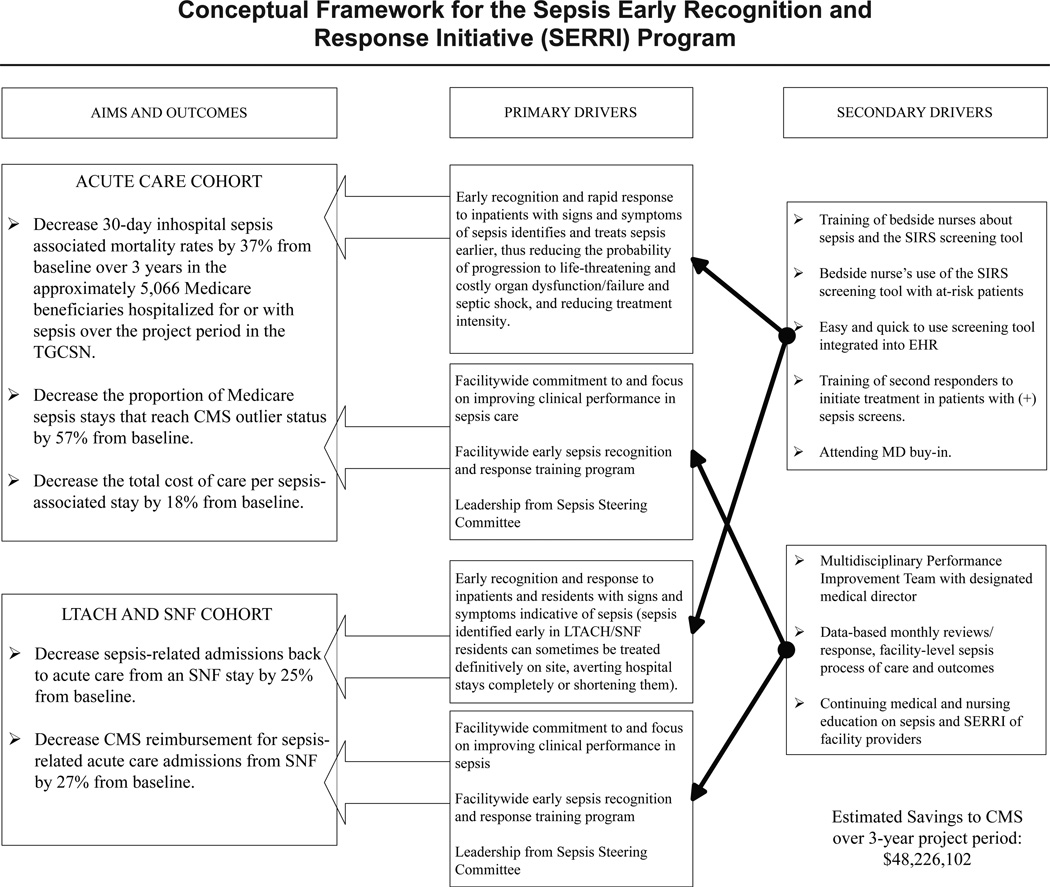
Figure 1.
SERRI’s conceptual framework is shown, along with the projected impacts on lives saved and costs avoided in the acute care cohort, which were extrapolated from the convener hospital (Houston Methodist Hospital) experience from 2009 through 2011. Projected outcomes for the postacute care sites were based on 2011 data provided by 14 such sites (not all of which elected to be SERRI participants) showing that, per 1,000 long term acute care hospitals (LTACHs), and skilled nursing facilities (SNFs) stays of Medicare beneficiaries, there were 200 returns to acute care hospitals within 30 days of LTACH and SNF admission, and that nearly two thirds were due to suspected sepsis. As the figure shows, a set of primary and secondary drivers was projected to reduce from their respective baselines the following: (1) in the acute care cohort, inpatient sepsis death rates by 37%, the proportion of sepsis-associated Medicare stays reaching high-cost outlier status by 57%, and the total cost of care per sepsis-associated stay by 18%; and (2) in the postacute care cohort, sepsis-associated returns to acute care hospitals from LTACHs and SNFs by 25%, and Centers for Medicare & Medicaid Services (CMS) reimbursement for sepsis-associated acute care admissions from LTACHs and SNFs by 27%. SIRS, systemic inflammatory response syndrome (a manifestation of early sepsis); TGCSN, Texas Gulf Coast Sepsis Network; EHR, electronic health record.