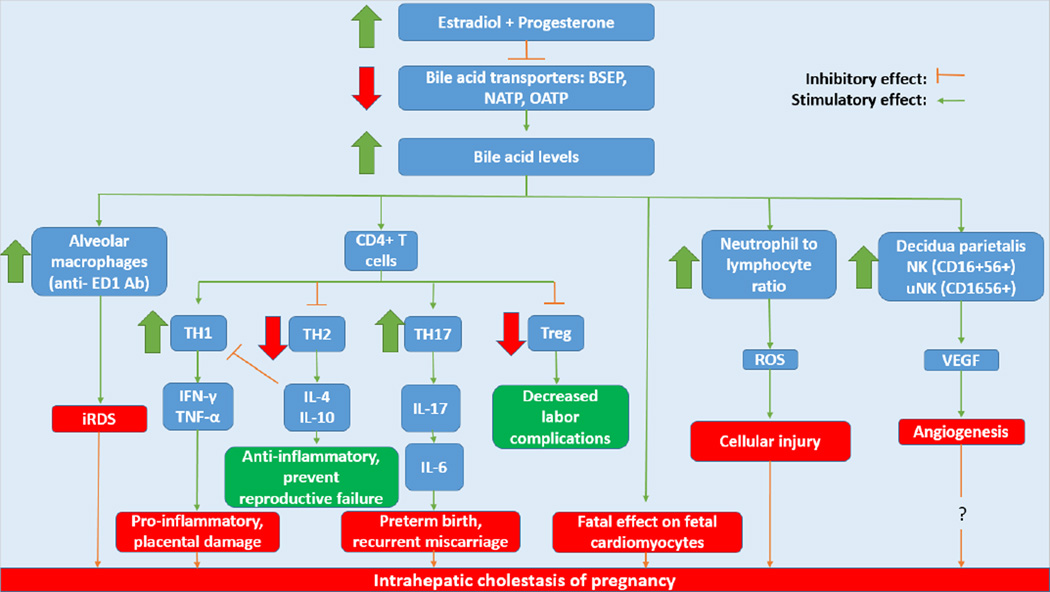
Figure 2. Immunologic changes occurring in intrahepatic cholestasis of pregnancy.
The rise in estradiol and progesterone in the third trimester of pregnancy modulates immune cells including macrophages, CD4+ T cells, neutrophils and NK cells via increases in bile acids. The increase in bile acid levels lead to increased activation of alveolar macrophages which have been implicated in infant respiratory distress syndrome, one of the fetal risks involved this disorder. Changes occur in the differentiation of CD4+ T cells. TH1 cell proliferation becomes increased and secrete pro-inflammatory cytokines such as IFN-γ and TNF-α that cause placental damage. TH2 cells which secrete anti-inflammatory IL-4 and IL-10 are decreased along with T-regulatory cells which have been shown to decrease the incidence of labor complications. Meanwhile TH17 cells produce IL-17 which induces the production of IL-6, a cytokine shown to cause preterm birth and recurrent miscarriage when at increased levels. Neutrophils, which are increased, create ROS that cause cellular injury. Finally, NK and uNK cells secrete VEGF, a factor that causes angiogenesis. While VEGF is increased in ICP, other angiogenic factors are decreased thus questioning the role of angiogenesis in intrahepatic cholestasis of pregnancy.
BSEP: Bile Salt Export Pump; NATP: Na+/taurocholate co-transporter; OATP: Organic anion transporting polypeptides; iRDS: Infant respiratory distress syndrome; Treg: T-regulatory cells; ROS: Reactive oxygen species; NK: Natural killer cells; uNK: Uterine natural killer cells; VEGF: Vascular endothelial growth factor.