Figure 2. Trend of proteinuria and renal function in red-haired nephrotic patients upon ACTH monotherapy.
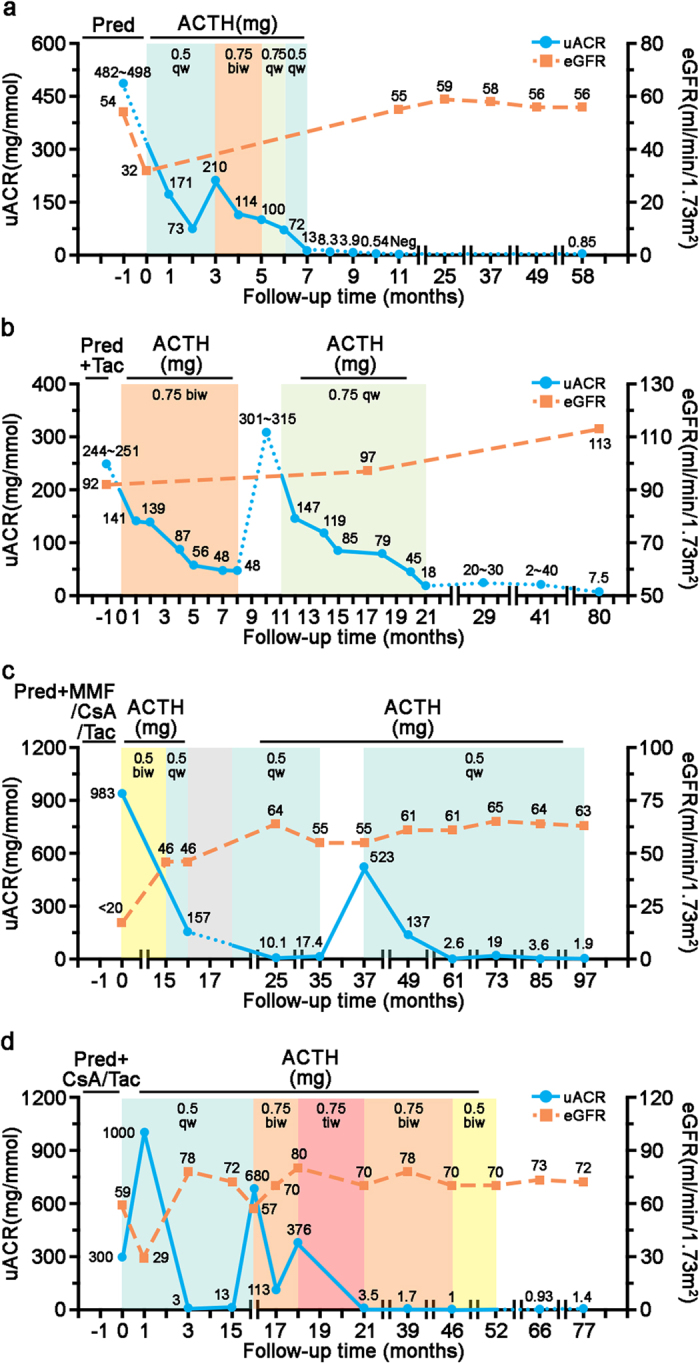
(a) Patient 1 with iMN had been refractory to prednisolone (Pred). ACTH was given at an initial dose of 0.5 mg once a week (qw) with progressive reduction in proteinuria. When a rebound of proteinuria was noted, the dose of ACTH was increased to 0.75 mg twice a week (biw) for 2 months, paralleled by further improvement of nephrotic syndrome. The patient was maintained on ACTH for another 2 months at a reduced dose (0.5 mg once a week), and a complete remission was achieved. He was followed up for more than 4 years with sustained remission and stable kidney function as shown by estimated glomerular filtration rate (eGFR). (b) Patient 2, diagnosed with iMN, was resistant to prednisolone plus tacrolimus (Tac). ACTH monotherapy was initiated with progressive improvement in proteinuria. A rapid relapse of nephrotic syndrome ensued when ACTH treatment was discontinued 8 months later. Subsequently, ACTH therapy was reinstated at a lower dose until complete remission was achieved. She was followed up for more than 5 years without relapse. (c) Patient 3, diagnosed with FSGS, was changed to ACTH monotherapy after suspected calcineurin nephrotoxicity. A dose reduction after ACTH therapy for 3 years resulted in a severe relapse. To date, this patient has maintained complete remission with a low-dose ACTH. ACTH treatment was paused for 2 month (grey area) due to pulmonary infection. (d) Patient 4, diagnosed with FSGS, remitted quickly in 3 months after initiation of ACTH. The dose was later escalated two times upon two episodes of relapse. ACTH was tapered off slowly over a period of 31 months. After stopping ACTH, this patient was followed up for over 2 years without relapse. All patients were simultaneously treated with ACEI or ARB and they tolerated ACTH therapy very well, except that patient 3 experienced one episode of fungal lung infection (Fig. 2c, grey area). MMF, mycophenolate mofetil; CsA, cyclosporine A.
