Abstract
Background: Treatment outcomes of tuberculosis (TB) in children are rarely evaluated by most national TB programmes in sub-Saharan Africa. This study evaluated the treatment outcomes of children treated for TB in Lagos State, Nigeria.
Methods: A retrospective review of programme data of the Lagos state TB and the Leprosy control programme in Nigeria from 1 January 2012 to 31 December 2012. Treatment outcomes were categorized according to the national TB guidelines.
Results: A total of 535 cases of childhood TB were notified in 2012, representing 6.3% of the total TB cases notified in Lagos state in 2012. The prevalence of TB/HIV co-infection was 29%. The treatment success rate was 79.2% in TB/HIV-negative children compared with 73.4% in TB/HIV-positive children (p = 0.1268). Children <1 year had the worst treatment outcomes (p < 0.001).
Conclusion: There is a need to intensify effort at improving notification and treatment outcomes in children.
Keywords: childhood, TB, treatment outcome
INTRODUCTION
Globally, tuberculosis (TB) remains a public health problem associated with significant morbidity and mortality. In 2012, about 530 000 children were diagnosed with TB, translating to about 6% of all new TB cases [1]. The proportion of TB in children is said to vary with the prevalence of TB in adults. This ranges from <5% in low-burden countries to 20–40% in high-burden countries [2]. The epidemiology of childhood TB has been poorly described, and as such, there are no reliable data or exact estimates of the incidence, prevalence and mortality of childhood TB in most regions of the world [3]. The reason for this is not farfetched. Childhood TB is associated with diagnostic dilemmas as well as lack of precise case definitions. In addition, they rarely produce sputum and tend to have negative results on sputum smear examination. Diagnosis, therefore, is often based on a constellation of clinical symptoms and non-specific investigations [4]. Childhood TB had been neglected largely by the National Tuberculosis Control Programmes (NTPs) because disease in childhood is often paucibacillary, and children are not considered to contribute significantly to disease transmission [5]. The occurrence of TB in children has, however, been considered a sentinel event, because it is a pointer of recent transmission in the community and also represents a failure of public health prevention measures to a large extent [6].
The treatment outcomes of TB treatment in children are rarely evaluated by the NTPs, including the Nigerian National Tuberculosis and Leprosy Control Programme (NTBLCP). Some studies however have suggested that treatment outcomes of children diagnosed and treated for TB vary from one country to another depending on age, sex, occurrence of adverse events during treatment and HIV status [7]. The significance of childhood TB cannot be overemphasized, especially in a country like Nigeria, being one of the 22 high-burden countries responsible for about 80% of total TB cases worldwide, and 75% of childhood TB [8]. The surveillance data on childhood TB, which are important in identifying the predictors of poor treatment outcomes in children, are largely lacking. In addition, there are no data regarding the contribution of childhood TB-to-TB burden and the treatment outcomes of TB in children in Nigeria. This study therefore assessed the treatment outcomes of childhood TB in Lagos State, Nigeria.
METHODOLOGY
Study design
A retrospective review of routine programme data of all children diagnosed and treated for TB from 1 January 2012 to 31 December 2012 in Lagos state, Nigeria was conducted.
Lagos state has a population of 9.3 million according to the 2006 national population census. The public and private sector were involved in provision of health care services in Lagos State. The Lagos State tuberculosis and leprosy control programme (LSTBLCP) commenced operation in 2003 in collaboration with international agencies, which include the International Union against TB and Lung Diseases, World Health Organization (WHO), Canadian International Development Agency (CIDA) and the United States Agency for International Development (USAID). There were 218 treatment facilities offering directly observed treatment short course (DOTS) under the LSTBLCP at the end of 2012. Of the 218 DOTS centres in Lagos State, 61(30%) notified childhood TB in 2012. This consists of 43 public DOTS (29 primary health centres, 11 secondary health and 3 tertiary health centres) facilities and 18 private DOTS facilities.
TB diagnosis and treatment
Childhood TB is defined by the national TB programme as TB occurring in children <15 years,14 and any child with cough for ≥2 weeks is considered as presumptive TB case. Two samples are usually collected from children who can produce sputum for acid fast bacilli (AFB) test. If any of the sputum AFB test is positive for TB, the patient is classified as sputum smear-positive pulmonary TB. In the event of a negative result, other diagnostic tests like chest radiograph, tuberculin test, erythrocyte sedimentation rate were performed to aid diagnosis of TB. If the radiographic findings were consistent with the clinical signs and symptoms of TB, the child is diagnosed as sputum smear-negative pulmonary TB. For younger children who cannot produce sputum for smear microscopy, diagnosis is usually made with the use of a score chart according to the national TB guidelines. The score chart takes into consideration parameters that include chest radiography abnormalities, history of close contact with a smear-positive pulmonary TB patient, growth faltering, poor or non-response to antibiotics and readings of tuberculin skin test where available. A score >7 is suggestive of TB. Children with extra-pulmonary TB are usually diagnosed in secondary and tertiary health facilities, where there are facilities for histological and radiological diagnosis depending on the organ of the body affected. Majority of the DOTS centres at the primary health care centres were manned by community health officers and community health extension workers, while those at the secondary and tertiary facilities were supervised by doctors. Diagnosis of childhood TB is exclusively made by doctors when sputum AFB results are not available. Children who cannot produce sputum or have negative sputum AFB results who presented to a DOTS facility where there are no medical officers were usually referred to facilities where there are medical officers for diagnosis.
Each presumptive TB patient was routinely offered HIV testing by the health care workers at the DOTS facility. The HIV rapid test kit used in accordance with the national HIV Counseling and Testing (HCT) policy was Determine (determine HIV-1/2 Alere Determine™, Japan 2012) and Uni-Gold™ (Trinity Biotech PLC, Wicklow, Ireland 2013) in parallel algorithm. A concordance result was regarded as positive. In cases of a discordant result, STAT-PAK® was used as the tie breaker.
Treatment of TB in children is free because drugs are provided by the State TB and leprosy programme. The duration of TB treatment was 6 months. The treatment regimen consisted of 2 months intensive phase of Rifampicin, Isoniazid and Pyrazinamide and Ethambutol and 4 months continuation phase of Rifampicin and Isonizid. Patients who were TB/HIV co-infected were offered Cotrimoxazole preventive therapy (CPT) along with their anti-TB medications. TB/HIV co-infected patients were referred to the antiretroviral therapy (ART) clinic, where they are offered ART within 8 weeks of commencement of their anti-TB medications.
TB treatment outcomes were categorized according to the Nigerian National TB guidelines as follows.
Cure: This was the proportion of patients among smear-positive patients that completed treatment and had at least two negative smears with an interval of at least 1 month, one of which should be obtained at the end of treatment.
Treatment completed: This was the proportion of patients that completed treatment, but sputum examination results are not available.
Died: The proportion of patients that died before completion of treatment.
Default: This was the proportion of patients that did not take drugs for two consecutive months or more.
Treatment failure: This was the proportion of patients who are still sputum smear positive
at ≥5 months after the commencement of chemotherapy, or who interrupted treatment for >2 months after completing 1 month of chemotherapy, returned to treatment and are found to be smear positive
Transferred out: This was the proportion recorded that moved out of the health facility catchment area.
Treatment success: Defined as the sum of the cases that were cured and that completed treatment.
Recording and reporting system
TB activities in Lagos State are being coordinated by the state TB control officer. At the local government (district) level, the local government TB supervisors coordinate the activities of the DOTS facilities in each local government. In addition, they oversee the TB focal person in each DOTS facility, ensuring that the patient’s treatment cards are properly filled. Details of patients treated for TB were entered into the TB facility register by the TB focal person at that facility, and details of TB patients treated in all the DOTS facilities in each local government were entered into the local government TB treatment register by the local government TB supervisors. The data for each local government were usually sent to the state on a quarterly basis. Mode of reporting is paper based.
Data analysis: Data were entered and analyzed using the Statistical Package for Social Sciences version 19. Chi squared test and Fisher’s exact test were used to compare categorical variables as the case may be. The Student's t-test was used to compare means of continuous variables. Confidence interval was set at 95% for all statistical tests. Microsoft excel was used to draw charts.
Ethical issues: Data for this study were retrieved from secondary data routinely collected by the Lagos State TB control programme, and as such, no ethical clearance was obtained.
RESULTS
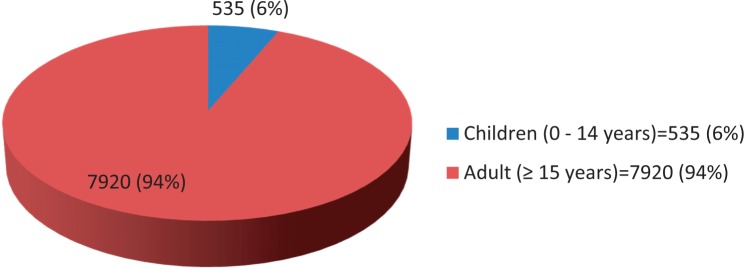
A total of Eight thousand four hundred and fifty-five patients were registered for treatment in 2012. Of these, 535 (6.3%) were children <15 years of age as shown in Fig. 1. About 13.0% of the children treated for TB were <1 year old, while 61.3% were aged between 5 and 14 years. About 91% of the children had pulmonary TB, 93% were new TB cases, 20.6% of the cases were diagnosed by smear microscopy, 69.9% by chest radiographs and 3.7% were diagnosed clinically. The majority (95.5%) were treated at the public DOTS facilities; HIV test was not done for 42 (76.9%) children. Of the children that underwent HIV test, 29% (149/493) were HIV positive as shown in Table 1. The prevalence of TB/HIV co-infection was 29%.
Fig. 1.
Proportion of childhood TB treated in 2012 (n = 8455).
Table 1.
Socio demographic characteristics of children treated for TB
| Variable | Frequency (n = 535) | % |
|---|---|---|
| Age group (years) | ||
| <1 year | 69 | 12.9 |
| 1–4 years | 138 | 25.8 |
| 5–14 years | 328 | 61.3 |
| Mean ± SD | 7.0 ± 4.8 | |
| Gender | ||
| Male | 277 | 51.8 |
| Female | 258 | 48.2 |
| Treatment category | ||
| New cases | 495 | 92.5 |
| Retreatment cases | 40 | 7.5 |
| Type of TB | ||
| Pulmonary | 486 | 90.8 |
| Extra pulmonary | 49 | 9.2 |
| Mode of diagnosis | ||
| Smear AFB | 110 | 20.6 |
| CXR | 374 | 69.9 |
| Clinical | 20 | 3.7 |
| Mantoux | 11 | 2.1 |
| Not reported | 20 | 3.7 |
| Type of facility | ||
| Public | 511 | 95.5 |
| Private | 24 | 4.5 |
| HIV status | ||
| Positive | 143 | 26.7 |
| Negative | 350 | 65.4 |
| Not done | 42 | 7.9 |
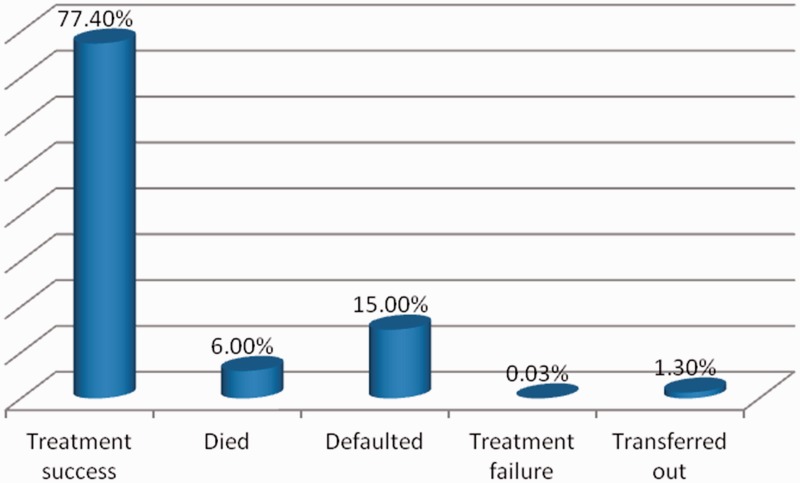
The proportion of children that had treatment success was 77.4%; 6.0% died and 15.0% defaulted (Figure 2). Table 2 shows that the proportion of children that had treatment success was significantly higher among children aged 5–14 years (82%) compared with those aged between 1–4 years (75.3%) and those <1 year (59.4%) (p < 0.001). The proportion of children that died while receiving treatment (13.0%) and defaulted (27.5%) was significantly higher in those <1 year old compared with the other age groups (p < 0.05). A higher proportion (78%) of the HIV-negative children compared with 73.4% of those who were HIV positive had successful treatment (p = 0.127). However, a significantly higher proportion (11.2%) of the HIV-positive children treated for TB compared with 4.0% of HIV-negative children died (p < 0.001). The defaulter rate among the HIV-positive and HIV-negative children was comparable as shown in Table 3. Table 4 shows that a significantly higher proportion (44.9%) of children <1 year compared with those who were 1–4 years and 5–14 years were HIV positive. Age was significantly associated with treatment success. The mean age of children who had treatment success was significantly higher. (p = 0.004). HIV status, gender and type of TB were not associated with treatment success Table 5.
Fig. 2.
Treatment outcomes of childhood TB in 2012 (n =535).
Table 2.
. Treatment outcomes of childhood TB by age groups
| Treatment outcomes | Age groups |
|||
|---|---|---|---|---|
| <1 year |
1–4 years |
5–14 years |
p | |
| N = 69 (%) | n = 138 (%) | n = 328 (%) | ||
| Treatment success | 41 (59.4) | 104 (75.3) | 269 (82.0) | <0.001 |
| Died | 9 (13.1) | 9 (6.5) | 14 (4.3) | 0.019 |
| Defaulted | 19 (27.5) | 22 (15.9) | 39 (11.9) | 0.004 |
| Treatment failure | – | 1 (0.7) | 1 (0.3) | 0.685 |
| Transferred out | – | 2 (1.4) | 5 (1.5) | 0.590 |
Table 3.
. Treatment outcomes of childhood TB by HIV status
| Treatment outcome | HIV positive |
HIV negative |
p |
|---|---|---|---|
| n = 143 (%) | n = 350 (%) | ||
| Treatment success | 105 (73.4) | 279 (79.7) | 0.127 |
| Died | 16 (11.2) | 14 (4.0) | 0.002 |
| Defaulted | 20 (14.0) | 51 (14.6) | 0.867 |
| Treatment failure | 0 (0.0) | 2 (0.6) | 0.504a |
| Transferred out | 2 (1.4) | 4 (1.1) | 0.591a |
aFisher’s exact p value.
Table 4.
. Distribution of HIV-positive and HIV-negative children treated for TB by age group
| HIV status | Age group |
p | ||
|---|---|---|---|---|
| <1 year |
1–4 years |
5–14 years |
||
| N = 69 (%) | n = 138 (%) | n = 328 (%) | ||
| Positive | 31 (44.9) | 41 (29.7) | 71 (21.6) | <0.001 |
| Negative | 34 (49.3) | 86 (62.3) | 230 (70.1) | |
| Not donea | 4 (5.8) | 11 (8.0) | 27 (8.2) | |
aNot part of the analysis.
Table 5.
Factors associated with treatment success of childhood TB in Lagos State
| Variable | Treatment success |
Test | p | |
|---|---|---|---|---|
| Yes |
No |
|||
|
n = 414 |
n = 121 |
|||
| Frequency (%) | Frequency (%) | |||
| Age | ||||
| <1 year | 41 (59.4) | 28 (40.6) | ||
| 1–4 years | 104 (75.4) | 34 (24.6) | ||
| 5–14 years | 269 (82.0) | 59 (18.0) | ||
| Mean ± SD | 7.3 ± 4.6 | 5.9 ± 5.1 | 2.926a | 0.004 |
| Type of facility | ||||
| Public | 396 (77.5) | 115 (22.5) | 0.082b | 0.775 |
| Private | 18 (75.0) | 6 (25.0) | ||
| Gender | ||||
| Male | 217 (78.3) | 60 (21.7) | 0.300b | 0.584 |
| Female | 197 (76.4) | 61 (23.6) | ||
| Treatment category | ||||
| New cases | 386 (78.0) | 109 (22.0) | 1.347b | 0.246 |
| Retreated cases | 28 (70.0) | 12 (30.0) | ||
| TB site | ||||
| Pulmonary | 381 (78.4) | 105 (21.6) | 3.104b | 0.078 |
| Extra pulmonary | 33 (67.3) | 16 (32.7) | ||
| HIV status | n = 384 (%) | n = 109 (%) | ||
| Positive | 105 (73.4) | 38 (26.6) | 2.33b | 0.127 |
| Negative | 279 (79.7) | 71 (20.3) | ||
at' test.
bChi squared test.
DISCUSSION
Of the total TB cases notified in Lagos State in 2012, the proportion of childhood TB was 6.3%. This finding is similar to the 2012 national figure [9], the 2012 global figure [1] and elsewhere in Africa [4, 10]. However, this figure was low compared with what was reported in other high TB-burden countries in Africa [7, 11–13]. Misdiagnosis/under-diagnosis of childhood TB is a common problem in TB-endemic countries, including Nigeria [6]. Diagnosis of childhood TB is made exclusively by doctors in Lagos, Nigeria; although presumptive childhood TB cases were usually referred by other health workers to DOTS facilities manned by doctors for diagnosis, there is a huge possibility of missed diagnosis because <15% of the DOTS centres in the state are covered by doctors. The 2012 National TB prevalence survey put the prevalence of smear-positive TB cases at 318/100 000 populations; this figure compared with the previous WHO estimate of 131/100 000 strongly suggests that childhood TB is grossly under-reported in Nigeria [14, 15].
The low case notification rate in Nigeria could be responsible for the low childhood TB case notification obtained in this study. The TB case notification rate in 2012 was 53/100 000 population, which is low compared with the TB burden in the country.9 The challenges of routinely collected TB surveillance data in terms of quality, completeness and accuracy of data may also be responsible for this finding.
The HIV prevalence among children treated for TB in this study was 29%. This is higher than the national TB/HIV co-infection rate of 22% and elsewhere in the country [9, 16]. Similar high HIV prevalence among children with TB has been reported in studies from various location in Africa [4, 17, 18]. Similar to findings of a study from Ethiopia, the TB/HIV co-infection rate varied with age; the older children had the least co-infection rate compared with the younger children in this study [4].
The overall treatment success of children notified in 2012 was 77.4%. This finding is lower than the national figure. The goal of the NTBLCP is to increase treatment success rate from 82% in 2008 to at least 85% by 2015 [8]. This finding is however higher than what was obtained in studies from other countries in Africa [19, 20] and lower than what was reported in a study from Ethiopia [4]. Differences in settings, disease presentation, prevalence of HIV infection and parental adherence to treatment have been suggested as possible explanations for the differences in treatment success [4]. In this study, risk factors such as HIV status, type of TB and gender were not associated with treatment success.
The treatment success rate among children <5 years in this study was significantly lower; death and default rate were however significantly higher compared with children >5 years. In addition, the mean age of patients with treatment success was significantly higher compared with those with poor treatment outcomes. (p = 0.004) This finding is similar to what was reported in studies from Malawi and Ethiopia [4, 12, 21]. Children <5 years are said to be at risk of death from infectious diseases including TB and also of developing TB meningitis and disseminated TB, which are often associated with high mortality because of immature immune system [22, 23]. In this study, about half of the patients that were HIV positive were <5 years. This may explain why the death rate was significantly higher in this age group.
Studies conducted in Nigeria and elsewhere in Africa have documented poor treatment outcomes of HIV-infected children treated for TB [16, 24, 25]. In this study, the death rate observed among HIV-positive children treated for TB was significantly higher than the HIV-negative children (p = 0.002). This is contrary to what was reported in a study from Botswana [7]. Contrary to a study from Nigeria, the treatment success of HIV-positive children treated for TB was comparable with those of HIV-negative children [16]. The collaboration between the NTBLCP and the HIV programme in Nigeria has led to improvement in the quality of care provided to patients with TB/HIV co-infection. Access to HIV counselling and testing among TB patients has increased the proportion of TB patients tested for HIV from 32% in 2007 to 84.5% in 2012. In addition, the proportion of TB/HIV patients placed on co-trimoxazole preventive therapy also increased from 30% in 2008 to 81% in 2012, while the proportion of TB/HIV patients on ART increased from 17% in 2008 to 57% in 2012 [8, 9]. The direct implication of this on the treatment outcomes of children with TB/HIV co-infection is difficult to ascertain because until recently, treatment outcomes of childhood TB were not disaggregated from the national data.
CONCLUSION
The number of childhood TB cases notified by the Lagos State TB programme was low. The need to intensify effort at improving notification and treatment outcomes in children, especially those <1 year in the state, cannot be over emphasized.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the Lagos State TB control officer, TB focal persons, LGA TB supervisors and the Lagos State Ministry of Health for their support.
REFERENCES
- 1.World Health Organization. Global tuberculosis report. Geneva: World Health Organization, 2013. http://www.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf (June 2015, date last accessed).
- 2.Beyers N, Gie R, Schaaf H, et al. A prospective evaluation of children under the age of 5 years living in the same household as adults with recently diagnosed pulmonary tuberculosis. Int J Tuberc Lung Dis 1997;1:38–43. [PubMed] [Google Scholar]
- 3.Starke JR. Childhood tuberculosis: ending the neglect. Int J Tuberc Lung Dis 2002;6:373–74. [PubMed] [Google Scholar]
- 4.Dereje H, Woldaregay EA, Mulugeta B. Childhood tuberculosis and its treatment outcomes in Addis Ababa: a 5-years retrospective study. BMC Pediatr 2014;14:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marais BJ, Pai M. Recent advances in the diagnosis of childhood tuberculosis. Arch Dis Child 2007;95:446–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Safdar N, Hinderaker SG, Baloch NA, et al. Diagnosis and outcome of childhood tuberculosis: implementing public health policy in three districts of Pakistan. Int J Tuber Lung Dis 2010;14:872–7. [PubMed] [Google Scholar]
- 7.Oeltmann JE, Chengeta B, Mboya JJ, et al. Reported childhood tuberculosis treatment outcomes, Gaborone and Francistown, Botswana, 1998–2002. Int J Tuberc Lung Dis 2008;12:186–92. [PubMed] [Google Scholar]
- 8.NTCLP. National Tuberculosis and Leprosy program 2011 annual report. Abuja: NTCLP, 2012a.
- 9.NTCLP. National Tuberculosis and Leprosy program 2013 annual report. Abuja: NTCLP, 2012b.
- 10.Harries AD, Hargreaves NJ, Graham SM, et al. Childhood tuberculosis in Malawi: nationwide case-finding and treatment outcomes. Int J Tuberc Lung Dis 2002;6:424–31. [PubMed] [Google Scholar]
- 11.Nelson LJ, Wells CD. Global epidemiology of childhood tuberculosis. Int J Tuberc Lung Dis 2004;8:636–47. [PubMed] [Google Scholar]
- 12.Harries AD, Hargreaves NJ, Graham SM, et al. Childhood tuberculosis in Malawi: nationwide case-finding and treatment outcomes. Int J Tuberc Lung Dis 2002;6:424–31. [PubMed] [Google Scholar]
- 13.Marais BJ, Hesseling AC, Gie RP, et al. The burden of childhood tuberculosis and the accuracy of community-based surveillance data. Int J Tuberc Lung Dis 2006;10:259–63. [PubMed] [Google Scholar]
- 14.World Health Organization. Global tuberculosis control: a short update to the 2009 report. Geneva: WHO, 2009. WHO/HTM/TB/2009.426. www.who.int/tb/publications/global_report/2009/update/tbu_9pdf (September 2015, date last accessed)
- 15.Federal Ministry of Health Department of Public Health. Report: First National TB Prevalence Survey 2012. FMOH Abuja.
- 16.Daniel OJ, Ogunfowora OB, Oladapo OT. HIV and tuberculosis co-infection in children: presentation and treatment outcome. Niger J Peadiatr 2005;32:83–7. [Google Scholar]
- 17.Iriso R, Mudido PM, Karamagi C, et al. The diagnosis of childhood tuberculosis in an HIV-endemic setting and the use of induced sputum. Int J Tuberc Lung Dis 2005;9:716–26. [PubMed] [Google Scholar]
- 18.Madhi SA, Huebner RE, Doedens L, et al. HIV-1 co-infection in children hospitalized with tuberculosis in South Africa. Int J Tuberc Lung Dis 2000;4:448–54. [PubMed] [Google Scholar]
- 19.Muň oz-sellart M, Yassin MA, Tumato M, et al. Treatment outcome in children with tuberculosis in Southern Ethiopia. Scand J Infect Dis 2009;41:450–5. [DOI] [PubMed] [Google Scholar]
- 20.Ramos JM, Reyes F, Tesfamariam A. Childhood and adult tuberculosis in a rural hospital in Southeast Ethiopia: a ten-year retrospective study. BMC Public Health 2010;10:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mtabho CM, Irongo CF, Boeree MJ, et al. Childhood Tuberculosis in the Kilimanjaro region: lessons from and for the TB Programme. Trop Med Int Health 2010;15:496–501. [DOI] [PubMed] [Google Scholar]
- 22.Swaminathan S, Rekha B. Pediatric tuberculosis: global overview and challenges. Clin Infect Dis 2010;50(Suppl. 3):S184–94. [DOI] [PubMed] [Google Scholar]
- 23.Enarson PM, Enarson DA, Gie R. Management of tuberculosis in children in low-income countries. Int J tuberc Lung Dis 2005;9:1299. [PubMed] [Google Scholar]
- 24.Hesseling AC, Westra AE, Werschkull H, et al. Outcome of HIV infected children with culture-confirmed tuberculosis. Arch Dis Child 2005;90:1171–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palme IB, Gudetta B, Bruchfeld J, et al. Impact of human immunodeficiency virus 1 infection on clinical presentation, treatment outcome and survival in a cohort of Ethiopian children with tuberculosis. Pediatr Infect Dis J 2002;21:1053–61. [DOI] [PubMed] [Google Scholar]