Abstract
Background:
Tibial fracture without concomitant fibular fracture is an injury that has long attracted notice for the fact that it sometimes heals cleanly, other times causes various problems when the bone does not heal, or misaligns. In this randomized clinical trial, we assessed two treatment modalities plating and intramedullary nailing for treatment of closed, noncomminuted tibial fractures with intact fibulae.
Materials and Methods:
During the three year period, 1470 patients with leg fractures were treated and out of which, 114 were eligible to enter the study. Of the eligible patients, 73 were recruited to enter the trial, and ultimately 69 of these were followed for at least one year. The patients were randomized into two groups, one of which was treated by plating of the fracture, the other group by intramedullary nailing, both of which are standard surgical procedures. The primary variables that influenced the outcome of the procedures in both treatments were the duration of surgery, the amount of bleeding, the time to union, the need to repeat surgery to achieve union, the need to remove a device, and patients’ complaints about pain or discomfort in the limb.
Results:
One case of nonunion occurred in the group treated with intramedullary nailing and one of the patients in this group developed late, deep infection in the screws location, which was resolved by screw removal (P = 0.285 and P = 0.478, respectively). In both groups the tibial fractures achieved union in about 4 months, though the intramedullary group underwent more operations to achieve union (dynamization was performed in 4 patients, representing 12.1% of the patients in this group, P = 0.047). During the followup period, the incidence of implant removal (after union) was not statistically significant between the two groups: two patients (6.1%) in the intramedullary group and four patients (11.1%) in the plate group (P = 0.675) had implants removed. Of the other studied variables, the difference between the two groups was statistically significant only with regard to patients’ complaints of pain in the limb and the number of individuals with knee pain (in both cases, P = 0.001). In the intramedullary group, 18 patients had no complaints (54.4%) and 13 complained of knee pain (39.4%), while in the plate group 29 had no complaints (80.6%).
Conclusion:
Based upon the findings of the present study, both the methods studied are suitable treatments for closed noncomminuted isolated tibial fractures, but the patients in whom intramedullary nails are used are more likely to require additional surgeries to achieve union, and probably will have more complaints of pain in their limbs or knees.
Keywords: Bone plates, intramedullary nailing, tibial fractures
MeSh terms: Implant, orthopaedic equipment, osteosynthesis, fracture, tibia
INTRODUCTION
Fractures of the tibia are the most common type of long bone fractures.1 There is a controversy in the literature about appropriate treatment of these fractures, and it has been said that when an issue is both common and a subject of controversy, it is worthy of attention,2 which is correct in this case.
For half a century, it has been observed that tibial fractures with intact fibulae may encounter complications. Indeed, the fibulae remain intact in only 10–15% of tibial fractures,3,4 but this may cause segments of the tibial fracture to remain separated. Charnley declared that although the initial force may be strong enough to break the tibia, the fibula, because of soft tissue surrounding it, remains protected, and this may cause complications.5 Jackson and Macnab found that tibial fracture without fibular fracture may result in a varus malunion.6 Sarmiento and Latta8 and Teitz et al.9 noted that these fractures, especially the diaphyseal types, will achieve union later and usually with a deformity of varus. It has also been noted that problems have been encountered during reaming of the intramedullary canal while nailing such fractures.10
Assuming that the intact fibula prevents compression of the fracture of the tibia, in the case of closed diaphyseal noncomminuted tibial fractures, intramedullary nailing may just preserve the alignment of the bone, and it might be better to use a plate, which can maintain the alignment of the bone and also provide compression to the broken segments. In the present study, we tried to answer this question of which method would produce better outcomes for these fractures.
MATERIALS AND METHODS
This clinical trial was performed between December 2009 and December 2012, in a tertiary care centre. The study was registered in the International Clinical Trial System (number IRCT201110292115N2). A written informed consent for participation in the study, after thorough explanation by researchers was taken from all patients.
Inclusion criteria were - A female or male ≥18 years, with close or open type 1 Gustilo-Anderson diaphyseal tibial fracture,10 and comminution type 0, 1 or 2 Winquist and Hansen,11 so that if a plate were used, there would be no need for a lag screw. The fibula intact and adequate diameter of the tibial canal for nailing. Absence of bone injury or visceral injury in other parts of the body. Absence of compartment syndrome or any other underlying disease that could affect bone union. Absence of pregnancy. Availability for at least 1-year of followup after surgery.
The sample size was calculated based on the formula:
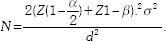
Considering d = 0.5, n = 88, α =0.05, β =0.1, and z = 2, the sample size would be 88. Patients were randomly divided into two groups: The first was treated with intramedullary nailing, the second with plating. Randomization was done by opening one of ten similar envelopes in which half had the words “intramedullary nailing” [Figure 1] and the other half the word “plate.” [Figure 2] The envelopes were replaced after the entry of each group of 10 patients to the study.
Figure 1.
(a) Preoperative x-rays anteroposterior and lateral views of leg bones showing isolated short oblique tibial fracture (b) Postoperative x-rays treated with intramedullary nailing
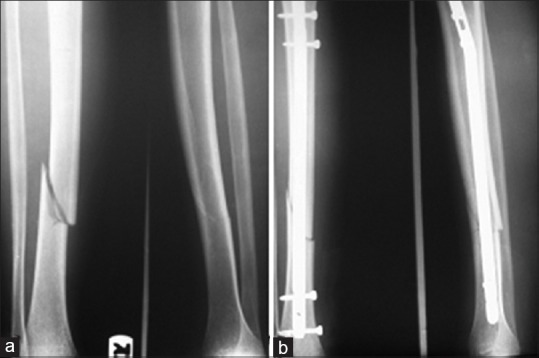
Figure 2.
(a) Preoperative x-ray leg bones anteroposterior and lateral views showing fracture middle 1/3rd tibia with intact fibula (b) Postoperative anteroposterior and lateral views showing plate in situ and union
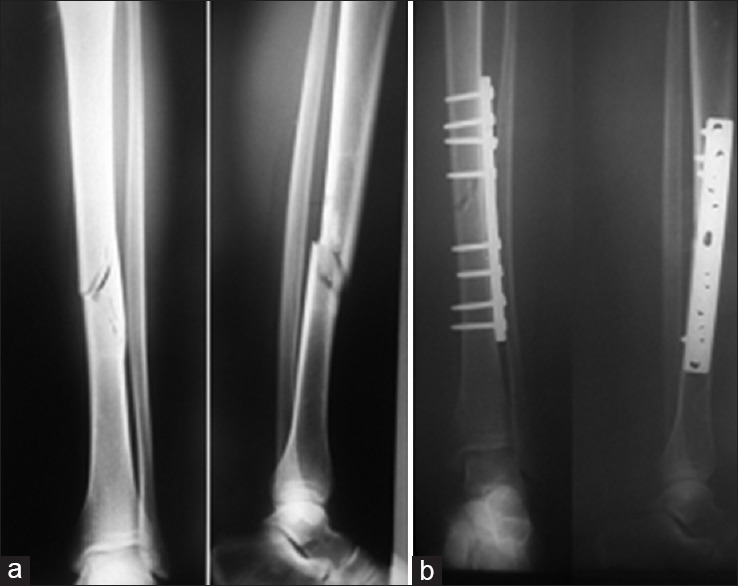
In the intramedullary nailing cohort, an intramedullary nail and two locking screws on each side (one of them in dynamic mode) were used to stabilize the fracture [Figure 3]. In the plating cohort, a narrow plate (4.5 mm) with eight screws and with at least four screws on each side of the fractures were used. Tourniquet was not used in either procedure.
Figure 3.
Followup X-ray of leg bones anteroposterior and lateral views of a patient in the nail group showing one of the proximal screws has been removed for dynamization
The amount of bleeding was estimated by an anesthesia technician by counting the number of the gauzes. Duration of the surgery was calculated by logging the time when surgery began until completion of the dressing. The amount of drainage from the site using the Hemovac drain (SUPA, Tehran, Iran) and the need for changes of dressing because of bleeding were noted after the patient entered the ward. Pain level was recorded by visual analog scale and scores of 1 and 2 were recorded as mild, 3 and 4 as moderate, 5 and 6 as severe, 7 and 8 as very severe, and 9 and 10 as intolerable. Patients were discharged 48 h after hospitalization.
Followup of patients was done at 2 weeks after the surgery and then monthly until union; after that every 6 months. In the intramedullary nailing cohort, dynamization was performed by proximal or distal screw removal (according to the location of fracture) if the union was not apparent after 3–4 months. If the union did not appear after 6 months, the case would have been considered a “nonunion” in both cohorts. Union was confirmed by observation of callus in the fracture site and by the ability of the patient to walk without pain and the support of a cane. Superficial infection was confirmed by clinical signs of erythema, swelling and hotness, and deep infection was confirmed by pus exudate. All the surgeries and followup visits were performed by a single surgeon.
Finally, the results were analyzed by Student's t-test, Chi-square test, Spearman and Fishers exact test using SPSS 20 software (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.).
RESULTS
During the study period, 1470 patients with leg fractures were referred to our center, 114 of whom were diagnosed with isolated tibial fractures were eligible for entry into the study (7.75%). Finally 69 patients who completed the followup period of at least 1-year were included in study. Entry of patients into the study is shown in the flow chart [Figure 4].
Figure 4.
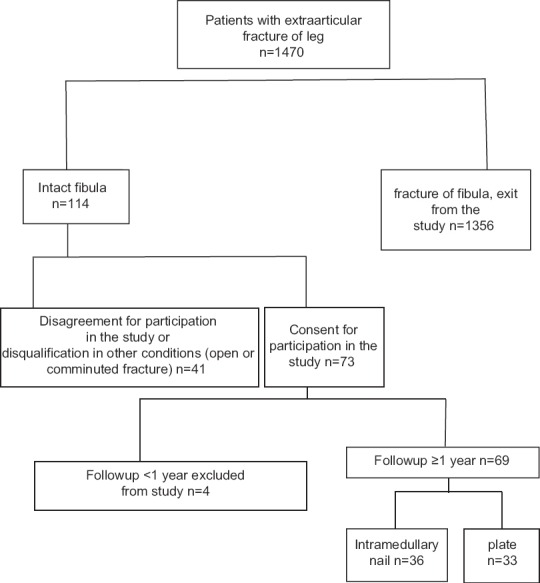
Flowchart of the referred patients to the hospital during the study
Demographics of the study participants are shown in Table 1. Considering the fact that the difference of “comminution” between two groups was statistically significant, correlations between study variables were evaluated and no significant relationships were observed, in particular for time to union and the severity of comminution, as the Spearman correlation coefficient was not significant (rho = 0.282), and the use of ANCOVA for eliminating the confounding effect of the severity of comminution did not seem to be necessary.
Table 1.
Demographic characteristics and comparison of two groups
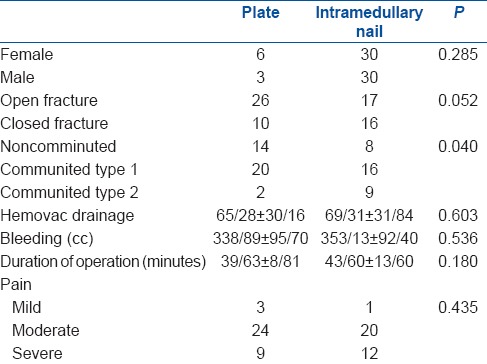
Results of the comparison of the two cohorts for the duration of surgery, amount of bleeding during surgery, amount of drainage to Hemovac, and degree of pain are shown in Table 1. Nonunion occurred in one of the patients (3.1%) from the intramedullary nailing cohort (P = 0.285), which by definition meant that the union had not been achieved after 6 months. The average time for union in the plating cohort was 4.30 ± 1.48 months, and in the intramedullary nailing cohort, it was 4.34 ± 1.45 months. The difference between cohorts was not significant (P = 0.787).
A revision surgery was required in eleven patients: Seven from the intramedullary nailing cohort and four from the plating cohort (P = 0.675). In six patients, reoperation was for device removal (plating (n=4) and intramedullary cohort (n=2), P = 0.675) and was done after complete union and after adequate time had elapsed (18 months after surgery) because of severe pain in the knee or at the surgical site, and in one case on patient's (plating cohort) request. Even if we consider the patient requested device removal unnecessary, and did not count it for that reason, it would not have changed the result. the difference between the two groups did not approach statistical significance (P = 0.542).
In four patients in the intramedullary nailing group, 4 months after surgery, there was no sign of union, so dynamization was performed by removing locking screws. If dynamization is considered to be an additional surgery required to achieve union, the difference between the two groups with regard to the number of subsequent surgeries was significant, affecting four patients (12.1%) in the intramedullary nailing group and none in the plating cohort (P = 0.047).
One patient in the intramedullary nailing group developed infection and abscess at the proximal screws site 9 months after surgery and following complete union. The infection was controlled by removal of the screws and with the administration of antibiotics. This was the only case of infection among all the patients (P = 0.478) of both groups.
Finally, the patients were divided into three groups with regard to complaints of pain in the limb or at the location of surgery: The first group had no complaints, the second complained of pain in the knee, and the third complained of pain in the limb. In the intramedullary nailing cohort, 18 patients had no complaints (54.5%), 13 patients had pain in the knee (39.4%), and one patient had pain in the leg (6.10%). In the plating cohort, 29 patients had no complaints (80.6%), one patient had pain in the knee (2.8%), and three patients had pain in their limb (8.3%) (P = 0.001). Considering the patients who had no complaints as a group, the difference between the two cohorts was significant (80.6% in the plating cohort had no complaint vs. 54.5% in the intramedullary nailing cohort, P = 0.001). Knee pain was significantly more common in the intramedullary nailing cohort (39.4% vs. 2.8%, P < 0.001). Regarding the number of patients who had pain in the limb, the difference between the cohorts was not significant (6.1% in the intramedullary nailing cohort vs. 8.3% in the plating cohort, P = 1). When the surgeon who performed all of the surgeries was asked for his preferred method, toward which he would counsel patients under similar conditions, the answer was plating, and when he was asked for the method that he would choose if he were so unfortunate to sustain such an injury, again the answer was plating.
DISCUSSION
In the present study, we evaluated two methods for treatment of fractures of the tibia with intact fibulae we did not find any advantage of either method from the standpoint of duration of the operation or the rate of union. There was a higher incidence of complaints in patients in the intramedullary nailing cohort, and their need for more surgeries to achieve union.
In the present study, approximately 8% of fractures were leg fracture with intact fibulae, and this is lower than the percentage mentioned in the literature.3,4 Although we could not find any justification for our lower rate of intact fibulae.
The current standard treatment for tibial fractures and the method of choice for surgical intervention are considered to be locked intramedullary nailing.12,13 Indeed, as we mentioned in the introduction to this report, tibial fracture with intact fibula is still considered a special fracture of the leg, but even in such fractures, it seems that the best treatment is surgery,13 and intramedullary nailing is an appropriate method, although the surgical technique may be more complex than plating.10 The method of choice for treatment of tibial shaft fractures is considered to be intramedullary nailing, but our research shows no scientific reason for this statement, based on a comparison of different methods (in closed noncomminuted fractures), and in the primary textbook, the rationale is only the results of a questionnaire answered by orthopedic surgeons, almost all of whom preferred the intramedullary nailing method.14 Of course, many studies have compared these two methods, but almost all of them have been performed on distal and metaphyseal fractures, and the main discussion has been on the necessity and method of fixation of the fibula, a discussion that continues.15,16,17,18,19,20,21 In fact, we could find few studies like the current one despite our efforts to search: A paper for which only an abstract was available reported on comminuted and noncomminuted fractures together, and concluded that intramedullary nailing is better for comminuted fractures and plating is better for noncomminuted fractures.22 Another study which enrolled patients with open, closed, and comminuted fractures reached a similar conclusion.23 In yet another study, for which only an abstract was available, a locking plate was considered a better treatment with lower complications and price24 than the intramedullary nailing procedure.
In the present study, we avoided tourniquet use in both cohorts, and the main reason was that tourniquet use is contraindicated with reaming of the intramedullary canal, because of the possibility of intramedullary bone necrosis.12 For the sake of a uniform study protocol, this precluded the use of a tourniquet in the plating cohort, although there are studies that recommend against tourniquet use during plating of tibial fractures as well.25,26
In the present study, there was no difference between the two cohorts regarding the need for surgeries to remove a device, owing to the fact that a followup period of 1-year or more was not achieved for all of the patients. It should be noted that most cases of nail removal for tibial fractures are performed in response to complaints of pain in the knee or at the site of the screws.27,28 From this observation, we conclude that patients who receive this treatment may require surgery for device removal at a higher rate than those who receive plating as therapy. This conclusion suggests that a study with a followup period is needed.
Patients in the intramedullary nailing cohort had more complaints of pain in their limb (not just at the site of surgery). Anterior knee pain was reported by 39.4% of the patients in the intramedullary nailing cohort, a smaller percentage than reported by most of other studies we cited; we found just one study that reported pain statistics similar to our study.29 Knee pain is a very common complication of tibial fractures treated with intramedullary nailing and is reported by 50–70% of patients.12,13,30,31,32
We inserted both proximal and distal interlocking screws, the more distal of the proximal ones in dynamic mode, because of these fractures tendency to heal in valgus. This may have led to unnecessary dynamization in 4 of our patients in the intramedullary cohort, as stable fractures may not need static locking,33 though for the purpose of dynamization, we used to remove both proximal screws.
There was no case of infection or nonunion in the plating group in our study. Plating is rarely used in fractures of the tibial shaft and it is used, for example, in osteoporotic patients, when there is a deformity of the tibia because of prior surgery, and when there is canal with a small diameter; these are cases in which use of the nail is actually impossible. Hence, we could not compare our findings to others’.
The inadequate diameter of the tibial canal is not uncommon; the diameter of the canal was <8 mm in 30% of patients in one study.34 The most important problem for the use of plating in tibial fractures is periosteal damage,12 which is preventable with less invasive methods. As was mentioned, with the growth in popularity of intramedullary devices, screws and plates have been used less often for a long time, and we did not encounter a recent article about the incidence of infection in patients who received this therapy. Overall, it seems that plate utilization, especially if performed with minimal manipulation of soft tissues, is probably a good choice for patients with fractures similar to those of our patients, a conclusion that experienced surgeons have reached previously35 and which apparently our surgeon believed by the end of the study.
The most important limitation of the present study was inadequate followup with all of the patients, to know what percentage would eventually require that the device be removed from their limbs. The small sample size. Followup with patients was done by the surgeon who performed the surgeries, which may be another limitation, but it should be noted that any other person following these patients would inevitably have identified which treatment cohort he or she belonged to.
CONCLUSIONS
From the results of the present study, both of the studied methods are suitable treatments for closed, isolated noncomminuted tibial fractures with a high probability of success, but the patients treated with intramedullary nails will more frequently require reoperation to achieve union, and will have a higher rate of complaints of pain in their limb and at the site of surgery.
Financial support and sponsorship
The study has been financially supported by Kerman University of Medical Sciences with paying the researchers.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pan RH, Chang NT, Chu D, Hsu KF, Hsu YN, Hsu JC, et al. Epidemiology of orthopedic fractures and other injuries among inpatients admitted due to traffic accidents: A 10-year nationwide survey in Taiwan. Scientific World Journal 2014. 2014 doi: 10.1155/2014/637872. 637872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nicoll EA. Closed and open management of tibial fractures. Clin Orthop Relat Res. 1974;105:144–53. Hammer R, Edholm P, Lindholm B. Stability of union after tibial shaft fracture. Analysis by a non-invasive technique. J Bone Joint Surg Br 1984;66:529-34. [PubMed] [Google Scholar]
- 3.Hooper G, Buxton RA, Gillespie WJ. Isolated fractures of the shaft of the tibia. Injury. 1981;12:283–7. doi: 10.1016/0020-1383(81)90202-3. [DOI] [PubMed] [Google Scholar]
- 4.Lambert KL. The weight-bearing function of the fibula. A strain gauge study. J Bone Joint Surg Am. 1971;53:507–13. [PubMed] [Google Scholar]
- 5.Charnley J. The Closed Treatment of Common Fractures. 3rd ed. New York: Churchill Livingstone; 1961. [Google Scholar]
- 6.Jackson RW, Macnab I. Fractures of the shaft of the tibia; a clinical and experimental study. Am J Surg. 1959;97:543–57. doi: 10.1016/0002-9610(59)90245-4. [DOI] [PubMed] [Google Scholar]
- 7.Sarmiento A, Latta LL. Closed Functional Treatment of Fractures. Berlin: Springer Verlag; 1981. [Google Scholar]
- 8.Teitz CC, Carter DR, Frankel VH. Problems associated with tibial fractures with intact fibulae. J Bone Joint Surg Am. 1980;62:770–6. [PubMed] [Google Scholar]
- 9.Bonnevialle P, Bellumore Y, Foucras L, Hézard L, Mansat M. Tibial fracture with intact fibula treated by reamed nailing. Rev Chir Orthop Reparatrice Appar Mot. 2000;86:29–37. [PubMed] [Google Scholar]
- 10.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 11.Winquist RA, Hansen ST., Jr Comminuted fractures of the femoral shaft treated by intramedullary nailing. Orthop Clin North Am. 1980;11:633–48. [PubMed] [Google Scholar]
- 12.Rudloff MI. Fractures of the lower extremity. In: Canal ST, Beaty JH, editors. Campbell's Operative Orthopedics. 12th ed. Elzevier; 2013. pp. 2650–7. [Google Scholar]
- 13.Petrisor BA, Bhandari M, Schemitsch E. Tibia and fibulae fractures. In: Bucholz RW, Heckman JD, Court-Brown CM, Tornetta P, editors. Rockwood and Green's Fractures in Adults. 7th ed. Lippincot, Williams and Wilkins; 2010. pp. 1880–2. [Google Scholar]
- 14.Court-Brown CM. Fractures of the tibia and fibulae. In: Bucholz RW, Heckman JD, Court-Brown C, editors. Rockwood and Green's Fractures in Adults. 6th ed. Philadelphia: Lippincott, Williams and Wilkins; 2006. pp. 2080–146. [Google Scholar]
- 15.Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A. Treatment of distal tibial shaft fractures by three different surgical methods: A randomized, prospective study. Int Orthop. 2014;38:1261–7. doi: 10.1007/s00264-014-2294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Attal R, Maestri V, Doshi HK, Onder U, Smekal V, Blauth M, et al. The influence of distal locking on the need for fibular plating in intramedullary nailing of distal metaphyseal tibiofibular fractures. Bone Joint J. 2014;96-B:385–9. doi: 10.1302/0301-620X.96B3.32185. [DOI] [PubMed] [Google Scholar]
- 17.Seyhan M, Unay K, Sener N. Intramedullary nailing versus percutaneous locked plating of distal extra-articular tibial fractures: A retrospective study. Eur J Orthop Surg Traumatol. 2013;23:595–601. doi: 10.1007/s00590-012-1016-x. [DOI] [PubMed] [Google Scholar]
- 18.Vallier HA, Cureton BA, Patterson BM. Factors influencing functional outcomes after distal tibia shaft fractures. J Orthop Trauma. 2012;26:178–83. doi: 10.1097/BOT.0b013e31823924df. [DOI] [PubMed] [Google Scholar]
- 19.Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma. 2011;25:736–41. doi: 10.1097/BOT.0b013e318213f709. [DOI] [PubMed] [Google Scholar]
- 20.Ehlinger M, Adam P, Gabrion A, Jeunet L, Dujardin F, Asencio G, et al. Distal quarter leg fractures fixation: The intramedullary nailing alone option. Orthop Traumatol Surg Res. 2010;96:674–82. doi: 10.1016/j.otsr.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Bonnevialle P, Lafosse JM, Pidhorz L, Poichotte A, Asencio G, Dujardin F, et al. Distal leg fractures: How critical is the fibular fracture and its fixation? Orthop Traumatol Surg Res. 2010;96:667–73. doi: 10.1016/j.otsr.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Huang P, Tang PF, Yao Q, Liang YT, Tao S, Zhang Q, et al. A comparisive study between intramedullary interlocking nail and plate-screw fixation in the treatment of tibial shaft fractures. Zhongguo Gu Shang. 2008;21:261–3. [PubMed] [Google Scholar]
- 23.Johner R, Wruhs O. Classification of tibial shaft fractures and correlation with results after rigid internal fixation. Clin Orthop Relat Res. 1983;178:7–25. [PubMed] [Google Scholar]
- 24.Huang P, Tang P, Yao Q. Comparison of LCP and locked intramedullary nailing fixation in treatment of tibial diaphysis fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2007;21:1167–70. [PubMed] [Google Scholar]
- 25.Saied A, Zyaei A. Tourniquet use during plating of acute extra-articular tibial fractures: Effects on final results of the operation. J Trauma. 2010;69:E94–7. doi: 10.1097/TA.0b013e3181dbac93. [DOI] [PubMed] [Google Scholar]
- 26.Salam AA, Eyres KS, Cleary J, el-Sayed HH. The use of a tourniquet when plating tibial fractures. J Bone Joint Surg Br. 1991;73:86–7. doi: 10.1302/0301-620X.73B1.1991784. [DOI] [PubMed] [Google Scholar]
- 27.Sidky A, Buckley RE. Hardware removal after tibial fracture has healed. Can J Surg. 2008;51:263–8. [PMC free article] [PubMed] [Google Scholar]
- 28.Karladani AH, Ericsson PA, Granhed H, Karlsson L, Nyberg P. Tibial intramedullary nails – Should they be removed? A retrospective study of 71 patients. Acta Orthop. 2007;78:668–71. doi: 10.1080/17453670710014374. [DOI] [PubMed] [Google Scholar]
- 29.Song SY, Chang HG, Byun JC, Kim TY. Anterior knee pain after tibial intramedullary nailing using a medial paratendinous approach. J Orthop Trauma. 2012;26:172–7. doi: 10.1097/BOT.0b013e3182217fe6. [DOI] [PubMed] [Google Scholar]
- 30.Toivanen JA, Väistö O, Kannus P, Latvala K, Honkonen SE, Järvinen MJ. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft. A prospective, randomized study comparing two different nail-insertion techniques. J Bone Joint Surg Am. 2002;84-A:580–5. doi: 10.2106/00004623-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Bhattacharyya T, Seng K, Nassif NA, Freedman I. Knee pain after tibial nailing: The role of nail prominence. Clin Orthop Relat Res. 2006;449:303–7. doi: 10.1097/01.blo.0000223976.91089.08. [DOI] [PubMed] [Google Scholar]
- 32.Darabos N, Bajs ID, Rutic Z, Darabos A, Poljak D, Dobsa J. Nail position has an influence on anterior knee pain after tibial intramedullary nailing. Coll Antropol. 2011;35:873–7. [PubMed] [Google Scholar]
- 33.Drosos GI, Bishay M, Karnezis IA, Alegakis AK. Factors affecting fracture healing after intramedullary nailing of the tibial diaphysis for closed and grade I open fractures. J Bone Joint Surg Br. 2006;88:227–31. doi: 10.1302/0301-620X.88B2.16456. [DOI] [PubMed] [Google Scholar]
- 34.Uhlin B, Hammer R. Attempted unreamed nailing in tibial fractures: A prospective consecutive series of 55 patients. Acta Orthop Scand. 1998;69:301–5. doi: 10.3109/17453679809000935. [DOI] [PubMed] [Google Scholar]
- 35.Schmidt AH, Finkemeier CG, Tornetta P., 3rd Treatment of closed tibial fractures. Instr Course Lect. 2003;52:607–22. [PubMed] [Google Scholar]


