Abstract
We report a rare case of a ruptured distal anterior inferior cerebellar artery aneurysm that was successfully treated by endosaccular embolization, and review the literature on the results of endovascular surgery for this condition.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; AICA, anterior inferior cerebrllar artery
Introduction
Distal anterior inferior cerebellar artery (AICA) aneurysms are extremely rare and account for only 0.025% to 0.1% of all cerebral aneurysms. Morphologically, distal AICA aneurysms tend to be more dissecting or fusiform than saccular. The aneurysm most often occurs in a region unrelated to the bifurcation of the AICA. It is often necessary to trap the parent artery, because of morphological problems with the artery. Therefore, the treatment of AICA is often difficult.
Case report
A 61-year-old woman experienced a sudden onset of headache and vomiting while bicycling and was transferred to a neighboring hospital by ambulance. Because computed tomography (CT) revealed subarachnoid hemorrhage (SAH), she was transported to our hospital. On admission, she was alert. Her neurological status was World Federation of Neurological Societies grade I. CT showed SAH, predominantly in the right ambient cistern (Fig. 1). Three-dimensional CT (3D-CT) angiography could not identify the ruptured aneurysm with motion artifact. Digital subtraction angiography showed a saccular aneurysm in the distal aspect of the meatal loop of the right AICA (Fig. 2). Since craniotomy was judged to be difficult from the region of the aneurysm, we planned endosaccular embolization using coils. The patient and her family were advised about the possibility of parent artery occlusion, and they gave their informed consent to perform endosaccular embolization.
Figure 1.

61-year-old female with ruptured distal anterior inferior cerebellar artery aneurysm. A plain CT scan on admission showing thin subarachnoid hemorrhage, mainly in the right ambient cistern (arrow).
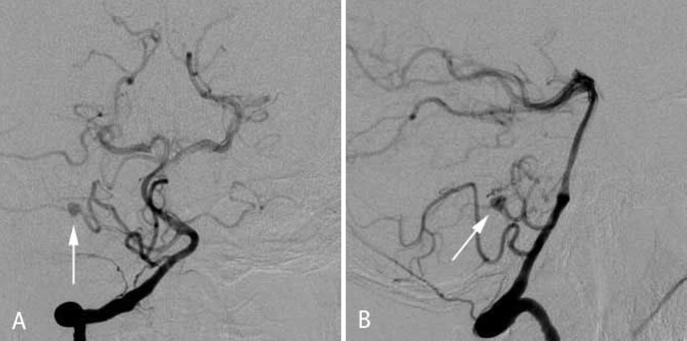
Figure 2.
61-year-old female with ruptured distal anterior inferior cerebellar artery aneurysm. An anterior-posterior view (A) and lateral view (B) of the preoperative digital subtraction angiography of the right vertebral artery showing a saccular aneurysm of the anterior inferior cerebellar artery in the distal aspect of the meatal loop (arrow).
Under general anesthesia, a 5-Fr guiding catheter (Envoy; Johnson & Johnson Company, Miami, FL, USA) was navigated via a transfemoral arterial access over a guidewire into the left vertebral artery (VA). We first tried to approach the aneurysm by using an Excelsior SL-10 (shaping angle of the tip is 45°, 1.7F/ 2.3F, Boston Scientific, Fremont, CA, USA). Because the approach angle to the right AICA through the right VA was smaller than that through the left VA, a microcatheter was inserted into the left VA. The right AICA was tortuous, but it could be used to approach the aneurysm by using an Agility 10 soft-tip guidewire (0.010 inch, Johnson & Johnson Company). The aneurysm was located in the distal aspect of the meatal loop. The collateral circulation of the distal AICA was not determined. Therefore, endosaccular embolization was attempted as the first choice. Although the aneurysm had a relatively wide neck (fundus: 3mm, neck: 2mm, fundus/neck ratio: 1.5), it was successfully caged using a 3D coil (Cerecyte Micrusphere, 3 mm × 5.4 cm; Micrus Corp., San Jose, CA, USA), and a distal branch was preserved. Two filling coils (Microplex hypersoft, 2 mm × 6 cm; Terumo, Japan & Cerecyte Ultipaq, 2 mm × 4 cm; Micrus Corp., San Jose, CA, USA) were packed into the aneurysm sac. Complete obliteration of the distal AICA aneurysm was successfully achieved (Fig. 3).
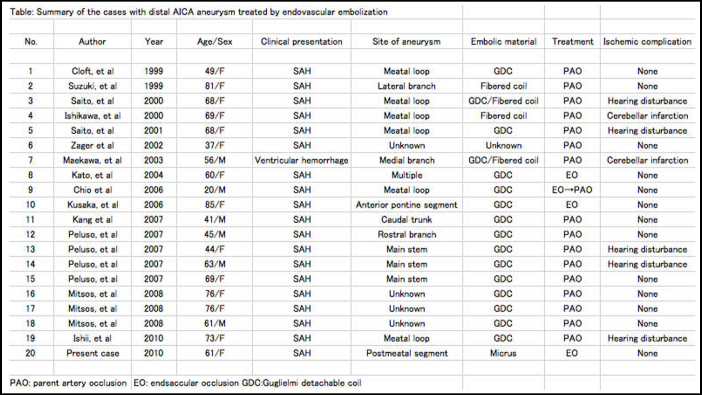
Figure 3.
61-year-old female with ruptured distal anterior inferior cerebellar artery aneurysm. An anterior-posterior view of the postoperative digital subtraction angiography of the right vertebral artery showing complete endosaccular embolization (small arrows). The distal branch is preserved (arrow).
The patient’s postoperative course was uneventful, and she was discharged from our hospital without any neurological deficits. Followup magnetic resonance angiography 14 months after the endovascular surgery revealed complete aneurysmal embolization (Fig. 4).
Figure 4.
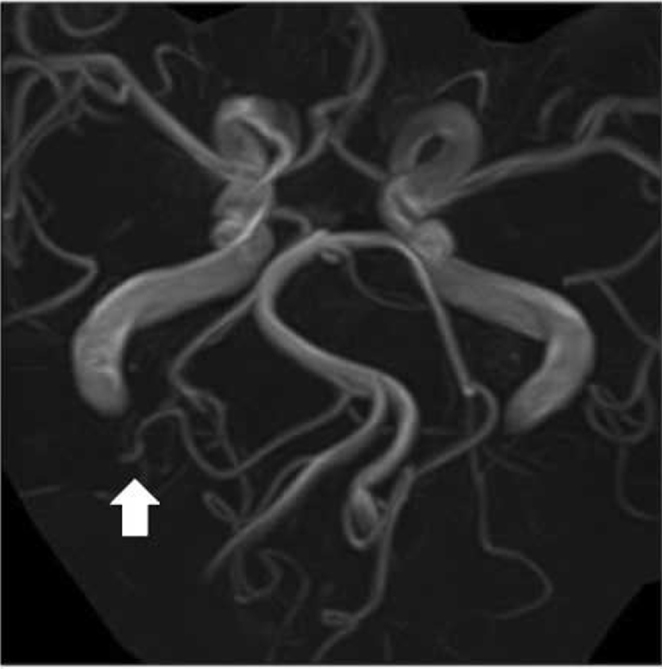
61-year-old female with ruptured distal anterior inferior cerebellar artery aneurysm. Magnetic resonance angiogram taken 14 months after the endovascular surgery demonstrating no aneurysm (arrow).
Discussion
The AICA originates from the basilar artery, usually as a single trunk, and encircles the pons near the abducent, facial, and vestibulocochlear nerves (1). The main trunk from the AICA that is associated with the facial and acoustic nerves is divided into three segments, the premeatal, meatal, and postmeatal, near the porus acusticus internus. Approximately 77% of the auditory arteries originate from the premeatal segment, 21% from the meatal segment, and 2% from the postmeatal segment. Therefore, the proximal occlusion of the meatal segment frequently causes hearing disturbances.
The most common treatment for distal AICA aneurysms is neck clipping or parent vessel occlusion. Aneurysms of the distal AICA most often occur between the facial nerve and the acoustic nerve. Therefore, a direct surgical approach to an AICA aneurysm is difficult, and the complication rate is high.
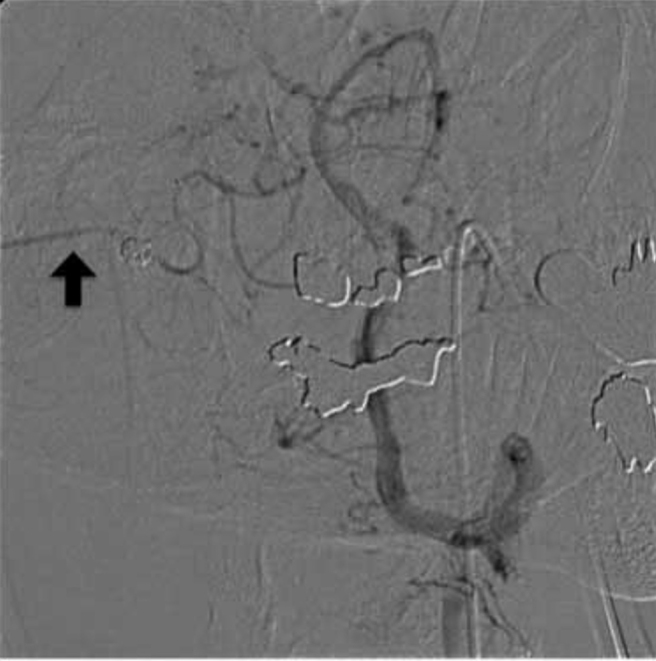
Recently, there have been reports on 20 cases of distal AICA aneurysms treated by endovascular surgery (2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15). The characteristics of the patients and aneurysms are summarized in the table. The study included 6 men and 14 women, with a mean age of 60.1 years (range, 20 to 85 years). The aneurysm location was the premeatal segment in 5, the meatal in 6, the postmeatal in 4, multiple in 1, and unknown in 4. Distal AICA aneurysms tended to be dissecting or fusiform. In that study, occlusion of the parent artery was performed in 85% of the cases. Neurological complications occurred in 7 (35%) of the 20 patients: 5 had hearing disturbances, and 2 had cerebellar infarctions. Aneurysms in the meatal loop were most frequently associated with complications, and had a complication rate of 66%. Therefore, the location of the aneurysm is important when deciding whether to perform endovascular parent artery occlusion. The internal auditory artery, which diverges from the neighborhood of the meatal loop, must be preserved. In addition, because blood flow disorders of the internal auditory artery may develop due to retrograde thrombosis after embolization, it is necessary to consider the regions that will be affected by embolization. Collateral circulation from the PICA is more likely when an aneurysm exists in the distal than in the meatal loop. However, it is difficult to evaluate the collateral circulation in the acute period. Although only a few cases have been reported thus far, endosaccular embolization appears to be a safe and effective treatment.
The parent artery is preserved during an endosaccular embolization, which avoids many complications. However, in many cases the AICA aneurysm is unfit for endosaccular embolization, and in such cases, it is also often difficult to use a microcatheter. Of the 20 patients reported in the previous studies, four underwent an endosaccular embolization. Kato et al. considered that the enlarged AICA, which served as a feeding artery for arteriovenous malformation, facilitated the embolization of the aneurysms (9). Kusaka et al. reported that a rupture was caused during the first endosaccular embolization, which ended in insufficient embolization, and caused a subsequent rerupture (11). This resulted in another endosaccular embolization. Choi et al. reported a case of rerupture following endosaccular embolization for a dissecting aneurysm of the distal AICA with parent artery preservation, which was treated again successfully by parent artery occlusion (10). Therefore, an endosaccular embolization is never an easy technique for distal AICA aneurysms. The choice of the guidewire is also important for leading a microcatheter into the aneurysm. To achieve successful endosaccular embolization, a good understanding of the characteristics of each coil and their use is necessary. Moreover, at present, since parent artery occlusion is selected when endosaccular embolization is difficult, it is important to obtain informed consent about the potential occurrence of complications associated with the procedure.
Technical considerations in endosaccular embolization for AICA distal aneurysm
Approaching from the contralateral side of the VA gives an advantage in advancing a microcatheter to a tortuous artery like a distal AICA, because it makes an obtuse angle. It is essential to navigate a microcatheter with a small caliber and a soft tip preceded by a soft-tip guidewire. First, it should be gently advanced into the distal portion of the AICA beyond the aneurysm. Second, the microcatheter should be pulled back slowly near the aneurysmal neck, which will enable the navigation of the microcatheter into the aneurysmal lumen safely. Third, caging using a 3D coil, followed by filling coils, is effective for a broad-neck aneurysm (similar to this case), in attempts to preserve a parent artery.
Footnotes
Published: May 31, 2012
References
- 1.Martin RG, Grant JL, Peace D. Microsurgical relationships of the anterior inferior cerebellar artery and the facial-vestibulocochlear nerve complex. Neurosurgery. 1980;6:483–550. doi: 10.1227/00006123-198005000-00001. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Cloft HJ, Kallmes DF, Jensen ME. Endovascular treatment of ruptured, peripheral cerebral aneurysms: Parent artery occlusion with short Guglielmi detachachable coils. AJNR Am J Neuroradiol. 1999;20:308–310. [PubMed] [PMC free article] [PubMed] [Google Scholar]
- 3.Suzuki K, Meguro K, Wada M. Embolization of a ruptured aneurysm of the distal anterior inferior cerebellar artery: case report and review of the literature. Surg Neurol. 1999;51:509–512. doi: 10.1016/s0090-3019(97)00462-x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Saito A, Ezura M, Takahashi A. An arterial dissection of the distal anterior inferior cerebellar artery treated by endovascular therapy. No Shinkei Geka. 2000;28:269–274. [PubMed] [PubMed] [Google Scholar]
- 5.Ishikawa E, Yanada K, Meguro K. Treatment of peripheral aneurysms of the posterior circulation. No Shinkei Geka. 2000;28:337–343. [PubMed] [Google Scholar]
- 6.Saito R, Tominaga T, Ezura M. Distal anterior inferior cerebellar artery aneurysma: report of three cases and literature review. No Shinkei Geka. 2001;29:709–714. [PubMed] [PubMed] [Google Scholar]
- 7.Zager EL, Shaver EG, Hurst RW. Distal anterior inferior cerebellar artery aneurysms. Report of four cases. J Neurosurg. 2002;97(3):692–696. doi: 10.3171/jns.2002.97.3.0692. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Maekawa M, Awaya S, Fukuda S. A ruptured choroidal artery aneurysm of the anterior inferior cerebellar artery obliterated via the endovascular approach: case report. No Shinkei Geka. 2003;31:523–527. [PubMed] [PubMed] [Google Scholar]
- 9.Kato S, Kurokawa T, Yun YS. Endosaccular embolization for multiple distal anterior inferior cerebellar artery aneurysms: a case report. Jpn J Neurosurg. 2004;13:539–544. [Google Scholar]
- 10.Choi CH, Cho WH, Choi BK. Rerupture following endovascular treatment for dissecting aneurysm of distal anterior inferior cerebellar artery with parent artery preservation: retreatment by parent artery occlusion with Guglielmi detachable coils. Acta Neurochir (Wien) 2006;148:363–366. doi: 10.1007/s00701-005-0702-4. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Kusaka N, Maruo T, Nishjiguchi M. Embolization for aneurismal dilatation associated with ruptured dissecting anterior inferior cerebellar artery aneurysm with preservation of the parent artery: case report. No Shinkei Geka. 2006;34:729–734. [PubMed] [PubMed] [Google Scholar]
- 12.Kang HS, Roh HG, Han MH. Successful endovascular occlusion of a ruptured distal anterior inferior cerebellar artery aneurysm of the caudal trunk: case report. Interv Neuroradiol. 2007;13(3):271–276. doi: 10.1177/159101990701300306. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peluso JP, van Rooij WJ, Sluzewski M. Distal aneurysms of cerebellar arteries: incidence, clinical presentation, and outcome of endvascular parent vessel occlusion. AJNR Am J Neuroradiol. 2007;28:1573–1578. doi: 10.3174/ajnr.A0607. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mitsos AP, Corkill RA, Lalloo S. Idiopathic aneurysms of distal cerebellar arteries: endovascular treatment after rupture. Neuroradiology. 2008;50:161–170. doi: 10.1007/s00234-007-0315-0. [PubMed] [DOI] [PubMed] [Google Scholar]
- 15.Ishii D, Takechi A, Shinagawa K. Endovascular treatment for ruptured distal anterior inferior cerebellar artery aneurysm-case report. Neurol Med Chir. 2010;50(5):396–399. doi: 10.2176/nmc.50.396. [PubMed] [DOI] [PubMed] [Google Scholar]