymorphic region (5-HTTLPR) genotype with depression in elderly persons after hip fracture. Am J Geriatr Psychiatry. 2005;13:428–432. doi: 10.1176/appi.ajgp.13.5.428. [DOI] [PubMed] [Google Scholar]
- 74.Ostir GV, Goodwin JS, Markides KS, et al. Differential effects of premorbid physical and emotional health on recovery from acute events. J Am Geriatr Soc. 2002;50:713–718. doi: 10.1046/j.1532-5415.2002.50167.x. [DOI] [PubMed] [Google Scholar]
- 75.Choi M, Hector M. Effectiveness of intervention programs in preventing falls: a systematic review of recent 10 years and meta-analysis. J Am Med Dir Assoc. 2012;13(2):188, e13–e21. doi: 10.1016/j.jamda.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 76.Gillespie LD, Gillespoe WJ, Robertson MC, et al. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003;(4):CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 77.Krogh J, Nordentoft M, Sterne JAC, et al. The effect of exercise in clinically depressed adults: systematic review and meta-analysis of randomized controlled trials. J Clin Psychiatry. 2011;72:529–538. doi: 10.4088/JCP.08r04913blu. [DOI] [PubMed] [Google Scholar]
- 78.Sjosten N, Vaapio S, Kivela SL. The effects of fall prevention trials on depressive symptoms and fear of falling among the aged: a systematic review. Aging Ment Health. 2008;12:30–46. doi: 10.1080/13607860701366079. [DOI] [PubMed] [Google Scholar]
- 79.Vind AB, Andersen HE, Pedersen KD, et al. Effect of a program of multifactorial fall prevention on health-related quality of life, functional ability, fear of falling and psychological well-being. A randomized controlled trial. Aging Clin Exp Res. 2010;22:249–254. doi: 10.1007/BF03324804. [DOI] [PubMed] [Google Scholar]
- 80.Sjösten NM, Salonoja M, Piirtola M, et al. A multifactorial fall prevention programme in the community-dwelling aged: predictors of adherence. Eur J Public Health. 2007;17:464–470. doi: 10.1093/eurpub/ckl272. [DOI] [PubMed] [Google Scholar]
- 81.Zijlstra GA, van Haastregt JC, Ambergen T, et al. Effects of a multicomponent cognitive behavioral group intervention on fear of falling and activity avoidance in community-dwelling older adults: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57:2020–2028. doi: 10.1111/j.1532-5415.2009.02489.x. [DOI] [PubMed] [Google Scholar]
- 82.Tennstedt S, Howland J, Lachman M, et al. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci Soc Sci. 1998;53:P384–P392. doi: 10.1093/geronb/53b.6.p384. [DOI] [PubMed] [Google Scholar]
- 83.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2009;194:491–499. doi: 10.1192/bjp.bp.107.045732. [DOI] [PubMed] [Google Scholar]
- 84.Cheung AM, Feig DS, Kapral M, et al. Prevention of osteoporosis and osteoporotic fractures in postmenopausal women: recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2004;170:1665–1667. doi: 10.1503/cmaj.1030757. [DOI] [PMC free article] [PubMed] [Google Scholar]