Abstract
Although intravenous drug users report the breaking of a needle as a relatively common occurrence, central embolism of needle fragments occurs infrequently in the literature. Central needle embolism also poses a conundrum for the radiologist, as the needle may be easily overlooked when the clinical history is nonspecific. We present two cases of needle embolism to the lung, one complicated by inflammatory mass and progressive pleuritic chest pain requiring wedge resection. We hope that our experiences may increase radiologists’ and emergency physicians’ familiarity with this unusual cause of chest pain. The radiological findings are subtle and may be easily overlooked, particularly without thorough clinical history.
Abbreviations: CT, computed tomography; IVDU, intravenous drug use
Introduction
Complications of intravenous drug use (IVDU) pose a significant public health burden, with the number of drug-related emergency room visits on the rise in recent years (1). The global prevalence of IVDU has been estimated at 21 million users annually, with the United States accounting for more than 40% of all cases (2). Although intravenous drug users report the breaking of a needle as a relatively common occurrence (3), only fourteen cases appear in the literature, dating back to 1985 (4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16).
To date, there have been no reported delayed complications of needle fragments embolizing to the lung; therefore, this condition has been presumed to follow a benign course. However, to our knowledge, one of our two cases is the first reported case of complications related to pulmonary needle embolism. Through our experiences and a review of the literature, we hope to increase radiologists’ and emergency physicians’ familiarity with this unusual entity.
Case report 1
A 28-year-old man with a five-year history of IVDU had recently begun keeping a needle in each groin for durable venous access. On the morning of presentation, he awoke and found that his right-sided needle was missing. Approximately 30 minutes later, the patient developed right-sided chest pain and dyspnea. He immediately presented to a community emergency department, where chest radiographs demonstrated a needle in the right lung (Fig. 1). Upon transfer to our institution, a CT of the chest confirmed the presence of a needle in the lateral segment of the right lower lobe with both intravascular and intraparenchymal components (Fig. 2). By this time, his symptoms had resolved. Vital signs and EKG were normal, and he was discharged following a brief period of observation. At two-week followup, he remained asymptomatic, and repeated chest radiographs demonstrated essentially no migration of the needle. A plan for conservative management was established, but the patient was lost to followup.
Figure 1.
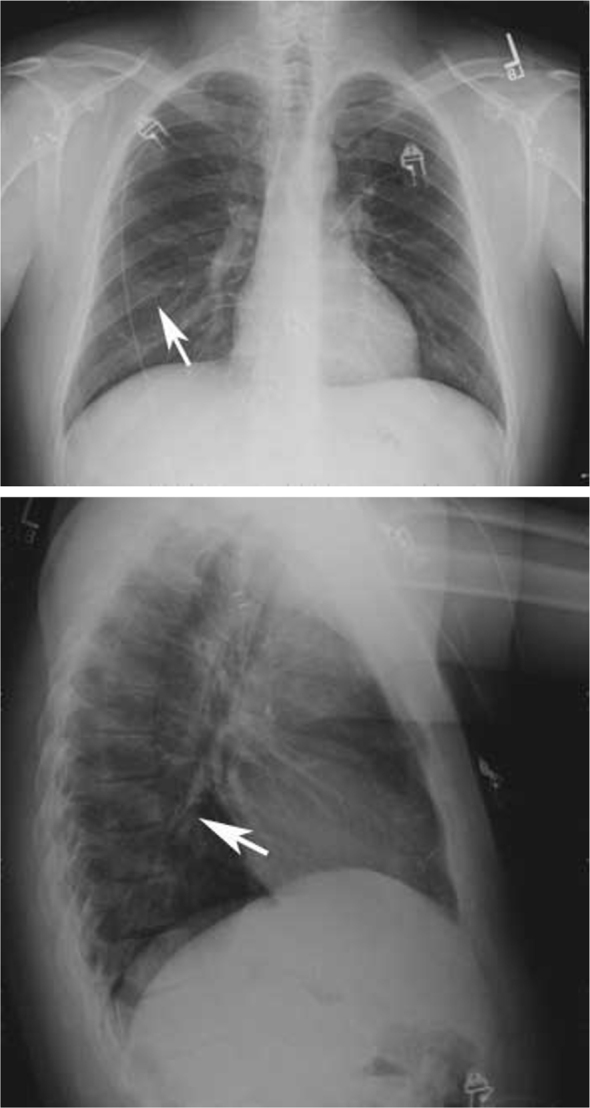
28-year-old man with needle embolism. Frontal and lateral radiographs of the chest demonstrate a thin linear radiodensity in the right midlung.
Figure 2.
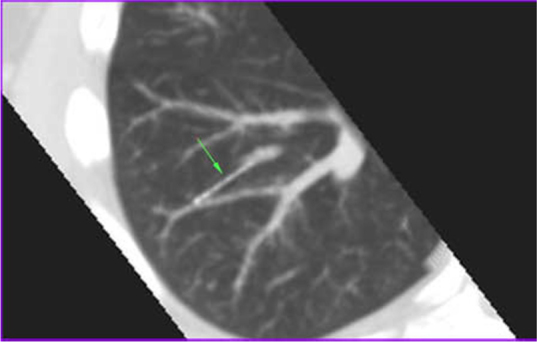
28-year-old man with needle embolism. Multiplanar reconstruction CT of the chest in lung windows (WL/WW -500/1400) shows the thin linear radiodensity extending from a segmental pulmonary artery into peripheral lung parenchyma (arrow).
Case report 2
A 28-year-old man with a history of IVDU presented to our emergency department with pleuritic chest pain, dyspnea, and malaise. He was afebrile, with elevated ESR (48mm/hr), elevated c-reactive protein (140 mg/L), elevated D-dimer (3.05 mcg/mL), and borderline leukocytosis (10,260/uL, 67% neutrophils, no bands). A CT pulmonary angiogram revealed a linear metallic object with surrounding irregular consolidation in the peripheral right middle lobe (Fig. 3). A concurrent chest radiograph confirmed the presence of a needle (Fig. 4).
Figure 3.
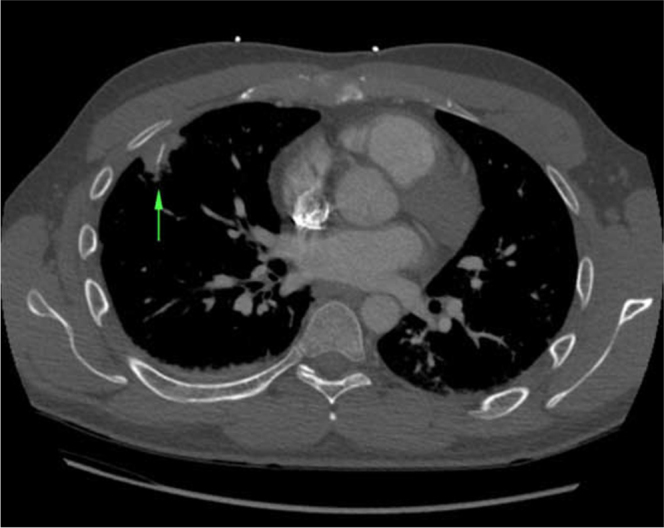
28-year-old man with needle embolism. Axial image from pulmonary embolism protocol CT of the chest in bone windows (WL/WW 300/1500) demonstrates a linear radiodensity within an irregular consolidation in the peripheral right middle lobe (arrow).
Figure 4.

28-year-old man with needle embolism. Frontal radiograph of the chest, A, Full field of view. B. 10X enlargement of right lung region of interest reveals a linear radiodensity in the right mid-lung (arrow) with faint surrounding consolidation.
Upon further questioning, the patient endorsed that several days before he had lost control of a needle while injecting into his right femoral vein. He subsequently visited an urgent care clinic for inflammation at the injection site; a targeted ultrasound did not show any retained fragments.
After initial workup in our emergency department, the patient was admitted to the thoracic surgery service, where he remained stable. Based on his lack of obvious infection and the usual benign course of pulmonary needle embolism, he was treated empirically with trimethoprim-sulfamethoxazole and doxycycline and was scheduled for short-term followup. At one-month follow-up, his pleuritic chest pain had worsened. Although he remained afebrile and had a normal white blood cell count (7,600/uL), the patient elected to undergo wedge resection of his pulmonary phlegmon to alleviate his progressive pain. At surgery, an inflammatory mass adherent to the chest wall was removed, and the presence of an embolized needle within that mass was confirmed. Histologic analysis revealed active inflammation, organizing pneumonia, and chronic active bronchiolitis with prominent eosinophilia. Cultures grew three distinct colony types of methicillin-sensitive staphylococcus aureus, one of which met criteria for vancomycin intermediate staphylococcus aureus (VISA). The patient did well postoperatively. He was discharged on a course of cephalexin (500 mg by mouth four times daily for fourteen days) and scheduled for short-term followup. To date, he has not returned to our institution.
Discussion
In the fourteen cases of central embolism of needle fragments following intravenous drug use (3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15), needles embolized to the right heart in six patients (10, 11, 13, 14, 15, 16) (43%), to the lungs in seven patients (4, 5, 6, 7, 9, 12) (50%) and to both right heart and lung in one patient (8) (7%). In cases of pulmonary embolism, the right lung was affected in seven patients (88%) with only one case of left lung involvement (9). Followup ranged from nil to three years. Needle emboli were found at autopsy in one case and were not contributory to the cause of death (14). Of the seven cases of needle embolization to the heart, three (43%) resulted in complications requiring intervention: two patients developed pericarditis (10, 13), and one developed consequent endocarditis with multiple septic emboli (15). Of the eight cases of pulmonary needle embolism, there were no documented complications or ongoing symptomology.
Of the published cases of centrally embolized foreign bodies, most have been iatrogenic complications of vascular access, intravascular monitoring, or diagnostic device usage (12); needle embolism from intravenous drug use would seem to be comparatively infrequent. However, due to lack of physician awareness of this entity, its inconspicuity on imaging, and its routine absence of symptoms, the true incidence of IVDU-related central needle embolism may be underestimated. A cross-sectional survey of intravenous drug users published in 2002 found that one in five had experienced a needle breaking during drug injection, many of which could not be recovered either by the individual or by professional surgical exploration (3).
In a review of 163 cases of all centrally embolized foreign bodies, Grabenwoeger et al determined that mortality associated with untreated foreign objects was over 30%, with duration and location being the major determinants of complication (17). Specifically, foreign objects in the right heart conferred the highest mortality, with causes of death including cardiac-wall perforation, septic endocarditis, arrhythmias, caval thrombosis causing pulmonary thromboembolism, and cardiac-wall necrosis. Conversely, needle embolism to the lung typically followed a benign course. One case of pulmonary needle embolism remained stable in location and without symptoms through two years of clinical followup. The first case from our institution follows this pattern. Our second case, on the other hand, is the first reported case of pulmonary needle embolism with complications.
Cultures from the resected inflammatory mass in our second case were positive for staphylococcus aureus, skin flora that presumably traveled to the lung as a contaminant on the needle fragment. Aseptic pulmonary granulomas associated with intravenous drug abuse are common and usually attributable to adulterants within the injected substance or injection of pharmaceutical preparations formulated for oral consumption only (18). In a review of over 200 cases of embolization of catheter fragments, Richardson et al identified eight cases of embolization to the lung periphery, none of which required treatment (19). Injection in the context of intravenous drug abuse and particularly in cases of shared needles would presumably carry a higher risk of infection. Although our review identified one case of a needle embolic to the heart that did serve as a nidus for endocarditis (15), none of the previous cases of needle embolism to the lung have required dedicated antibiosis (two patients were treated with antibiotics for infection elsewhere [5, 7]). The presence of prolonged symptoms in our case complicated by an inflammatory mass likely indicated deviance from the usual benign course of pulmonary needle embolism. Our experience suggests that ongoing symptoms attributable to the needle fragment may warrant closer monitoring and possibly intervention.
Footnotes
Published: September 22, 2012
References
- 1.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Drug abuse warning network: Detailed tables: National estimates, Drug-related emergency department visits for 2004–2009. Rockville, MD, December 28, 2010. Available at: http://www.samhsa.gov/
- 2.Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70. doi: 10.1016/S0140-6736(11)61138-0. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Norfolk GA, Gray SF. Intravenous drug users and broken needles–a hidden risk? Addiction. 2003;98(8):1163–1166. doi: 10.1046/j.1360-0443.2003.00462.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Lewis TD, Henry DA. Needle embolus: a unique complication of intravenous drug abuse. Ann Emerg Med. 1985;14(9):906–908. doi: 10.1016/s0196-0644(85)80645-4. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Angelos MG, Sheets CA, Zych PR. Needle emboli to lung following intravenous drug abuse. J Emerg Med. 1986;4(5):391–396. doi: 10.1016/0736-4679(86)90217-9. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Galdun JP, Paris PM, Weiss LD, Heller MB. Central embolization of needle fragments: a complication of intravenous drug abuse. Emerg Med. 1987;5(5):379–382. doi: 10.1016/0735-6757(87)90385-8. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Brunette DD, Plummer DW. Pulmonary embolization of needle fragments resulting from intravenous drug abuse. Am J Emerg Med. 1988;6(2):124–127. doi: 10.1016/0735-6757(88)90048-4. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Horattas MC, Moorman DW. Cardiopulmonary needle embolization: a complication of central venous drug abuse. Am J Emerg Med. 1988;6(1):27–30. doi: 10.1016/0735-6757(88)90200-8. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Hart BL, Newell JD, 2nd, Davis M. Pulmonary needle embolism from intravenous drug abuse. Can Assoc Radiol J. 1989;40(6):326–327. [PubMed] [PubMed] [Google Scholar]
- 10.Gyrtrup HJ, Andreassen KH, Pedersen JH, Mortensen LB. Central embolization of needle fragment following intravenous drug abuse. Br J Addiction. 1989;84(1):103–105. doi: 10.1111/j.1360-0443.1989.tb00557.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Stern MF, Steinbach BG. Hypodermic needle embolism to the heart. N Y State J Med. 1990;90(7):368–371. [PubMed] [PubMed] [Google Scholar]
- 12.Kulaylat MN, Barakat N, Stephan RN, Gutierrez I. J Embolization of illicit needle fragments. Emerg Med. 1993;11(4):403–408. doi: 10.1016/0736-4679(93)90242-y. [PubMed] [DOI] [PubMed] [Google Scholar]
- 13.LeMaire SA, Wall MJ, Jr, Mattox KL. Needle embolus causing cardiac puncture and chronic constrictive pericarditis. Ann Thorac Surg. 1998;65(6):1786–1787. doi: 10.1016/s0003-4975(98)00246-x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Thorne LB, Collins KA. Speedballing with needle embolization: case study and review of the literature. J Forensic Sci. 1998;43(5):1074–1076. [PubMed] [PubMed] [Google Scholar]
- 15.Ngaage DL, Cowen ME. Right ventricular needle embolus in an injecting drug user: the need for early removal. Emerg Med J. 2001;18(6):500–501. doi: 10.1136/emj.18.6.500. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Low GS, Jenkins NP, Prendergast BD. Images in cardiology. Needle embolism in an intravenous drug user. Heart. 2006;92(3):315. doi: 10.1136/hrt.2004.059279. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grabenwoeger F, Bardach G, Dock W, Pinterits F. Percutaneous extraction of centrally embolized foreign bodies: a report of 16 cases. Br J Radiol. 1988;61(731):1014–1018. doi: 10.1259/0007-1285-61-731-1014. [PubMed] [DOI] [PubMed] [Google Scholar]
- 18.Dettmeyer RB, Verhoff MA, Bruckel B, Walter D. Weidespread pulmonary granulomatosis following longtime intravenous drug abuse - a case report. Br J Radiol. 2010;197(1-3):27–30. doi: 10.1016/j.forsciint.2009.12.066. [PubMed] [DOI] [PubMed] [Google Scholar]
- 19.Richardson JD, Grover RL, Trinkle JK. Intravenous catheter emboli. Experiences with twenty cases and collective review. Br J Radiol. 1974;128(6):722–727. doi: 10.1016/0002-9610(74)90057-9. [PubMed] [DOI] [PubMed] [Google Scholar]


