ABSTRACT
Background
Generalized joint laxity is more prevalent in women than men and may lead to poorer post-operative outcomes in select orthopedic populations. There are no studies examining peri-operative function in patients with generalized joint laxity (GJL) and femoroacetabular impingement (FAI).
Purpose
The purpose of this study was to determine the difference in perceived function and quality of life as measured by the Hip Outcome Score ADL subscale (HOS-ADL), International Hip Outcomes Tool (iHOT-33) and the Short Form 12-Item Health Survey (SF-12) in women with and without GJL prior to and six months after undergoing hip arthroscopy for FAI.
Study Design
Cohort Study
Methods
Peri-operative data were collected from women with FAI from November 2011-September 2014. Lax subjects were women with laxity scores ≥4/9 on the Beighton and Horan Joint Mobility Index; Nonlax subjects were women with laxity scores <4/9. Functional outcomes were evaluated using the HOS-ADL, iHOT-33, PCS-12, and the MCS-12 pre-operatively and at 6 months post-operatively. Change scores (post-score – pre-score) were calculated for each outcome measure and compared between groups, along with pre-operative and post-operative means, using Mann-Whitney U tests.
Results
166 women met the inclusion criteria: Nonlax (n = 131), Lax (n = 35). There were no statistically significant differences between groups in pre-operative functional outcomes (all p > .05). Additionally, there were no statistically significant differences between groups in post-operative means or change scores, respectively, for HOS-ADL (p = .696, .358), iHOT-33 (p = .550, .705), PCS-12 (p = .713, .191), and MCS-12 (p = .751, .082). Laxity score was not associated with any post-operative functional outcome score or change score (all p > .05).
Conclusion
Women with and without generalized joint laxity do not appear to report differences in hip function in the 6-month peri-operative period before and after hip arthroscopy for FAI.
Level of Evidence
3
Keywords: Hip arthroscopy, femoroacetabular impingement, generalized joint laxity
INTRODUCTION
Femoroacetabular impingement (FAI) is defined as aberrant contact between the proximal femur and acetabulum due to abnormal morphology of the hip joint.1 Left untreated, FAI may result in pain and disability,1 chondrolabral dysfunction,2 and future development of degenerative arthritis.3–5 Hip arthroscopy has emerged as an effective surgical management technique for FAI and associated labral pathology,4 yielding high patient satisfaction and significant improvements in patient self-reported outcome scores for the majority of patients.6–8 However, women report lower pre- and post-operative quality of life scores9 and worse functional outcomes10 compared to age-matched men. Further, female patients were the only individuals to undergo revision surgeries for continued pain and hip dysfunction in a study of outcomes post-hip arthroscopy in adolescents.10 Understanding factors related to poorer outcomes in women undergoing hip arthroscopy may help guide the most effective peri-operative clinical decisions.
Generalized joint laxity (GJL) may be one factor that explains the difference in outcomes between sexes following hip arthroscopy. The prevalence of GJL in the general population ranges from 5-20%,11 with rates as high as 33% reported in pubertal and post-pubertal highly active females.12 Importantly, the presence of GJL may predispose individuals to injury and poorer orthopedic surgical outcomes. GJL increases the risk of knee joint injury18 and specifically increases the risk of anterior cruciate ligament (ACL) injury five-fold in young female athletes.19 GJL is also related to poorer self-reported orthopedic surgical outcomes, increased joint and musculoskeletal pain, and decreased quality of life.20–22
Comprehensive pre-operative assessment provides critical information concerning patient care and surgical decision-making. The pre-surgical condition of the patient and the injured joint are known predictors of function following hip arthroscopy.8 In a cohort study of 112 adults scheduled to undergo hip arthroscopy for FAI with associated chondrolabral dysfunction, poorer self-reported function prior to surgery was associated with poorer post-operative outcomes; those individuals with lower Modified Harris Hip Scores were also more likely to undergo total hip arthroplasty following failure of hip arthroscopy.8 GJL may adversely affect peri-operative function in patients undergoing hip arthroscopy and could have important implications on peri-operative care and rehabilitation strategies.
While GJL complicates the clinical outcomes in some orthopaedic populations, the influence of GJL on peri-operative function in women with symptomatic FAI has not been previously investigated. The purpose of this study was to determine the difference in perceived function and quality of life as measured by the Hip Outcome Score ADL subscale (HOS-ADL), International Hip Outcomes Tool (iHOT-33) and the Short Form 12-Item Health Survey (SF-12) in women with and without GJL prior to and six months after undergoing hip arthroscopy. The primary hypothesis tested was that women with GJL would report significantly worse outcomes of perceived function and quality of life when compared with women without GJL pre-operatively and six months after hip arthroscopy. The second hypothesis tested was that BHJMI score would be associated with post-operative function in women six months after hip arthroscopy.
METHODS
This study was approved by the Institutional Review Board and The Ohio State University, and all subjects provided informed consent prior to participation. Self-reported outcomes data were prospectively collected on 664 consecutive patients undergoing hip arthroscopy for symptomatic FAI with and without associated labral pathology from November 2011 to May 2015. Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted by The Ohio State University.23 REDCap is a secure, web-based application designed to support data capture for research studies, providing 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.23 The current study was a retrospective, secondary analysis from this prospective cohort of subjects undergoing hip arthroscopy. Women who consented to undergo hip arthroscopy and had completed self-reported outcomes questionnaires before and six months after surgery were included in this study, regardless of arthroscopic labral management (debridement, repair, or reconstruction). Subjects who were male, underwent revisions, underwent bilateral surgeries or had a history of orthopedic surgery over the six months prior to the collection of baseline data were excluded. Symptom duration was grouped into one of three categories: 0-1 year, 1-3 years and 3 + years.
Clinical Examination
Pre-operative diagnosis of FAI was confirmed by clinical examination and imaging. All subjects underwent a pre-operative medical evaluation with the treating orthopaedic surgeon (TJE). This included the collection of demographic information, medical and surgical history, and history of current condition and symptoms; the completion of self-reported outcome questionnaires; and the completion of a physical examination including pre-operative assessment of GJL.
The diagnosis of FAI was confirmed by a combination of injury history and objective examination findings, including specific intra-articular provocation tests, hip range of motion testing and results of imaging studies. Clinical guidelines for arthroscopic management for FAI included: hip pain (primarily in the groin) that interfered with activities of daily living; radiologic evidence of FAI; cam impingement (alpha angle > 50 degrees), pincer impingement (acetabular retroversion or coxa profunda) or both; failure of conservative therapy for a duration of six months including activity modification and treatment with non-steroidal anti-inflammatory drugs; and minimal degenerative changes of the hip (Tönnis grade < 1). If necessary, intra-articular source of symptoms was confirmed by relief after injection of local anesthetic into the joint. Physical examination was performed on all subjects by the same orthopedic surgeon pre-operatively. Hip provocation testing included the flexion abduction external rotation (FABER) test and the Flexion/Internal rotation test and the hip impingement test (FADIR). Radiographs, magnetic resonance imaging (MRI) and three-dimensional (3-D) computed tomography (CT) were used in the clinical assessment and for pre-operative planning. MRI was used to confirm labral tears, evaluate joint abnormalities and assess articular damage within the joint. Subjects with significant dysplasia (Lateral Center Edge Angle (LCEA)<25 ° and Angle of Inclination (AI)>10 °) were excluded. The degree of hip osteoarthritis present on hip radiographs was determined by using the Tönnis grade classification system.24–25
GJL was assessed using the Beightonand Horan joint mobility index (BHJMI).13 The BHJMI is frequently used to evaluate the presence and degree of generalized joint laxity17 (Table 1). A cutoff score of ≥ 4 out of 9 was used based on the revised 1998 Beighton scale (Beighton criteria) and previous studies.26–27 The BHJMI demonstrates excellent inter- and intra-rater reliability in screening for GJL in women aged 15-45.14 The BHJMI has also been validated against other global joint mobility scoring systems and with passive ranges of motion of multiple joints.15–16
TABLE 1.
Beighton and Horan Joint Mobility Index11
| Joint Examination | Positive Sign | Points |
|---|---|---|
| Knee hyperextension (each side) | ≥ 10 degrees | 2 (one per side) |
| Elbow hyperextension (each side) | ≥ 10 degrees | 2 (one per side) |
| Passive thumb to anterior forearm (each side) | Thumb to forearm | 2 (one per side) |
| Passive fifth finger hyperextension (each side) | ≥ 90 degrees | 2 (one per side) |
| Standing trunk flexion with knee extension | Ability to touch the palms to the floor | 1 |
Arthroscopic Surgery and Post-Operative Rehabilitation
Subjects included in this study underwent arthroscopy to address the bony impingement and associated labral pathology with femoral neck osteoplasty, acetabuloplasty, labral repair, labral debridement, and/or anterior inferior iliac spine resection, as indicated. Details of the surgical procedure were recorded in the database for each subject in the study. Capsular closures were performed on all patients with 3-4 sutures on all patients beginning in April of 2013 (Table 2). All subjects underwent the same supervised physical therapy program following arthroscopy with a standard set of rehabilitation guidelines, which included pain-guided weight-bearing progression, use of a continuous passive motion (CPM) machine, and family member instruction in performing passive hip circumduction in the acute phase of rehabilitation. After approximately four weeks, rehabilitation focused on restoring full pain free hip range of motion with respect to tissue healing guidelines and the progression of a previously published phased exercise program that individuals performed without pain or musculoskeletal compensation.1 Compliance with rehabilitation and duration of skilled physical therapy were not recorded for this study.
TABLE 2.
Pre-Operative Subject Demographic Data and Operative Data
| Variable | Lax | Non-Lax | P-value |
|---|---|---|---|
| Number of Subjects | 35 | 131 | -- |
| Age [mean (range)], yr | 25.7 (15-53) | 33.5 (15-60) | <.001* |
| Symptom Duration, no. of subjects (percentage) | |||
| 0-1 year | 11 (31.4%) | 27 (20.6%) | .209 |
| 1-3 years | 11 (31.4%) | 57 (43.5%) | .178 |
| 3 + years | 13 (37.2%) | 47 (35.9%) | .890 |
| FAI Classification, no. of subjects (percentage) | |||
| Cam Lesion | 23 (65.7%) | 80 (61.1%) | .656 |
| Pincer Lesion | 2 (5.7%) | 5 (3.8%) | .609 |
| Combined | 8 (22.9%) | 40 (30.5%) | .347 |
| Not Defined | 2 (5.7%) | 6 (4.6%) | .793 |
| Labral Management, no. of subjects (percentage) | |||
| Labral Repair | 31 (88.6%) | 104 (79.4%) | .154 |
| Labral Reconstruction | 0 (0%) | 4 (3.1%) | .580 ¶ |
| Labral Debridement | 0 (0%) | 4 (3.1%) | .580 ¶ |
| No Labral Management | 4 (11.4%) | 19 (14.4%) | .620 |
| Impingement Management, no. of subjects (percentage) | |||
| Osteoplasty | 19 (54.2%) | 80 (61.1%) | .472 |
| Acetabular Rim Resection | 1 (2.9%) | 1 (0.8%) | .378 ¶ |
| Combined | 14 (40.0%) | 50 (38.2%) | .844 |
| None | 1 (2.9%) | 0 (0%) | .211 ¶ |
| Capsule Closure, no. of subjects (percentage) | |||
| Yes | 15 (42.9%) | 65 (50.4%) | .474 |
| No | 20 (57.1%) | 66 (49.6%) |
yr = year; no. = number;
= Independent t-test group comparison;
= Fisher exact test group comparison, due to small number of events; All additional group comparisons with Chi-Square tests
Self-Reported Functional Outcome Measures
Reliable and valid functional outcome measures were completed at the pre-surgical visit and six months after surgery. Self-reported hip function was assessed using the Hip Outcome Score ADL subscale (HOS ADL) and the International Hip Outcome Tool (iHOT-33). The HOS ADL is a 17-item subscale of the HOS pertaining to basic daily activities.28 The iHOT-33 is a 33-item visual analog scale (VAS) outcome measure recently designed for young, active patients with hip pathology.29 A higher score on the HOS-ADL and the iHOT-33 indicates better function, and scores are transformed to a scale of 0-100 percent. Additionally, both the HOS ADL and iHOT-33 are valid and reliable in assessing outcomes after hip arthroscopy for labral pathology and FAI.29–30 Quality of life was assessed using the Short Form 12-item Health Survey v.2® (SF-12) physical component summary (PCS-12) and mental component summary (MCS-12). Both components of the SF-12 are reliable and valid global function measures scored based on a norm-based mean of 50 with a standard deviation of 10.31–32
Statistical Analyses
All statistical analyses were performed using SPSS software (IBM SPSS Statistics; v. 21.0; Chicago, IL). Subjects were divided into two groups for analysis based on their BHJMI score. Female subjects with BHJMI scores ≥ 4 out of 9 were classified as ‘LAX’ and those with BHJMI scores < 4 out of 9 were classified as ‘NONLAX’. Descriptive analysis of demographic data consisted of the calculation of percentages and frequencies for categorical data and the calculation of means and ranges for continuous data. Categorical demographic data were compared between groups (between LAX and NONLAX) using Chi Square tests and using Fisher exact tests when counts per group were less than five. Continuous demographic data were compared between groups using independent t-tests. Additionally, independent t-tests were used to compare pre-surgical group differences for each functional outcome score prior to surgery for all subjects with pre-surgical data. Equal variances and normality were confirmed for all pre-operative variables compared. Change scores (six-month post-operative score – pre-operative score) were calculated for each functional outcome score.33 However, due to non-normality of the six-month post-operative data and change scores across both the LAX and NONLAX groups, six-month group means and change scores were compared between groups using independent samples Mann-Whitney U tests. Statistical significance was established a priori (α = 0.05) for all comparisons. Linear regressions were used to test the second hypothesis that BHJMI scores would be associated with post-operative functional outcome scores six months after hip arthroscopy and change scores (post-score – pre-score). In each regression, capsule closure status was controlled for, as capsule closure during hip arthroscopy has been recommended for individuals undergoing hip arthroscopy34 and was not performed in the entire cohort. Capsule closure was dichotomized (No/Yes) prior to being entered into each model. After entering capsule closure status into each model, BHJMI score was entered to evaluate its impact on both post-operative functional outcome scores and change scores. Multi-collinearity was evaluated between capsule closure status and BHJMI score with tolerance and variance inflation factors. Using an a priori significance level set at 0.05, an effect size of 0.50 (Cohen's d), power of 0.8, and the distribution of individuals with laxity in this cohort, sample size was calculated to be 140 subjects (35 LAX, and 105 NONLAX) for Mann Whitney U group comparisons. Determination of a moderate effect size (0.50) was based on differences in musculoskeletal function between lax and non-lax individuals in other orthopedic populations.20
RESULTS
Of the 664 subjects in the authors’ hip outcomes database, 224 underwent hip arthroscopy for FAI. Of these, 166 (35 LAX, 131 NONLAX) met the inclusion criteria for this study, including the collection of six-month post-operative data. (Figure 1) The LAX group was younger than the NONLAX group (p<.001) (Table 2). However, other baseline pre-operative or operative characteristics were not significantly different between groups. (Table 2) Symptom duration for subjects varied from three to six months to greater than five years. Cam type of FAI was the most prevalent bony lesion, followed by combined and isolated pincer lesions in both groups. Surgical treatment of the labrum included labral repair, labral debridement, labral reconstruction, and no labral management. (Table 2) In total, 18 subjects went on to have revision procedures (LAX, n = 4; NONLAX, n = 14) following initial index procedure. Revision procedures were agreed upon by the patient and surgeon and were based on the persistence of pain and functional limitations.
Figure 1.
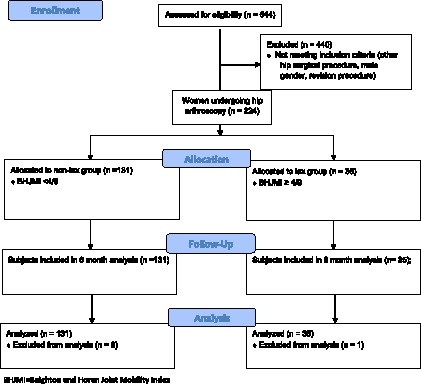
Consort Diagram.
Laxity Group Comparisons
Prior to the completion of statistical analyses, one subject was removed as an outlier from the LAX group due to having pre-operative and post-operative functional outcome scores greater than two standard deviations below the group means for two of the functional measures. Pre-operatively, there were no statistically significant differences between groups in the HOS-ADL, iHOT-33, PCS-12, or the MCS-12 (Table 3; all p ≥ .05). Post-operatively, there were no statistically significant differences in post-operative group means (p ≥ .05). or change scores on the HOS-ADL, i-HOT-33 and the PCS-12. (Tables 3, 4). Although the LAX group demonstrated greater improvements on the MCS-12 from the pre-operative to post-operative evaluation, the difference was not statistically significant (p = .082).
Table 3.
Self-reported hip function and quality of life scores prior to and six months after hip arthroscopy (N = 166; Lax = 35; Non-lax = 131)
| Outcome Measure | Pre-L | Pre-NL | P-value¶ | Post-L | Post-NL | P-value Ф |
|---|---|---|---|---|---|---|
| HOS ADL* | 60.63 (54.19, 67.06) | 60.22 (57.54, 62.90) | .895 | 81.93 (75.19, 88.67) | 82.35 (79.49, 85.21) | .696 |
| iHOT-33* | 27.90 (22.61, 33.19) | 31.52 (29.08, 33.96) | .188 | 62.04 (52.93, 71.14) | 65.71 (61.64, 69.79) | .550 |
| PCS-12* | 40.99 (37.99, 43.99) | 39.72 (38.37, 41.07) | .404 | 47.37 (43.79, 50.93) | 48.51 (46.96, 50.04) | .713 |
| MCS-12* | 46.08 (42.53, 49.63) | 49.17 (47.47, 50.87) | .104 | 52.10 (49.36, 54.84) | 52.47 (51.02, 53.92) | .751 |
HOS-ADL = Hip Outcome Score ADL subscale; iHOT-33 = International Hip Outcome Tool; PCS-12 = Short Form 12-Item Health Survey Physical Component Summary; MCS-12 = Short Form 12-Item Health Survey Mental Component Summary
= Mean (95% confidence interval); Pre-L = Pre-operative data for lax subjects; Pre-NL = Pre-operative data for non-lax subjects; Post-L = Post-operative data for lax subjects with 6 month follow-up; Post-NL = Post-operative data for non-lax subjects with 6 month follow-up;
= Independent t-test group comparisons; Ф = Mann Whitney U group comparisons;
Table 4.
Change scores for self-reported hip function and quality of life from pre- to 6 months after surgery (N = 166; Lax = 35; Non-lax = 131)
| Lax | Non-Lax | P-value Ф | |
|---|---|---|---|
| HOS ADL* | 21.29 (15.47, 27.13) | 22.13 (19.42, 24.84) | .358 |
| i-HOT-33* | 34.14 (25.19, 43.08) | 34.19 (30.15, 38.24) | .705 |
| PCS-12* | 6.37 (2.88, 9.86) | 8.79 (7.24, 10.33) | .191 |
| MSC-12* | 6.03 (3.12, 8.93) | 3.30 (1.56, 5.04) | .082 |
= Mean (95% confidence interval); Ф = Mann Whitney U group comparisons; HOS-ADL = Hip Outcome Score ADL subscale; iHOT-33 = International Hip Outcome Tool; PCS-12 = Short Form 12-Item Health Survey Physical Component Summary; MCS-12 = Short Form 12-Item Health Survey Mental Component Summary
Regression Results
Multi-collinearity among independent variables in each regression model (capsule closure status, BHJMI score) allowed both predictors to be entered into each model (Tolerance = .983; Variance inflation factor = 1.02). Neither capsule closure status nor BHJMI score were significantly associated with post-operative HOS-ADL score (p = .720, .876, respectively; R2 = .001), iHOT-33 score (p = .452, .215, respectively; R2 = .012), PCS-12 score (p = .604, .681, respectively; R2 = .002), or MCS-12 score (p = .517, .568, respectively; R2 = .005). Similarly, neither capsule closure status nor BHJMI score were significantly associated with HOS-ADL change score (p = .248, .754, respectively; R2 = .008), iHOT-33 change score (p = .391, .414, respectively; R2 = .008), PCS-12 change score (p = .196, .129, respectively; R2 = .021), or MCS-12 change score (p = .620, .391, respectively; R2 = .005). Additionally, because age was found to differ between the LAX and NONLAX group, the same models as those described above (six-month post-operative function; change scores) were evaluated with age included as an additional covariate. When including age in each model, neither capsule closure, BHJMI score, nor age were significantly associated with six-month post-operative function or change scores (all p>0.05).
DISCUSSION
The primary aim of this study was to determine differences in perceived function and quality of life in women with and without GJL prior to and six months following hip arthroscopy for FAI. Differences in self-reported hip function were not identified pre-operatively or six months after surgery, refuting our hypothesis that individuals with GJL would report poorer perioperative function than those without GJL. Statistically significant improvements in post-operative scores in hip function and quality of life from pre-operative to six months were achieved following surgery, regardless of group. Additionally, to examine the impact of BHJMI scores as a continuous variable on functional outcome scores, linear regressions were performed, revealing that severity of laxity was not associated with function at six months after arthroscopy or change scores in function from the pre-operative data collection to six month post-operatively.
The effects of laxity on function have yielded mixed results in a variety of clinical populations. In a matched comparison study of 36 healthy subjects,20 adults with GJL ( ≥ 4/9) reported significantly poorer general health and greater functional limitation measured by the KOOS. Additionally, women with GJL also demonstrated significantly lower normalized knee extension strength than women without GJL.20 In a retrospective analysis of 272 athletes undergoing ACL reconstruction,35 pre- and post-operative self-reported function were not different between those with and without GJL. In this study, knee joint laxity, rather than GJL using the BHJMI, might have been associated with lower clinical outcome scores.35 Although GJL has been identified as a factor in lower extremity injury risk19 and function,20 it does not appear to affect self-reported function in women prior to undergoing hip arthroscopy for FAI.
To the authors’ knowledge, this is the first prospective study to examine the effect of laxity on patients who undergo surgical treatment for intra-articular hip pathology. The current data indicated that self-reported hip function and quality of life in women six months after hip arthroscopy were not affected by the presence or absence of laxity. While little data exists, the lack of differences in group outcome scores may be explained by the limitations of a single post-operative follow-up and the use of a laxity score that is not specific to the hip joint. The aim of this study was to use the BHJMI to assess global tissue laxity and its effect on function. The utility of the BHJMI at predicting specific laxity at the hip is unknown. It is possible that the presence of true hip capsular and/or ligamentous laxity may differentiate individuals postoperatively, however, specific capsular and ligamentous laxity of the hip is difficulty to measure clinically.
Expectedly, these data corroborate previous findings that hip arthroscopy yields significant improvements in self-reported function in patients with intra-articular pathology;6–7,36 improvements that occurred regardless of GJL group allocation. The similarity in post-operative outcomes between subjects with and without GJL after hip arthroscopy may be attributed, in part, to the highly congruent joint surfaces of the hip joint.37 Additionally, the acetabulum has a defined concave arc of nearly 180 °, and almost entirely encompasses the spherical femoral head, contributing to excellent hip joint stability.38 These anatomic characteristics of the hip joint limit the amount of movement that is available37 and may compensate for any lack of stability resulting from lax soft tissue structures in those with GJL.
Limitations
There are several limitations of this study. This sample of subjects with GJL for the six-month post-operative analysis was small relative to the number of individuals without GJL. The subjects were selected from a large database of hundreds of consecutive patients undergoing elective hip surgery, and data collection and recruitment is ongoing. Differences in postoperative outcomes and function after hip arthroscopy have not been studied in individuals with GJL; therefore, data from other orthopaedic diagnoses with GJL justified the use of a moderate effect size for power analysis. This may have increased the likelihood of Type II error in the present study. In addition to sample size, follow up is relatively short (six months). It has been suggested that individuals with GJL may progress at slower rates than those without GJL.39 Thus, changes in self-reported function may manifest between groups if followed over a longer period of time.
Lastly, individuals with hip dysplasia were not included in this cohort. Hip dysplasia may make individuals more susceptible to the effects of laxity than those with FAI. Due to the rising interest amongst surgeons and rehabilitation specialists regarding the influence of laxity on patients with FAI, the focus of this study was exclusively on a cohort of individuals with FAI. Upcoming studies should further examine the role of bony stability and post-operative outcomes following hip arthroscopy.
Future work should examine the assessment of patient self-reported outcomes and laxity at various time points (i.e. six weeks, three months, and two years) in the post-operative period. Additionally, examining the influence of specific hip joint laxity instead of global joint laxity on outcomes after arthroscopy for FAI should also be considered. Lastly, patient-specific demographic information including duration of symptoms and psychosocial factors should be assessed to determine any relationship they may have to patient outcomes following hip arthroscopy.
CONCLUSIONS
GJL does not appear to affect self-reported hip function or quality of life in the peri-operative period before and after hip arthroscopy for FAI. Regardless of the presence or absence of GJL, all patients reported significant improvements in both hip function and quality of life after surgery. Identification of variables such as generalized joint laxity may aid clinicians in adjusting the course of post-operative care.
REFERENCES
- 1.Enseki K Harris-Hayes M White DM Cibulka MT Woehrle J Fagerson TL Clohisy JC. Orthopaedic Section of the American Physical Therapy Association: Nonarthritic hip joint pain. J Orthop Sports Phys Ther. 2014;44(6):A1-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meermans G Konan S Haddad FS Witt JD. Prevalence of acetabular cartilage lesions and labral tears in femoroacetabular impingement. Acta Orthop Belg. 2010;76(2):181-188. [PubMed] [Google Scholar]
- 3.Agricola R Waarsing J Arden N Carr A Bierma-Zeinstra S Thomas G Weinans H Glynn-Jones S. Cam impingement of the hip: A Risk factor for hip osteoarthritis. Nat Rev Rheumatol. 2013;9:630-634. [DOI] [PubMed] [Google Scholar]
- 4.Byrd J Jones K. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39:7S-13S. [DOI] [PubMed] [Google Scholar]
- 5.Ganz R Parvizi J Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120. [DOI] [PubMed] [Google Scholar]
- 6.Nho SJ Magennis EM Singh CK Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39:Suppl:14S-9S. [DOI] [PubMed] [Google Scholar]
- 7.Palmer DH Ganesh V Comfort T Tatman P. Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy. 2012;28(11): 1671-1681. [DOI] [PubMed] [Google Scholar]
- 8.Phillipon M Briggs K Yen Y Kuppersmith. Outcomes following hip arthroscopy for femoroacetabular impingement associated with chondrolabral dysfunction: a minimum of two-year follow-up. .J Bone Joint Surg Br 2009;91(1):16-23. [DOI] [PubMed] [Google Scholar]
- 9.Malviya A Stafford G Villar R. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J Bone Joint Surg Br. 2012;94-B:466-470. [DOI] [PubMed] [Google Scholar]
- 10.Phillipon MJ Ejnisman L Ellis HB Briggs KK. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012;28:1255-1261. [DOI] [PubMed] [Google Scholar]
- 11.Biro F Gewanter H Baum J. The Hypermobility Syndrome. Pediatrics. 1983;72(5):701-706. [PubMed] [Google Scholar]
- 12.Scher D Owens B Sturdivant R Moriatis J. Incidence of Joint Hypermobility Syndrome in a Military Population: Impact of Gender and Race. Clin Orthop Relat Res. 2010;468:1790-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beighton P Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969;51:444–453. [PubMed] [Google Scholar]
- 14.Boyle KL Witt P Riegger-Krugh C. Intrarater and interrater reliability of the Beighton and Horan Joint Mobility Index. J Athletic Training. 2003;38:281–285. [PMC free article] [PubMed] [Google Scholar]
- 15.Remvig L Jensen DV Ward RC. Are diagnostic criteria for general joint hypermobility and benign joint hypermobility syndrome based on reproducible and valid testsϿ. A review of the literature. J Rheumatol. 2007;34(4):798-803. [PubMed] [Google Scholar]
- 16.Smits-Engelsman B Klerks M Kirby A. Beighton Score: A Valid Measure for Generalized Hypermobility in Children. J Pediatr. 2011;158(1):119-123.e4. [DOI] [PubMed] [Google Scholar]
- 17.Wolf J Cameron K Owens B. Impact of Joint Laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg. 2011;19:463-471. [DOI] [PubMed] [Google Scholar]
- 18.Pacey V Nicholson L Adams R Munn J Munns C. Generalized joint hypermobility and risk of lower limb joint injury during sports: As systematic review with meta-analysis. Am J Sports Med. 2010;38:1487-1497. [DOI] [PubMed] [Google Scholar]
- 19.Myer GD Ford KR Paterno MV Nick TG Hewett TE. The Effects of Generalized Joint Laxity on Risk of Anterior Cruciate Ligament Injury in Young Female Athletes. Am J Sports Med. 2008;36(6):1073–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Juul-Kristensen B Hansen H Simonsen R Alkjaer T Krstensen J Jensen B Remvig L. Knee function in 10-year-old children and adults with generalized joint hypermobility. Knee. 2012;19:773-778. [DOI] [PubMed] [Google Scholar]
- 21.Rombaut L Malfait F Cools A DePaepe A Calders P. Musculoskeletal complaints, physical activity and health-related quality of life among patients with Ehlers-Danlos Syndrome hypermobility type. Disability Rehabil. 2010;16:1339-1345. [DOI] [PubMed] [Google Scholar]
- 22.Rombaut L Malfait F Wandele I Cools A Thijs Y DePaepe A Calders P. Medication, Surgery, and Physiotherapy among patients with hypermobility type of ehlers-danlos syndrome. Arch Phys Med Rehabil. 2011;92:1106-1112. [DOI] [PubMed] [Google Scholar]
- 23.Harris PA Taylor R Thielke R Payne J Gonzalez N Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clohisy JC Carlisle JC Trousdale R Kim YJ Beaule PE Morgan P Steger-May K Schoenecker PL Millis M. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467(3):666-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany, New York, NY: Springer; 1987. [Google Scholar]
- 26.Al-Rawi ZS Al-Aszawi AJ Al-Chalabi T. Joint mobility among university students in Iraq. Br J Rheumatol. 1985;24(4):326–331. [DOI] [PubMed] [Google Scholar]
- 27.Grahame R Bird H A Child A. The revised (Brighton 1998) criteria for the diagnosis of benign joint hyper-mobility syndrome. J Rheumatol; 2000;27:1777–1779. [PubMed] [Google Scholar]
- 28.Martin RL Kelly BT Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy. 2006;22(12):1304-1311. [DOI] [PubMed] [Google Scholar]
- 29.Mohtadi N Griffin D Pedersen E Chan D Safran M Parsons N Sekiya J et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: The International Hip Outcome Tool (iHOT-33). Arthroscopy. 2012;28:595-610. [DOI] [PubMed] [Google Scholar]
- 30.Martin RL Philippon MJ. Evidence of validity for the hip outcome score in hip arthroscopy. Arthroscopy. 2007;23(8):822-826. [DOI] [PubMed] [Google Scholar]
- 31.Gandek B Ware JE Aaronson NK Apolone G Bjorner JB Brazier JE Bullinger M Kaasa S Leplege A Prieto L Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1171–1178. [DOI] [PubMed] [Google Scholar]
- 32.Ware J Jr Kosinski M Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220-233. [DOI] [PubMed] [Google Scholar]
- 33.Dimitrov DM Rumrill PD Jr. Pretest posttest designs and measurement of change. Work. 2003;20(2):159-65. [PubMed] [Google Scholar]
- 34.Harris J Slikker W Gupta A McCormick F Nho S. Routine Capsular Closure During Hip Arthroscopy. Arthosco Tech. 2013;2(2):e89-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim SJ Moon HK Kim SG Chun YM Oh KS. Does Severity or Specific Joint Laxity Influence Clinical Outcomes of Anterior Cruciate Ligament Recons-truction? Clin Orthop Relat Res. 2010;468:1136–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krych A Thompson M Knutson Z Scoon J Coleman S. Arthroscopic Labral Repair Versus Selective Labral Debridement in Female Patients With Femoroacetabular Impingement: A Prospective Randomized Study. Arthroscopy. 2013;29(1):46-53. [DOI] [PubMed] [Google Scholar]
- 37.Loubert PV Zipple JT Klobucher MJ Marquardt ED Opolka MJ. In vivo ultrasound measurement of posterior femoral glide during hip joint mobilization in healthy college students. J Orthop Sports Phys Ther. 2013;43(8):534-541. [DOI] [PubMed] [Google Scholar]
- 38.Drake RL Vogl AW Mitchell AWM. Gray's Anatomy for Students. 2nd ed. Philadelphia, PA: Churchill Livingstone; 2010. [Google Scholar]
- 39.Hardin A Voight M Blackburn T, et al. The Effects of “Decelerated” Rehabilitation Following Anterior Cruciate Ligament Reconstruction on a Hyperelastic Female Adolescent: A Case Study. J Orthop Sports Phys Ther. 1997;26(1):29-34. [DOI] [PubMed] [Google Scholar]


