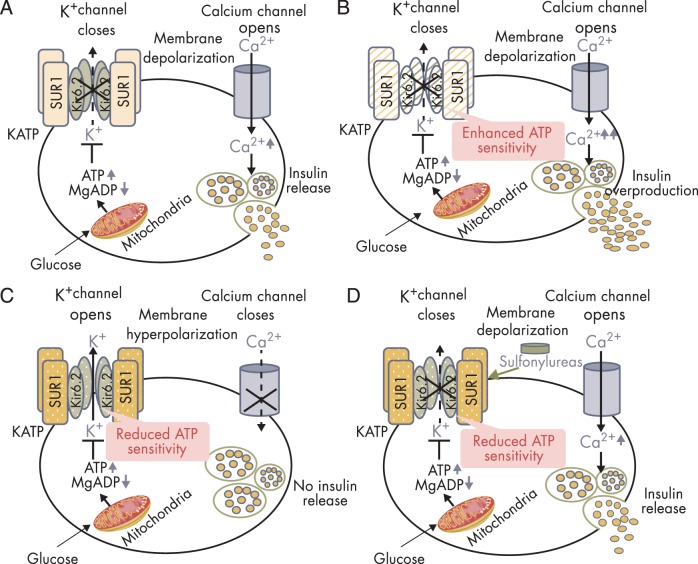
Figure 3.
Insulin secretion in normal and KATP channel mutant pancreatic β-cells. A, Glucose-stimulated insulin secretion in normal β-cells. The KATP channel is composed of four Kir6.2 subunits encoded by KCNJ11 and four SUR1 subunits encoded by ABCC8. High glucose in the circulation leads to increased glucose uptake into pancreatic β-cells. Increased intracellular glucose is metabolized via glycolytic and mitochondrial metabolism, leading to an increase in ATP production and a fall in MgADP. This results in KATP channel closure, membrane depolarization, opening of voltage-gated Ca2+ channels, Ca2+ influx, and insulin release. B, Insulin overproduction in the β-cell with KATP channel-inactivating mutations. Loss-of-function mutations in KATP channel enhances ATP binding to the channel, leading to KATP channel closure, membrane depolarization, insulin oversecretion and CHI. C, Impaired insulin secretion in the β-cell with KATP channel activating mutations. Gain-of-function mutations in KATP channel impair ATP binding to the channel Kir6.2 mutant (shown in olive green, encoded by KCNJ11), or enhance the binding of Mg-nucleotide to SUR1 mutant (shown in amber, encoded by ABCC8) leading to KATP channel opening, membrane hyperpolarization, impaired insulin release, and NDM. D, Oral sulfonylureas stimulate insulin secretion in patients with KATP channel-activating mutations. Sulfonylureas bind to the ABCC8-encoded SUR1 subunit of the KATP channel to effect channel closure independent of ATP and enable insulin secretion.