Abstract
Objective. To educate pharmacists and assess their knowledge of and ability to calculate the Drug Burden Index (DBI) using a continuing professional development (CPD) intervention.
Methods. The intervention included designing education surrounding the DBI and its application in practice and assessing knowledge in the form of a CPD education article with four multiple-choice questions (MCQs). Deidentified demographic data on participants were collected.
Results. Multiple-choice questions were completed by 2522 pharmacist participants: 97.9% of participants successfully completed the CPD assessment (answered three or four MCQs correctly), and 76.5% of participants achieved a perfect score (answered four MCQs correctly). The question that required calculation of the DBI for a fictional patient was answered correctly least often (81.8%).
Conclusion. Pharmacist participants had good knowledge of using DBI in practice; difficulty was observed in calculating the DBI for a hypothetical patient. This CPD intervention provided a practical medium for educating and assessing pharmacists’ knowledge of the DBI.
Keywords: Drug Burden Index, continuing professional development, pharmacists, education, older adults, polypharmacy
INTRODUCTION
Aging is associated with an increase in multiple chronic diseases, polypharmacy and adverse drug events.1,2 In particular inappropriate use of anticholinergic and sedative medications may contribute to poor clinical outcomes in older adults.3 Pharmacists play an important role in medication management and clinical pharmacist interventions can reduce unplanned hospital admissions.4 In Australia, consultant pharmacists can conduct home medicine reviews (HMRs), a government-funded community-based collaborative service provided by general practitioners and pharmacists. During an HMR, a patient’s medications are reviewed to ensure their optimal use.5 Recommendations provided by a pharmacist during the medication review are evidence-based and improve outcomes such as adherence and reduction in the number of falls among older adults.6-8
The Drug Burden Index (DBI) is a pharmacological risk assessment tool that measures a patient’s total exposure to medications with anticholinergic and sedative properties.9 A higher DBI is associated independently with hospitalization, frailty, falls, mortality, and impairments in function necessary for independent living in older adults.10 The DBI is a valuable clinical tool in practice that optimizes health outcomes through reducing anticholinergic and sedative exposure in older adults.11 Two retrospective analyses identified a significant reduction in DBI exposure for patients following recommendations provided by a consultant pharmacist’s medication review.12,13 However, evidence on recommendations regarding changes to sedative and anticholinergic medications and their impact on health outcomes in older adults is limited.14,15 Therefore, training health care practitioners, especially pharmacists, is necessary to translate this tool into clinical practice.
In Australia, since the establishment of the Australian Health Practitioner Regulation Agency (AHPRA) in 2010, pharmacists in all Australian jurisdictions have a mandatory requirement to complete continuing professional development (CPD) to meet state and federal licenses to practice, comparable to continuing education (CE) in the United States.16,17 The agency defines CPD as the means by which members of the profession continue to improve and broaden their knowledge, expertise, and competence, and develop personal and professional qualities throughout their professional lives.18 In Australia, CPD is self-directed, practitioner-centered, and emphasizes practice-based learning, while CE is one component of the CPD model.19 This makes CPD education an appropriate avenue for implementation and translation of research tools into practice. Most pharmacists prefer educational resources that are easily accessible at convenient times.20 The improvement in pharmacists’ professional practice is dependent on the form of CPD they undertake. For instance, CPD delivered as multi-interventional educational meetings can improve professional practice and health care outcomes for patients, but may not be effective for changing complex behaviors.21 In contrast, printed educational material may have a small beneficial effect on professional practice outcomes, though little is known about its impact on patient outcomes or behavioral change.22 Targeted educational interventions improve evidence-based practice skills and knowledge.23
An interventional study using CPD education to investigate pharmacists’ knowledge and application of the DBI as a clinical risk assessment tool in older adults has not been conducted previously. The objectives of this study were to: (1) educate pharmacists and assess their knowledge of and ability to calculate the DBI to optimize medications for older adults, using a CPD education article; and (2) explore associations between pharmacist participant demographics and assessment performance.
METHODS
The intervention included a CPD education article published in Australian Pharmacist, the main professional journal of The Pharmaceutical Society of Australia (PSA).24 Articles in this journal are independently researched, compiled by the PSA, and peer reviewed. At the time of publication, there were 27 226 registered pharmacists in Australia.25
The intervention article was designed to address the issues identified by Grol et al as influencing the uptake of evidence to practice: attributes of evidence, barriers, and facilitators to changing practice and effectiveness of dissemination and implementation strategies.26 The intervention included topics surrounding the principles, evidence for, and application of the DBI in older adults, and related topics such as polypharmacy and deprescribing (the process of withdrawal of an inappropriate medication, supervised by a health care professional with the goal of managing polypharmacy and improving outcomes), and was defined in the education article in the context of implementing DBI in practice.27-29 The article included a fictional case study designed to elicit discussion of actions and recommendations following a HMR and to assess the calculation of DBI, to address barriers, facilitators, and implementation.
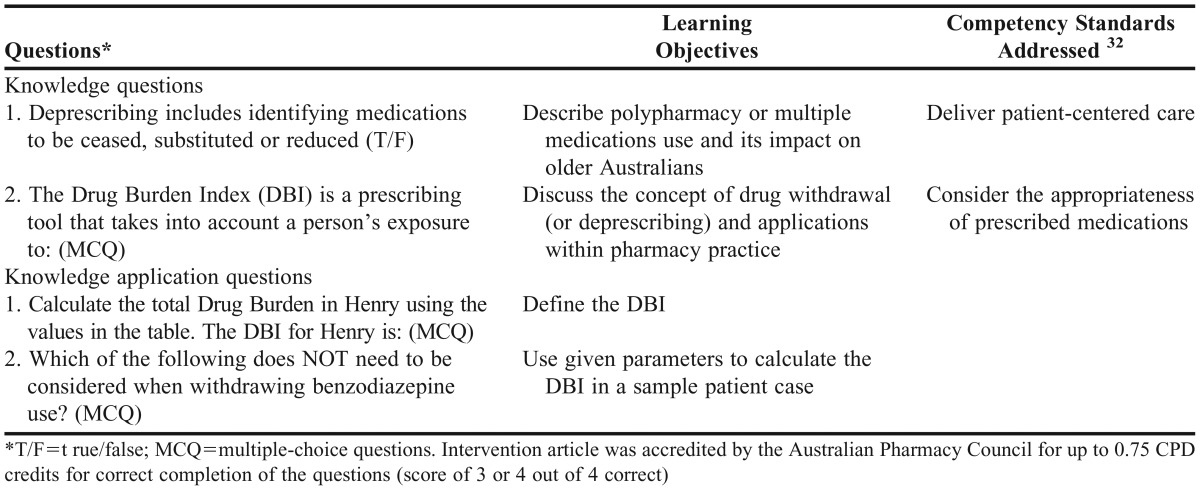
Four multiple-choice questions (MCQs) were used to measure knowledge and application of knowledge pertaining to the DBI. These questions were reviewed by the PSA and mapped to competency standards for the pharmacy profession (Table 1). Responses to the questions were entered by pharmacist participants through a password-protected website (Pharmaceutical Society of Australia, Deakin, ACT, Australia) and participants were able to claim CPD credits for scoring three or four out of four MCQs correctly. In this study, a perfect score was defined as four correct responses out of four MCQs.
Table 1.
The Four Questions, Learning Objectives, and Competency Standards Addressed by Completing the Continuing Professional Development (CPD) Activity
Ethical approval was obtained from the Northern Sydney Local Health District and the University of Sydney Human Research Ethics Committees to collect deidentified information relating to the pharmacist participants who answered the MCQs. Data were collected over two months (March to May 2013) and included participant demographics (eg, age, gender), suburb/district of practice, main field of pharmacy practice (eg, community, hospital consultancy, other), pharmacist consultant status, and responses to the MCQs. Suburb/district of practice was defined using the Pharmacy Access/Remoteness Index of Australia (PhARIA), which is designed to provide a comprehensive, standardized measurement of the physical and professional remoteness of pharmacies throughout Australia.30 The PhARIA categories are divided into a six classifications: highly accessible, accessible group A and B, moderately accessible, remote, and very remote. A consultant pharmacist is formally trained and annually accredited to conduct medication management reviews, such as HMR.
Descriptive characteristics were summarized using means, standard deviations (SD), and proportions. Multivariate logistic regression analyses were used to estimate the odds ratios (OR) and 95% confidence interval (CI) to investigate the associations between scoring of questions (categorical) and demographic characteristics. In this sample, scoring in questions was tested as a categorical variable (pass: scoring 3 or 4 out of 4 vs fail: scoring 0, 1, or 2 out of 4; nonperfect: scoring 0,1,2,3 vs perfect: scoring 4 out of 4). Data were analyzed using Microsoft Excel and SPSS, v21 (IBM, Armonk, NY).
RESULTS
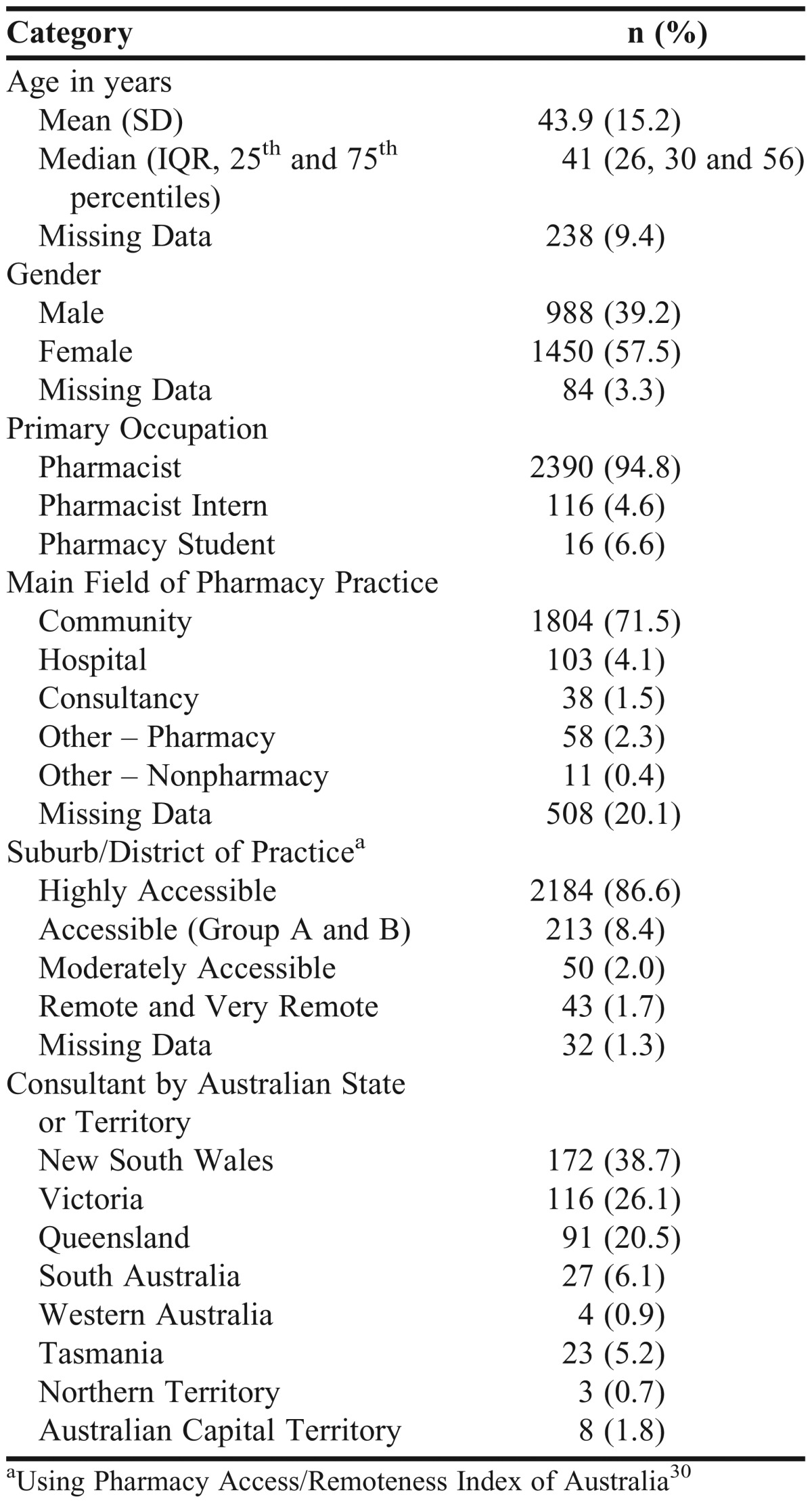
A sample of 2522 individuals completed the four MCQs associated with the intervention article, which represented 9.3% of Australian registered pharmacists (or ∼17% PSA members). The mean age (SD) of the participants was 44 (15) years. Most participants were female (57.5%), and 94.8% were qualified pharmacists, with the majority practicing in the community (71.5%) (Table 2). There was no significant difference between the study sample and national population data on pharmacists for age or gender. There was a significantly higher proportion of participants in the sample from highly accessible suburbs/districts of practice (p<0.05).
Table 2.
Summary of Demographic Characteristics of Participants
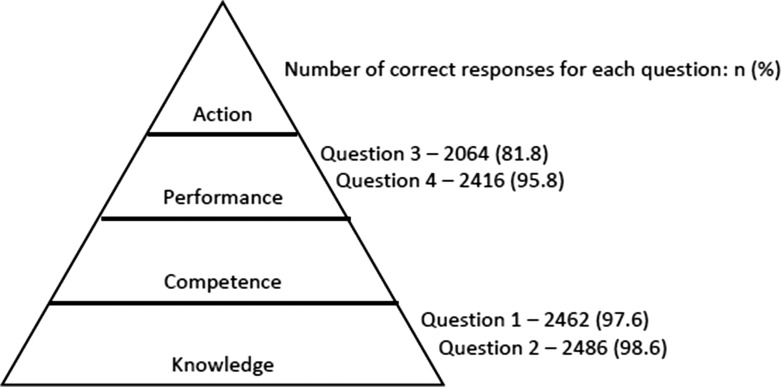
Nearly all participants (97.9%) passed (scored 3 or 4 out of 4), and 76.5% achieved a perfect score (Table 3). The lowest scoring question was question 3 (calculation of the DBI for patient case, 81.8%). There was no difference between scoring correctly on the knowledge or application questions (Figure 1). In the adjusted model, adjusting for age, gender, consultancy status, and suburb/district of practice, there was no significant relationship between demographic characteristics and whether participants scored a perfect vs nonperfect score, or whether participants passed or failed (Table 4).
Table 3.
Summary of the Scoring for the Four Multiple-Choice Questions
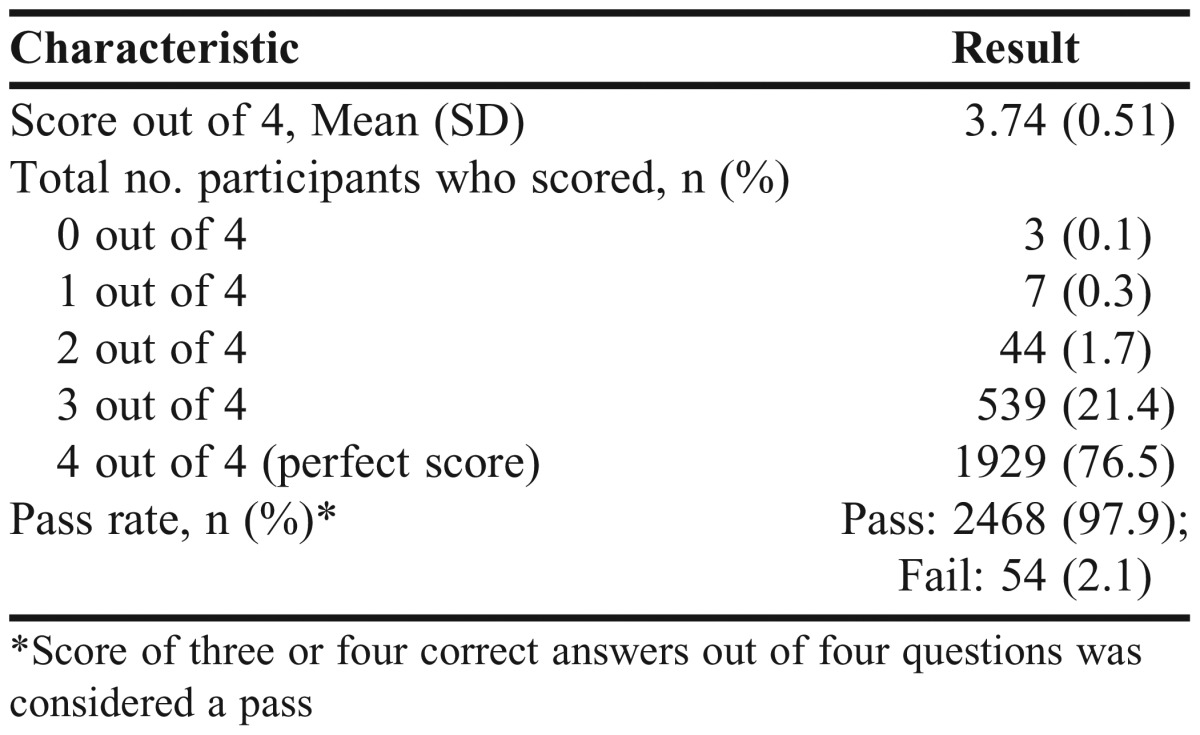
Figure 1.
The number of correct responses for each question mapped to Miller's triangle of clinical competence. Adapted from Miller 1990.33
Table 4.
Multivariate Logistic Regression to Investigate Relationships between Demographics and Whether a Participant Would Obtain a Perfect (4 out of 4) Score
DISCUSSION
This is the first study to use CPD education as an intervention to educate and assess pharmacists on the clinical use of the DBI in older adults. Pharmacists demonstrated good knowledge of the DBI, with the majority of participants passing the CPD assessment, which consisted of knowledge and application-based questions (97.9%). Even though the majority of participants passed, 76.5% obtained a perfect score, which may be predominately explained by difficulty in calculating the DBI for the hypothetical patient (81.8% of participants calculated DBI correctly, Figure 1). This may limit the future application of the research tool into clinical practice and to overcome this, an electronic calculator may facilitate the correct calculation of the DBI.31
The four questions were mapped to the National Competency Standards Framework for Pharmacists in Australia.32 For each domain of competence, Miller proposed a framework that argues there are four levels at which a medical learner should be assessed.33 Pharmacist participants demonstrated good DBI knowledge, but participants did not perform as well with questions assessing performance (or “shows how” level) (Figure 1). This highlights that this form of CPD assessment may be more suited for assessing knowledge-based questions, while performance-based questions would be best assessed perhaps in face-to-face or online interactive forms of learning.
There were no demographic predictors of scoring for CPD assessment although previous studies have observed associations between gender, age, and desire to learn with examination performance.34,35 The demographic data this study captured were limited, which may have restricted further analyses of covariates that could have predicted scoring for a CPD assessment, such as attendance at educational meetings.21
Our finding that CPD assessment in a peer-reviewed journal is an appropriate method for educating pharmacists is consistent with those of McNamara et al,36 in which pharmacists in focus groups considered evidence-based education from reliable sources essential. In our study, we used the CPD assessment method, which is carried out by the practitioner over a period of time suited to them. Self-paced learning activities satisfy the needs of health care professional learning.37 Furthermore, structured journal continuing education articles with associated examination is common practice, cost-effective (compared with attending a conference), convenient, and has the potential of reaching a large number of health professionals over a wide geographical area, as demonstrated by our 17% response rate.38 Likewise, a CPD approach was shown to implement practice changes identified in learning activities.39
A strength of this study was that it included a large population (9.3% of Australian registered pharmacists), and the sample participating in the CPD activity was representative of nationally registered pharmacists in terms of age and gender.25 There was a strong theoretical framework for the intervention article,24 which was written to address three key points as outlined by Grol et al26 to change practice and implement evidence for patient care. Grol et al further outlined that educational materials may be effective if they are continuous and interactive, and CPD should be built into patient care as clinical decision-support tools and real-time, patient-specific reminders.
There were some limitations to our study. The accuracy and completeness of the data were beyond the control of the investigators, as an external database was used. This resulted in missing data, which may have influenced results of the regression analyses (age and gender data missing for 238 (9%) and 84 (3%) participants, respectively (Table 2). Selection bias may have also occurred as pharmacists may have chosen to participate because they were interested in the content and issues outlined in the article, or because they thought that they had a knowledge deficit in the area. Furthermore, we could not determine whether the knowledge and understanding required to answer the CPD questions correctly were derived from the article or from other sources, making it difficult to conclude the direct impact of the CPD intervention on this area of pharmacy practice. Additionally, we could not evaluate the effect of the CPD article on increasing knowledge or long-term knowledge change, which would be better established through a randomized study, similar to the methodology used by Salter et al.40
Another limitation to this study was that the primary outcome was knowledge and application, not change in practice or patient outcomes. Tests of knowledge alone are insufficient to properly assess translation of knowledge and skills into practice.41 Education can be considered part of a comprehensive risk management strategy to overcome high-risk prescribing.42 Pharmacists who previously participated in CPD reported more often that their perceptions of pharmacy practice improved.43 Furthermore, printed education materials have a small beneficial effect on practice outcomes.22 Our study was one-dimensional (using one style of education), and previous studies showed that multimethod, multiphased CPD has potential for the greatest impact on practitioner behavior.44,45
CONCLUSION
Continuing professional development education was an easily accessible method for delivering education to pharmacists on the use of the DBI for older adults. Pharmacist participants demonstrated good knowledge and understanding of the DBI, however this CPD intervention method was not suited to assessing performance level of competency. Future studies may use this method as a component of multimethod training for educating health care professionals on translating DBI and other research into practice, and ultimately in multi-interventional studies that examine changes in patient outcomes.
ACKNOWLEDGMENTS
The authors acknowledge Andrew Daniels, editor of Australian Pharmacist, and Jan Ridd of the Pharmaceutical Society of Australia. The authors gratefully acknowledge the funding support from the Geoff and Elaine Penney Ageing Research Unit. Lisa Kouladjian was supported by the Australian NHMRC Primary Healthcare Scholarship. Danijela Gnjidic was supported by the Australian NHMRC Early Career Fellowship.
REFERENCES
- 1.Boparai MK, Korc-Grodzicki B. Prescribing for older adults. Mt Sinai J Med. 2011;78(4):613–626. doi: 10.1002/msj.20278. [DOI] [PubMed] [Google Scholar]
- 2.Colley CA, Lucas LM. Polypharmacy: the cure becomes the disease. J Gen Intern Med. 1993;8(5):278–283. doi: 10.1007/BF02600099. [DOI] [PubMed] [Google Scholar]
- 3.Bell JS, Mezrani C, Blacker N, et al. Anticholinergic and sedative medicines – prescribing considerations for people with dementia. Aust Fam Physician. 2012;41(1-2):45–49. [PubMed] [Google Scholar]
- 4.Thomas R, Huntley AL, Mann M, et al. Pharmacist-led interventions to reduce unplanned admissions for older people: a systematic review and meta-analysis of randomised controlled trials. Age Ageing. 2014;43(2):174–187. doi: 10.1093/ageing/aft169. [DOI] [PubMed] [Google Scholar]
- 5.Community Pharmacy Agreement. Home medicines review. http://5cpa.com.au/programs/medication-management-initiatives/home-medicines-review/. Accessed 10/07/13.
- 6.Castelino RL, Bajorek BV, Chen TF. Are interventions recommended by pharmacists during Home Medicines Review evidence-based? J Eval Clin Pract. 2011;17(1):104–110. doi: 10.1111/j.1365-2753.2010.01375.x. [DOI] [PubMed] [Google Scholar]
- 7.Hatah E, Braund R, Tordoff J, Duffull SB. A systematic review and meta-analysis of pharmacist-led fee-for-services medication review. Br J Clin Pharmacol. 2014;77(1):102–115. doi: 10.1111/bcp.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zermansky AG, Alldred DP, Petty DR, et al. Clinical medication review by a pharmacist of elderly people living in care homes – randomised controlled trial. Age Ageing. 2006;35(6):586–591. doi: 10.1093/ageing/afl075. [DOI] [PubMed] [Google Scholar]
- 9.Hilmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781–787. doi: 10.1001/archinte.167.8.781. [DOI] [PubMed] [Google Scholar]
- 10.Kouladjian L, Gnjidic D, Chen TF, Mangoni AA, Hilmer SN. The Drug Burden Index in older adults: theoretical and practical issues. Clin Interv Aging. 2014;9:1503–1515. doi: 10.2147/CIA.S66660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faure R, Dauphinot V, Krolak-Salmon P, Mouchoux C. A standard international version of the Drug Burden Index for cross-national comparison of the functional burden of medications in older people. J Am Geriatr Soc. 2013;61(7):1227–1228. doi: 10.1111/jgs.12343. [DOI] [PubMed] [Google Scholar]
- 12.Castelino RL, Hilmer SN, Bajorek BV, Nishtala P, Chen TF. Drug Burden Index and potentially inappropriate medications in community-dwelling older people: the impact of Home Medicines Review. Drugs Aging. 2010;27(2):135–148. doi: 10.2165/11531560-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Nishtala PS, Hilmer SN, McLachlan AJ, Hannan PJ, Chen TF. Impact of residential medication management reviews on drug burden index in aged-care homes: a retrospective analysis. Drugs Aging. 2009;26(8):677–686. doi: 10.2165/11316440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 14.He Z, Ball PA. Can medication management review reduce anticholinergic burden (ACB) in the elderly? Encouraging results from a theoretical model. Int Psychogeriatr. 2013;25(9):1425–1431. doi: 10.1017/S1041610213000872. [DOI] [PubMed] [Google Scholar]
- 15.Leikola SN, Virolainen J, Tuomainen L, Tuominen RK, Airaksinen MS. Comprehensive medication reviews for elderly patients: findings and recommendations to physicians. J Am Pharm Assoc. 2012;52(5):630–633. doi: 10.1331/JAPhA.2012.10163. [DOI] [PubMed] [Google Scholar]
- 16.Buxton EC, Burns EC, De Muth JE. Professional development webinars for pharmacists. Am J Pharm Educ. 2012;76(8) doi: 10.5688/ajpe768155. Article 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tran D, Tofade T, Thakkar N, Rouse M. US and international health professions' requirements for continuing professional development. Am J Pharm Educ. 2014;78(6) doi: 10.5688/ajpe786129. Article 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pharmacy Board of Australia. Continuing professional development standard. http://www.pharmacyboard.gov.au/documents/default.aspx?record=WD10%2f190&dbid=AP&chksum=bqZ4vUXTRO1MrlvK8V%2boyA%3d%3d; Accessed June 8, 2013.
- 19.Rouse MJ. Continuing professional development in pharmacy. J Am Pharm Assoc. 2004;44(4):517–520. doi: 10.1331/1544345041475634. [DOI] [PubMed] [Google Scholar]
- 20.Clifford RM, Ram PL, Lakos A, et al. Post-registration learning trends of community pharmacists. J Pharm Prac Res. 2011;41(3):203–207. [Google Scholar]
- 21.Forsetlund L, Bjorndal A, Rashidian A, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009;(2) doi: 10.1002/14651858.CD003030.pub2. CD003030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giguere A, Legare F, Grimshaw J, et al. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;10 doi: 10.1002/14651858.CD004398.pub3. CD004398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baker R, Camosso-Stefinovic J, Gillies C, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD005470.pub2. (3):CD005470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kouladjian L. The Drug Burden Index: a new tool for HMRs? Australian Pharmacist. 2013;32(3):52–55. [Google Scholar]
- 25.AHPRA. Australian Health Practitioner Regulation Agency Pharmacy Board of Australia. Pharmacy Registrant Data March 2013. www.pharmacyboard.gov.au.
- 26.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362(9391):1225–1230. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 27.Woodward MC. Deprescribing: achieving better health outcomes for older people through reducing medications. J Pharm Prac Res. 2003;33(4):323–328. [Google Scholar]
- 28.Frank C. Deprescribing: a new word to guide medication review. CMAJ. 2014;186(6):407–408. doi: 10.1503/cmaj.131568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of “deprescribing” with network analysis: implications for future research and clinical practice. Brit J Clin Pharm. 2015;80(6):1254–1268. doi: 10.1111/bcp.12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pharmacy Access/Remoteness Index of Australia. http://www.adelaide.edu.au/apmrc/research/projects/pharia/pharia-info.html. Australian Population and Migration Research Centre: The University of Adelaide.
- 31.Kouladjian L, Gnjidic D, Chen T, Hilmer SN. PP009 – Development, validation and usability of software to calculate the drug burden index: A pilot study. Clin Therap. 2013;35(8):e19. [Google Scholar]
- 32.National Competency Standards Framework for Pharmacists in Australia. http://www.psa.org.au/download/standards/competency-standards-complete.pdf. Pharmaceutical Society of Australia. [DOI] [PubMed]
- 33.Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9):S63–S67. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 34.McCall KL, MacLaughlin EJ, Fike DS, Ruiz B. Preadmission predictors of PharmD graduates' performance on the NAPLEX. Am J Pharm Educ. 2007;71(1) doi: 10.5688/aj710105. Article 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanson AL, Bruskiewitz RH, DeMuth JE. Pharmacists' perceptions of facilitators and barriers to lifelong learning. Am J Pharm Educ. 2007;71(4) doi: 10.5688/aj710467. Article 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Namara KP, Duncan GJ, McDowell J, Marriott JL. Community pharmacists' preferences for continuing education delivery in Australia. J Cont Educ Health Prof. 2009;29(1):52–57. doi: 10.1002/chp.20006. [DOI] [PubMed] [Google Scholar]
- 37.Suggs PK, Rose L, Mittelmark MB. Continuing education in geriatrics/gerontology: the critical factors. J Cont Educ Health Prof. 1993;13(2):149–157. [Google Scholar]
- 38.De Muth JE, Weinswig MH. Learners' evaluations of an accredited continuing education course in a pharmacy journal. Möbius: J Cont Educ Prof Health Sci. 1984;4(2):12–19. [Google Scholar]
- 39.Trewet CB, Fjortoft N. Evaluation of the impact of a continuing professional development worksheet on sustained learning and implementing change after a continuing pharmacy education activity. Res Social Adm Pharm. 2013;9(2):215–221. doi: 10.1016/j.sapharm.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 40.Salter SM, Vale S, Sanfilippo FM, Loh R, Clifford RM. Long-term effectiveness of online anaphylaxis education for pharmacists. Am J Pharm Educ. 2014;78(7) doi: 10.5688/ajpe787136. Article 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamarudin G, Penm J, Chaar B, Moles R. Educational interventions to improve prescribing competency: a systematic review. BMJ Open. 2013;3(8) doi: 10.1136/bmjopen-2013-003291. e003291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hilmer SN, Gnjidic D. Rethinking psychotropics in nursing homes. Reply. Med J Aust. 2013;199(2) doi: 10.5694/mja13.10353. Article 99. [DOI] [PubMed] [Google Scholar]
- 43.McConnell KJ, Newlon CL, Delate T. The impact of continuing professional development versus traditional continuing pharmacy education on pharmacy practice. Ann Pharmacother. 2010;44(10):1585–1595. doi: 10.1345/aph.1P161. [DOI] [PubMed] [Google Scholar]
- 44.Hurst D. Multifaceted and mixed didactic-interactive methods are more effective ways to learn and change behaviour. Evid Based Dent. 2013;14(3):67–68. doi: 10.1038/sj.ebd.6400944. [DOI] [PubMed] [Google Scholar]
- 45.Sarayani A, Rashidian A, Gholami K, Torkamandi H, Javadi M. Efficacy of continuing education in improving pharmacists' competencies for providing weight management service: three-arm randomized controlled trial. J Contin Educ Health Prof. 2012;32(3):163–173. doi: 10.1002/chp.21141. [DOI] [PubMed] [Google Scholar]