Abstract
Aims
Most programs specializing in the treatment of first-episode psychosis in the United States focus on schizophrenia. However, many early psychosis patients do not fit into this diagnostic category. Here we describe McLean OnTrack, an intensive outpatient treatment program that accepts all-comers with first-episode psychosis.
Methods
We assessed baseline characteristics of patients in the 2.5 years since program initiation. We examined how initial referral diagnoses compare to current diagnoses, calculating the proportion of diagnostic changes.
Results
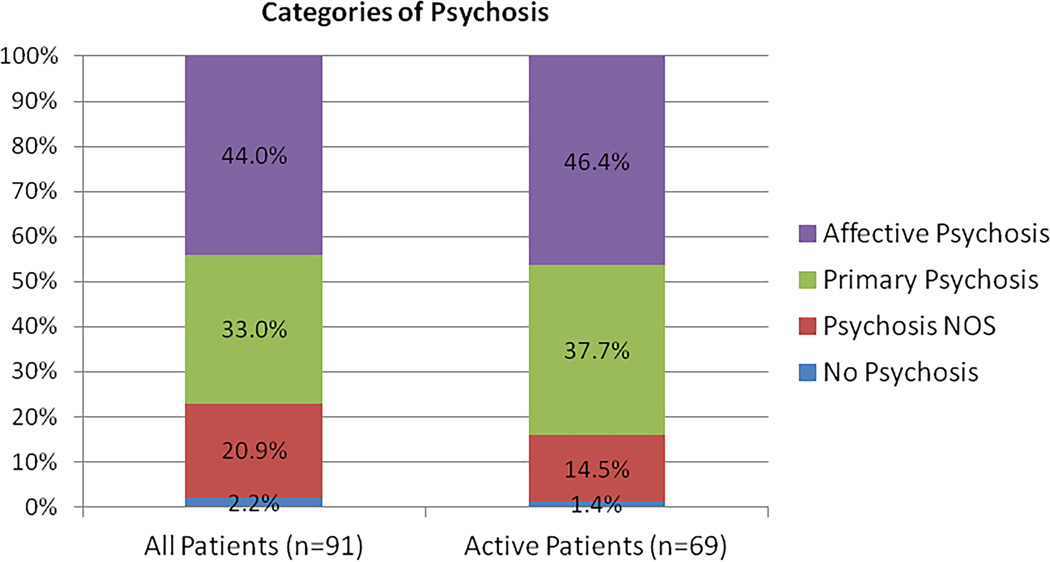
At 2.5 years, patients in McLean OnTrack consist of 30 (33.0%) individuals with primary psychotic disorder, 40 (44.0%) with affective psychosis, 19 (20.9%) with psychotic disorder NOS who do not meet full criteria for either category, and two (2.2%) individuals with no psychosis. While patients with affective psychosis had higher pre-morbid functioning, all three categories of psychosis had similar rates of prior hospitalizations and substance use. The retention rate in the psychotic disorder NOS group was lower than that in affective and primary psychotic disorders. Finally, diagnoses changed over the course of treatment in 50.5% of patients.
Conclusions
Diagnostic heterogeneity appears to be the norm among patients with first-episode psychosis, and diagnoses commonly evolve over the illness course. Baseline indices of illness severity were similar across categories and suggest the need for early intervention, irrespective of specific diagnosis. We discuss the benefits and challenges of a trans-diagnostic approach to early intervention in first episode psychosis, treating patients who share many but not all characteristics.
Keywords: Psychosis, first-episode, dimensional, trans-diagnostic, treatment
1. Introduction
The initial years following a first episode of psychosis are a critical period for intervention, when the greatest impact can be made to change the trajectory of illness and reduce the risk of long-term disability1–10. In the United States, much of the effort to date on treating early stages of psychotic disorders has focused on primary psychotic disorders such as schizophrenia e.g., 11, 12. Schizophrenia and bipolar disorder are usually treated in different specialty clinics that are staffed by different sets of clinicians, and most "first-episode" programs focus primarily, or even solely, on schizophrenia. Patients who do not fit neatly into the schizophrenia category might be turned away from such first-episode programs. And yet, most patients present with an unclear clinical picture during the initial episode, with varying degrees of mood and psychosis symptoms. Moreover, diagnostic shifts, whether due to changes in the illness course or misclassification, are not uncommon13, 14. First-episode patients may be diagnosed with affective psychosis (bipolar disorder or major depressive disorder with psychotic features) early in illness and diagnosed with schizophrenia spectrum disorders later. Similarly, patients initially suspected to have schizophrenia may later be diagnosed with other disorders. Others present with a mixed picture consistent neither with schizophrenia spectrum disorders nor with affective psychosis.
A common assumption is that full inter-episode recovery and less functional disability occur in affective disorders compared to schizophrenia. However, schizophrenia and affective psychotic disorders are likely not discrete entities but disorders that occur on a continuum15. While outcomes following a first episode of affective psychosis might be more variable than in schizophrenia, a growing body of evidence suggests that the clinical course of bipolar disorder is often cumulative and potentially deteriorating16, 17, not unlike that of schizophrenia. In particular, a larger number of episodes is associated with poorer social adjustment, greater hospitalizations, decreased treatment response, higher suicide rates, more substance abuse, greater cognitive impairments, progressive structural brain changes, and reduced quality of life18, 19. Early intervention after a first episode of mania is necessary to modify these risks and improve the trajectory of illness20–23. These studies suggest that all patients with first-episode psychosis, not just those with schizophrenia, stand to benefit from early intervention1–3. Moreover, the frequency of diagnostic shifts suggests that early intervention programs may serve patients more effectively by tailoring programs to presence or absence of symptom clusters, which are likely to evolve over the course of the illness, rather than on diagnosis per se.
Here, we describe a trans-diagnostic program for early intervention in psychotic illness, and report on our experiences in working with diagnostic heterogeneity and shifts over the life of the program. Our goals are to provide a brief overview of the clinic’s treatment philosophy and services, report baseline characteristics of our clinic sample, and determine the rates of change between referral diagnoses and active diagnoses, which if elevated would lend further support to the trans-diagnostic approach to early intervention in our patients.
The McLean OnTrackTM Program (abbreviated OnTrack), launched in spring 2012, is an outpatient early intervention program that treats individuals with first-episode psychosis across diagnostic categories. With the goal of taking a trans-diagnostic approach, OnTrack accepts young adults, ages 18–30 years, who have experienced new onset psychosis, with or without mood symptoms, within the past twelve months, including those with prominent mania or depression. The name “OnTrack” underscores the program’s emphasis on functional recovery. The program emphasizes hopefulness and shared decision-making, with the view that empowering young people to act as primary and active stakeholders in their care will improve their chances for a robust and sustained recovery. Recognizing that disease course is dynamic, treatment plans are formulated around the evolving needs of each patient, incorporating best practices for first-episode psychosis. The program is embedded within McLean Hospital in Belmont, Massachusetts, an academic, tertiary-care psychiatric hospital with access to state-of-the-art clinical and research resources, enabling clinicians to collaborate and consult with experts from other disciplines. Reflecting discussions in the literature, the optimal duration of treatment continues to be an active area of discussion in OnTrack.
Since patients in OnTrack are heterogeneous and have different needs, the combination and intensity of services delivered depends on individual circumstances. We offer evidence-based pharmacological treatment, individual psychotherapy, group psychotherapy, community-based care, and family support programs. Since syndromal recovery is not strongly correlated with functional recovery and medications for psychosis symptoms may not necessarily enhance functioning24, we do not aim for complete eradication of symptoms and treat using the lowest effective doses of medications. To engage young people in the process of creating meaning in their lives, we use multiple psychotherapeutic approaches, including less structured activities such as nature walks, expressive art therapies25, and self-narrative oriented psychotherapy26, as well as manualized psychotherapies such as cognitive behavioral therapy (CBT)27, personal therapy28, individual resiliency training (IRT)12, and interpersonal and social rhythm therapy (IPSRT)29. While many of these psychotherapies were originally designed for patients with schizophrenia, studies suggest that early psychosocial intervention is also critical for improved functional recovery in first-episode mania30, and we are adapting many of these treatments to address varying needs along the full spectrum of psychosis. For individuals with difficulty participating in traditional outpatient settings, a community-based social worker meets with patients and families in their homes or at school, and also assists with activities such as applying for jobs or navigating meetings with school administrators. Finally, we support caregivers and incorporate them as an essential part of the treatment team, providing guidance, support, and psychoeducation, both individually and in a group setting.
2. Methods
We report on clinical and demographic characteristics of patients enrolled in OnTrack during the first 2.5 years. We provide data on all patients seen in the clinic, as well as those actively receiving treatment in OnTrack as of January 21, 2015. We considered a patient to be active if they received any component of treatment at OnTrack within the prior three months.
We also explore clinical and demographic characteristics by category of psychosis [affective psychosis, primary psychotic disorder, psychotic disorder not otherwise specified (NOS), and no psychosis], providing age, duration of treatment in the program, referral source, hospitalization history, history of pre-morbid substance use disorders (SUD), and pre-morbid functional status (whether a patient was working or attending school prior to program entry). Patients were categorized on the basis of their current diagnoses as of January 21, 2015, extracted from OnTrack medical records. Lastly, we report on the initial referral diagnoses and the evolution of provisional diagnoses during treatment. We obtained referral diagnoses from medical records and intake paperwork completed by referring clinicians and/or family members.
3. Results
3.1. Baseline demographic and clinical characteristics
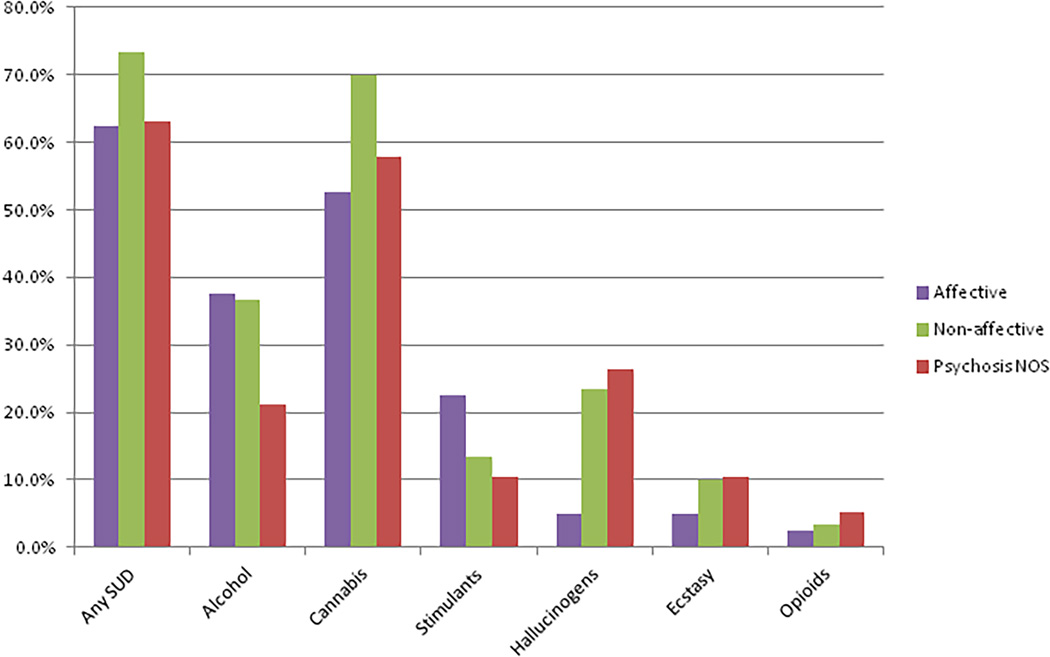
Table 1 provides baseline demographic characteristics of OnTrack patients. The “all-enrolled” and “active-only” groups are similar in diagnostic composition (Figure 1). Table 2 provides demographic and clinical characteristics by category of psychosis. The majority of patients are male and affective psychosis makes up the largest proportion of patients. The majority of patients (64.8%) have a comorbid SUD at intake, with cannabis being the most common abused substance (Figure 2). More than half of our patients (60.4%) were enrolled in school when they experienced their first episode. Most patients were referred from hospitals and had an average of 1.6 hospitalizations prior to program entry.
Table 1.
McLean OnTrack Patient Characteristics
| All patients | Active patients | |
|---|---|---|
| Total, no. (%) | 91 (100%) | 69 (75.8%) |
| Females, no. (%) | 15 (16.5%) | 8 (11.6%) |
| Age | ||
| At entry, mean ± SD (range) (y) | 21.4 ± 3.3 (16–34) | 21.7 ± 3.4 (16–34) |
| Current, mean ± SD (range) (y) | 23.1 ± 3.4 (17–36) | 23.2 ± 3.5 (17–36) |
| Duration in OnTrack, mean ± SD (range) (m) | 11.1 ± 9.6 (0–32.6) | 13.1 ± 9.7 (0–32.6) |
| Affective psychosis | 40 (44.0%) | 32 (46.4%) |
| BP with psychotic features, no. (%) | 36 (39.6%) | 28 (40.6%) |
| MDD with psychotic features, no. (%) | 4 (4.4%) | 4 (5.8 %) |
| Primary psychotic disorders | 30 (33.0%) | 26 (37.7%) |
| Schizophrenia, no. (%) | 14 (15.4%) | 12 (17.4%) |
| Schizoaffective disorder, no. (%) | 16 (17.6%) | 14 (20.3%) |
| Psychotic disorder, NOS | 19 (20.9%) | 10 (14.5%) |
| Atypical, no. (%) | 5 (5.5%) | 3 (4.4%) |
| Unclear/ill-defined, no. (%) | 14 (15.4%) | 7 (10.1%) |
| Other (no history of psychosis) | 2 (2.2%) | 1 (1.5%) |
| Adjustment disorder, no. (%) | 1 (1.1%) | 0 (0%) |
| Mood disorder, NOS, no. (%) | 1 (1.1%) | 1 (1.5%) |
BP = bipolar disorder, MDD = major depressive disorder, NOS = not otherwise specified.
Figure 1.
Categories of psychosis in McLean OnTrack. The diagnostic compositions in the "all-enrolled" and "active-only" groups are similar.
Table 2.
Patient Characteristics by Category of Psychosis
| All patients | Affective | Primary Psychotic | Psychosis NOS | No psychosis | |
|---|---|---|---|---|---|
| Total admitted, no. (% of total, n=92) | 91 (100%) | 40 (44.0%) | 30 (33.0%) | 19 (20.9%) | 2 (2.2%) |
| Active, no. (% of psychosis category) | 69 | 32 (46.4%) | 26 (37.7%) | 10 (14.5%) | 1 (1.5%) |
| Females, no. (% of psychosis category) | 15 | 9 (22.5%) | 2 (6.7%) | 4 (21.1%) | 0 (0%) |
| Age at entry, mean ± SD (y) | 21.4 ± 3.3 | 21.9 ± 2.8 | 21.5 ± 4.1 | 20.7 ± 2.3 | 16.5 ± 0.7 |
| Current age, mean ± SD (y) | 23.1 ± 3.4 | 23.6 ± 2.7 | 23.2 ± 4.4 | 22.4 ± 2.7 | 19.2 ± 1.1 |
| Duration (t) in OnTrack, mean ± SD (m) | 11.1 ± 9.6 | 11.9 ± 9.6 | 14.2 ± 9.2 | 4.2 ± 5.6 | 15.5 ± 17.5 |
| Total possible duration, mean ± SD (m) | 15.0 ± 10.3 | 15.3 ± 10.4 | 15.2 ± 8.7 | 13.0 ± 12.2 | 27.9 ± 0.4 |
| Proportional duration, mean ± SD | 0.81 ± 0.35 | 0.85 ± 0.31 | 0.90 ± 0.27 | 0.62 ± 0.44 | 0.56 ± 0.62 |
| Pre-morbid substance use disorders (SUD) | |||||
| No. of SUD’s, mean ± SD (range) | 1.4 ± 1.5 (0–6) | 1.3 ± 1.3 (0–5) | 1.6 ± 1.5 (0–6) | 1.4 ± 1.7 (0–6) | 0 |
| Any SUD, no. (% of psychos. category) | 59 (64.8%) | 25 (62.5%) | 22 (73.3%) | 12 (63.2%) | 0 (0%) |
| Alcohol | 30 (33.0%) | 15 (37.5%) | 11 (36.7%) | 4 (21.1%) | 0 (0%) |
| Cannabis | 53 (58.2%) | 21 (52.5%) | 21 (70.0%) | 11 (57.9%) | 0 (0%) |
| Stimulants | 15 (16.5%) | 9 (22.5%) | 4 (13.3%) | 3 (15.8%) | 0 (0%) |
| Hallucinogens | 14 (15.4%) | 2 (5.0%) | 7 (23.3%) | 5 (26.3%) | 0 (0%) |
| Ecstasy | 7 (7.7%) | 2 (5.0%) | 3 (10.0%) | 2 (10.5%) | 0 (0%) |
| Opioids | 3 (3.3%) | 1 (2.5%) | 1 (3.3%) | 1 (5.3%) | 0 (0%) |
| Pre-morbid functional status | |||||
| School | 55 (60.4%) | 29 (72.5%) | 14 (46.7%) | 11 (57.9%) | 1 (50.0%) |
| Full-time | 53 (58.2%) | 28 (70.0%) | 13 (43.3%) | 11 (57.9%) | 1 (50.0%) |
| Part-time | 2 (2.2%) | 1 (2.5%) | 1 (3.3%) | 0 (0%) | 0 (0%) |
| Work | 18 (19.8%) | 8 (20.0%) | 5 (16.7%) | 5 (26.3%) | 0 (0%) |
| Full-time | 13 (14.3%) | 7 (17.5%) | 4 (13.3%) | 2 (10.5%) | 0 (0%) |
| Part-time | 5 (5.5%) | 1 (2.5%) | 1 (3.3%) | 3 (15.8%) | 0 (0%) |
| Unemployed/not in school | 18 (19.8%) | 3 (7.5%) | 11 (36.7%) | 3 (15.8%) | 1 (50.0%) |
| Hospitalizations | |||||
| Prior, mean ± SD (range) | 1.6 ± 1.1 (0–7) | 1.4 ± 0.6 (0–3) | 1.7 ± 1.3 (0–7) | 1.7 ± 1.3 (0–5) | 2.0 ± 2.8 (0–4) |
| Referral source: | |||||
| Inpatient hospital | 53 (58.2%) | 20 (50.0%) | 19 (63.3%) | 14 (73.7%) | 0 (0%) |
| Partial hospital | 9 (9.9%) | 5 (12.5%) | 4 (13.3%) | 0 (0%) | 0 (0%) |
| Outpatient provider | 10 (11.0%) | 7 (17.5%) | 0 (0%) | 2 (10.5%) | 1 (50%) |
| Family | 19 (20.9%) | 8 (20.0%) | 7 (23.3%) | 3 (15.8%) | 1 (50%) |
NOS = not otherwise specified; SUD = substance use disorder; y = years; t = duration; m = months.
Figure 2.
Prevalence of pre-morbid substance use disorders (SUD) among all enrolled McLean OnTrack patients. SUD's are highly prevalent among our first-episode patients, regardless of psychosis category. Cannabis use disorders are the most common.
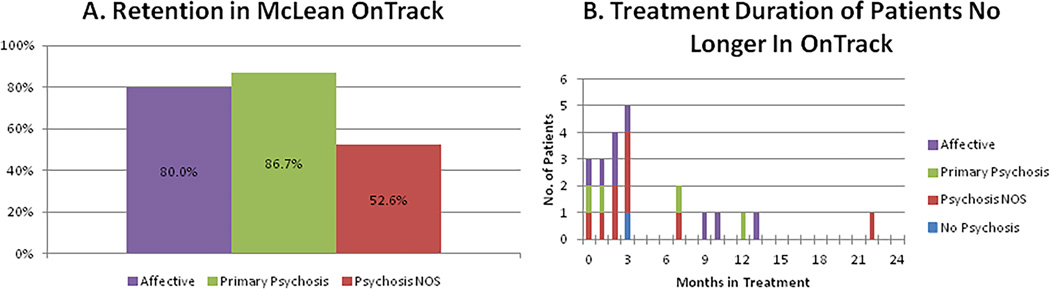
The overall retention rate (measured by the percentage of active patients) in OnTrack is 75.8%, with 80.0% for affective, 86.7% for primary psychosis, and 52.6% for psychotic disorder NOS (Figure 3A). Among patients who enrolled in OnTrack but are no longer active (n=22), fifteen (68.2%) dropped out at or before 3 months (early drop-outs), while seven (31.8%) engaged for 7 or more months before discontinuing treatment (later drop-outs). Among the early drop-outs, the majority (77.3%) had affective psychosis or psychotic disorder NOS (Figure 3B).
Figure 3.
Engagement in McLean OnTrack. A. The retention rate in psychotic disorder, not otherwise specified (NOS) is lower than that in affective and primary psychotic disorders. B. Patients with affective psychosis or psychotic disorder, NOS comprise the majority of individuals who dropped out of treatment early.
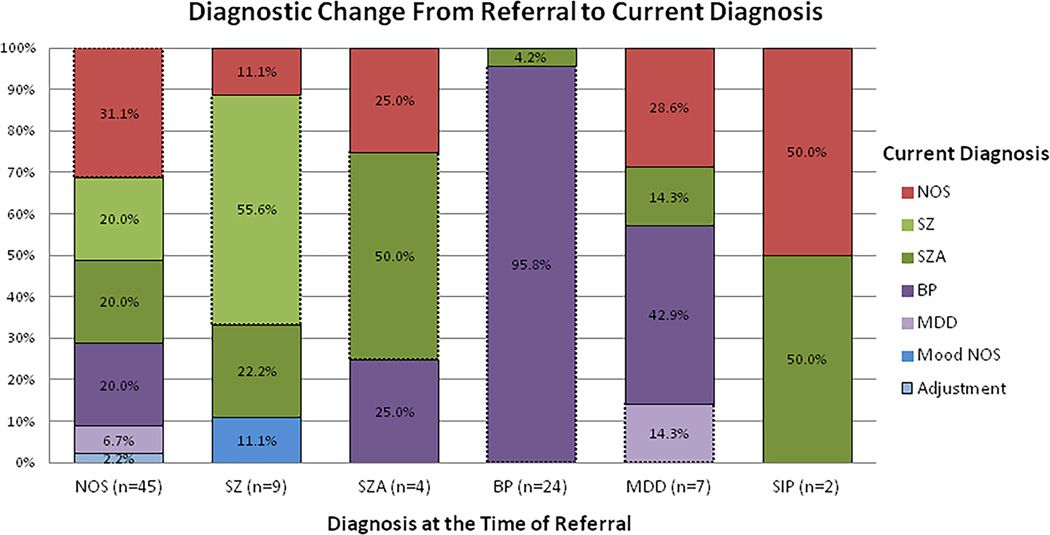
3.2. Evaluation of Diagnostic Change
50.5% of patients in OnTrack had a change in diagnosis between time of referral and the most recent documented diagnosis. Figure 4 shows the distribution of current diagnoses from each referral diagnosis. Patients referred with bipolar disorder with psychotic features are the most diagnostically stable, with only one patient (4.2%) having changed diagnosis. Diagnoses changed in 68.9% of psychotic disorder NOS referrals, 44.4% of schizophrenia referrals, 50.0% of schizoaffective disorder referrals, 85.7% of psychotic depression referrals, and in 100% of the two individuals referred with substance-induced psychosis.
Figure 4.
Distribution of current diagnoses for each referral diagnosis. Diagnostic change is common for all referral diagnoses except bipolar disorder with psychotic features. The areas of the bar graph outlined with dashed lines reflect diagnoses that remained consistent.
4. Discussion
McLean OnTrack is a specialized first-episode psychosis program that takes a dimensional and trans-diagnostic approach to early intervention, treating all-comers with first-episode psychosis under one roof. A first episode of psychosis is frequently associated with high clinical severity and marked disruption in functioning, and these challenges are not unique to schizophrenia. We tailor our approach to patients' individual needs, with the ultimate goal of helping individuals get back "on track," regardless of their diagnostic category.
Here, we report on baseline clinical and demographic data of OnTrack patients and find that diagnostic heterogeneity is the norm. Only 33% of OnTrack patients have a primary psychotic disorder (i.e,. schizophrenia or schizoaffective disorder). A large number of individuals with affective psychosis (44%) and psychotic disorder NOS (19%) comprise the clinic population as well. Our inclusive approach, to treat patients with a variety of psychotic disorders, has by definition resulted in a more heterogeneous patient group than is typically found in first-episode clinics in the U.S., and includes patients with bipolar disorder, major depressive disorder, and those with symptoms that are atypical or otherwise ill-defined.
We also find that shifts in diagnoses are common. In our sample, diagnoses evolved for 50.5% of patients following entry into our program. This rate is consistent with the overall rate (50.7%) of diagnostic shifts found in a study of first-admission psychosis patients followed for a decade14. Though the majority of patients referred with bipolar disorder with psychotic features were diagnostically stable, diagnostic change was otherwise common, suggesting that diagnosis tends to be highly dynamic in the course of early psychosis. The implications of this finding are two-fold: First, single-diagnosis specialty clinics that admit based on referral or baseline diagnosis are, in reality, likely treating a heterogeneous group of patients; second, limiting early interventions to only patients who clearly meet diagnostic criteria for schizophrenia early in their illness would miss many individuals who would otherwise benefit from intensive treatment.
Excluding individuals from receiving early intervention on the basis of referral diagnosis presents a missed opportunity to improve patient outcomes, as our data suggest that first-episode psychosis patients, regardless of diagnosis, stand to benefit from early intervention. Specifically, while the affective psychosis group has higher pre-morbid functional status, all categories of psychosis (affective, primary psychotic disorder, or psychotic disorder NOS) have similar baseline indices of illness severity, including high rates of prior hospitalizations and SUD, particularly cannabis use disorders. A recent study comparing first-episode patients with and without cannabis misuse at baseline found that baseline cannabis misuse was predictive of poorer social functioning over a 30 month follow-up period31. First-episode patients with co-morbid SUD have unique needs that may be different from SUD patients without psychosis, and even from SUD patients with chronic psychosis. To address these unique needs, we are working with SUD experts at McLean Hospital to develop a program geared specifically for SUD in first-episode patients, particularly targeting cannabis use disorder.
Furthermore, the retention rate in individuals with psychotic disorder NOS is markedly lower than that in clearly diagnosed affective and primary psychotic disorders, and patients with affective psychosis or psychotic disorder NOS comprised the majority of individuals who dropped out of treatment early. Getting “buy-in” from patients and families is essential for positive clinical outcomes and optimal use of resources. Our findings suggest that we need to step up efforts to increase patient engagement, and that those efforts should target individuals with affective psychosis or psychotic disorder NOS as well as those with primary psychotic disorders. Technology and social networking may offer creative solutions that enhance patient autonomy and synergistically complement our clinical services. A study of first-episode patients found that 100% regularly used computers, 92% cellphones/smartphones, and 83% gaming consoles, indicating that technology-based platforms for information and treatment delivery may be particularly beneficial for these patients32. We are developing a series of animated psychoeducational videos and a suite of mobile apps geared toward reaching the young adult demographic group. In focus groups, patients have expressed interest in using apps and electronic support tools to enhance their care, consistent with previous research33.
The National Institute of Mental Health (NIMH)'s Research Domain Criteria (RDoC) initiative is designed to encourage researchers to find new ways of classifying psychopathology based on dimensions of observable behavior and neurobiological measures, cutting across traditional diagnoses34. While the RDoC framework was intended primarily for research, it arises directly out of the clinical reality that existing psychiatric nosology is inadequate. McLean OnTrack represents an example of RDoC-consistent principles applied in the real world of clinical treatment. The findings from our OnTrack patient sample mirror the accumulating genetic and neurobiological research into the shared underpinnings of affective and non-affective psychotic disorders35, 36 as traditionally defined. Moreover, a trans-diagnostic clinical program such as OnTrack provides a natural referral source for translational investigations of the neurobiological and genetic causes of psychosis at the dimensional, rather than categorical, level. Our findings of diagnostic heterogeneity and instability early in illness point to the value of a more inclusive approach, and highlight the need for more availability of and research into trans-diagnostic early intervention programs that target the whole dimension of first-episode psychosis rather than the narrow category of schizophrenia.
We recognize that the trans-diagnostic approach is not without challenges. For example, we observe that the OnTrack psychotherapy group is primarily attended by individuals with affective psychosis. A major challenge in OnTrack is determining how best to deliver care in the face of diagnostic heterogeneity, uncertainty, and instability, as well as how to most efficiently and effectively adapt programs to benefit patients who share many but not all illness characteristics. Future directions might include personalized medicine approaches. For example, we have already mentioned the potential role for innovation and technology in reaching transitional age youth. A mobile app that can provide the treatment team with detailed metrics on each individual, derived from both active (i.e., pop-up surveys) and passive (i.e., sensor data such as accelerometer and phone usage) data collection, to generate a personalized phenotype could have major impact in aiding diagnosis and optimizing treatment planning.
Some limitations to our report deserve consideration. First, we present clinical diagnoses as documented in the patients' medical records; diagnoses were not systematically confirmed using a structured interview. On the other hand, our data were extracted from longitudinal medical records and reflect the richness of a real-world clinical setting. Second, while we provide data about the percentage of patients whose diagnoses have changed, we do not present data about when or why this occurred, which could provide insights into mechanism of evolution. In the future, we plan to examine whether such diagnostic changes result from improved recognition of existing symptomatology or from evolution of the illness itself.
To conclude, McLean OnTrack offers integrated, intensive treatment to all-comers with first-episode psychosis. We describe our goal to help first-episode patients get back “on track” regardless of their presumed diagnoses and the development of novel interventions to enhance patient engagement and decision-making. In our first-episode patients, diagnostic heterogeneity is the norm and diagnoses frequently change over the early illness course. Baseline indices of illness severity are similar across categories of first-episode psychosis, and suggest the need for early intervention, irrespective of diagnosis. Given these clinical realities, we recommend an inclusive approach that transcends traditional diagnostic boundaries when studying and treating first-episode patients.
Acknowledgments
We are grateful to the O’Keefe Family Foundation, the Gildea Family Foundation, Jane's Trust, and the Plimpton Shattuck Fund for their generous philanthropy. DO served on a scientific advisory board for Eli Lilly and Company in 2013. All other authors report no conflicts of interest.
References
- 1.McGorry PD, Purcell R, Hickie IB, Yung AR, Pantelis C, Jackson HJ. Clinical staging: a heuristic model for psychiatry and youth mental health. Med J Aust. 2007;187(7 Suppl):S40–S42. doi: 10.5694/j.1326-5377.2007.tb01335.x. [DOI] [PubMed] [Google Scholar]
- 2.McGorry PD, Hickie IB, Yung AR, Pantelis C, Jackson HJ. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. 2006;40(8):616–622. doi: 10.1080/j.1440-1614.2006.01860.x. [DOI] [PubMed] [Google Scholar]
- 3.McGorry PD. Issues for DSM-V: clinical staging: a heuristic pathway to valid nosology and safer, more effective treatment in psychiatry. Am J Psychiatry. 2007;164(6):859–860. doi: 10.1176/ajp.2007.164.6.859. [DOI] [PubMed] [Google Scholar]
- 4.Jackson HJ, McGorry PD. The Recognition and Management of Early Psychosis: A Preventive Approach. Second. Cambridge University Press; 2009. [Google Scholar]
- 5.Harrigan SM, McGorry PD, Krstev H. Does treatment delay in first-episode psychosis really matter? Psychol Med. 2003;33(1):97–110. doi: 10.1017/s003329170200675x. [DOI] [PubMed] [Google Scholar]
- 6.Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005;62(9):975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 7.Petersen L, Jeppesen P, Thorup A, et al. A randomised multicentre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. BMJ. 2005;331(7517):602. doi: 10.1136/bmj.38565.415000.E01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Craig TK, Garety P, Power P, et al. The Lambeth Early Onset (LEO) Team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ. 2004;329(7474):1067. doi: 10.1136/bmj.38246.594873.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGorry PD, Edwards J, Mihalopoulos C, Harrigan SM, Jackson HJ. EPPIC: an evolving system of early detection and optimal management. Schizophr Bull. 1996;22(2):305–326. doi: 10.1093/schbul/22.2.305. [DOI] [PubMed] [Google Scholar]
- 10.Norman RM, Manchanda R, Malla AK, Windell D, Harricharan R, Northcott S. Symptom and functional outcomes for a 5 year early intervention program for psychoses. Schizophr Res. 2011;129(2–3):111–115. doi: 10.1016/j.schres.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Kane JM, Schooler NR, Marcy P, et al. The RAISE early treatment program for first-episode psychosis: background, rationale, and study design. J Clin Psychiatry. 2015;76(3):240–246. doi: 10.4088/JCP.14m09289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mueser KT, Penn DL, Addington J, et al. The NAVIGATE Program for First-Episode Psychosis: Rationale, Overview, and Description of Psychosocial Components. Psychiatr Serv. 2015;66(7):680–690. doi: 10.1176/appi.ps.201400413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruggero CJ, Carlson GA, Kotov R, Bromet EJ. Ten-year diagnostic consistency of bipolar disorder in a first-admission sample. Bipolar Disord. 2010;12(1):21–31. doi: 10.1111/j.1399-5618.2009.00777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168(11):1186–1194. doi: 10.1176/appi.ajp.2011.11010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Craddock N, Owen MJ. Rethinking psychosis: the disadvantages of a dichotomous classification now outweigh the advantages. World Psychiatry. 2007;6(2):84–91. [PMC free article] [PubMed] [Google Scholar]
- 16.Berk M, Berk L, Dodd S, et al. Stage managing bipolar disorder. Bipolar Disord. 2013;16(5):471–477. doi: 10.1111/bdi.12099. [DOI] [PubMed] [Google Scholar]
- 17.Magalhaes PV, Dodd S, Nierenberg AA, Berk M. Cumulative morbidity and prognostic staging of illness in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) Aust N Z J Psychiatry. 2012;46(11):1058–1067. doi: 10.1177/0004867412460593. [DOI] [PubMed] [Google Scholar]
- 18.Berk M, Malhi GS, Hallam K, et al. Early intervention in bipolar disorders: clinical, biochemical and neuroimaging imperatives. J Affect Disord. 2009;114(1–3):1–13. doi: 10.1016/j.jad.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 19.Berk M, Brnabic A, Dodd S, et al. Does stage of illness impact treatment response in bipolar disorder? Empirical treatment data and their implication for the staging model and early intervention. Bipolar Disord. 2011;13(1):87–98. doi: 10.1111/j.1399-5618.2011.00889.x. [DOI] [PubMed] [Google Scholar]
- 20.Berk M, Conus P, Lucas N, et al. Setting the stage: from prodrome to treatment resistance in bipolar disorder. Bipolar Disord. 2007;9(7):671–678. doi: 10.1111/j.1399-5618.2007.00484.x. [DOI] [PubMed] [Google Scholar]
- 21.Kapczinski F, Dias VV, Kauer-Sant'Anna M, et al. Clinical implications of a staging model for bipolar disorders. Expert Rev Neurother. 2009;9(7):957–966. doi: 10.1586/ern.09.31. [DOI] [PubMed] [Google Scholar]
- 22.Scott J, Leboyer M, Hickie I, et al. Clinical staging in psychiatry: a cross-cutting model of diagnosis with heuristic and practical value. Br J Psychiatry. 2013;202(4):243–245. doi: 10.1192/bjp.bp.112.110858. [DOI] [PubMed] [Google Scholar]
- 23.Kapczinski F, Magalhaes PV, Balanza-Martinez V, et al. Staging systems in bipolar disorder: an International Society for Bipolar Disorders Task Force Report. Acta Psychiatr Scand. 2014;130(5):354–363. doi: 10.1111/acps.12305. [DOI] [PubMed] [Google Scholar]
- 24.Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry. 2013;70(9):913–920. doi: 10.1001/jamapsychiatry.2013.19. [DOI] [PubMed] [Google Scholar]
- 25.Hanevik H, Hestad KA, Lien L, Teglbjaerg HS, Danbolt LJ. Expressive art therapy for psychosis: A multiple case study. The Arts in Psychotherapy. 2013;40(3) [Google Scholar]
- 26.Potter NN. Narrative selves, relations of trust, and bipolar disorder. Philosophy, Psychiatry, & Psychology. 2013;20(1):57–65. [Google Scholar]
- 27.Kingdon DG, Turkington D. Cognitive therapy of schizophrenia. New York, NY: The Guilford Press; 2008. [Google Scholar]
- 28.Hogarty GE. Personal therapy for schizophrenia and related disorders. New York, NY: The Guilford Press; 2002. [Google Scholar]
- 29.Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62(9):996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- 30.McMurrich S, Sylvia LG, Dupuy JM, et al. Course, outcomes, and psychosocial interventions for first-episode mania. Bipolar Disord. 2012;14(8):797–808. doi: 10.1111/bdi.12001. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez-Blanch C, Gleeson JF, Koval P, Cotton SM, McGorry PD, Alvarez-Jimenez M. Social functioning trajectories of young first-episode psychosis patients with and without cannabis misuse: a 30-month follow-up study. PLoS One. 2015;10(4):e0122404. doi: 10.1371/journal.pone.0122404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdel-Baki A, Lal S, O DC, Stip E, Kara N. Understanding access and use of technology among youth with first-episode psychosis to inform the development of technology-enabled therapeutic interventions. Early Interv Psychiatry. 2015 doi: 10.1111/eip.12250. [DOI] [PubMed] [Google Scholar]
- 33.Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull. 2014;40(6):1244–1253. doi: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 35.Lichtenstein P, Yip BH, Bjork C, et al. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet. 2009;373(9659):234–239. doi: 10.1016/S0140-6736(09)60072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin PI, Mitchell BD. Approaches for unraveling the joint genetic determinants of schizophrenia and bipolar disorder. Schizophr Bull. 2008;34(4):791–797. doi: 10.1093/schbul/sbn050. [DOI] [PMC free article] [PubMed] [Google Scholar]