Supplemental Digital Content is available in the text
Abstract
The incidence of primary Crohn colitis is uncommon and surgical treatment has remained controversial, although most patients with Crohn colitis eventually require surgical intervention. This study aims to compare the operative outcomes of patients who underwent segmental versus either total colectomy or total proctocolectomy for Crohn colitis and to assess potential risk factors associated with clinical and surgical recurrence-free survivals.
This is a retrospective study of 116 patients who underwent primary surgery for Crohn colitis between August 1997 and July 2011. Patients were classified based on the type of surgery: segmental colectomy (SC group; n = 71) or either total colectomy or total proctocolectomy (TC group; n = 45).
There were no significant differences in postoperative complications or the nutritional state between the SC and TC groups. Patients in TC group had a significantly higher clinical recurrence-free survival (CRFS). Among the 54 patients with multisegmental Crohn colitis, the TC group had a significantly increased CRFS and surgical recurrence-free survival (SRFS), compared with patients in the SC group (5-year CRFS: 82.0% ± 5.8% vs 22.2% ± 13.9%, P = 0.001; 5-year SRFS: 88.1% ± 5.0% vs 44.4% ± 16.6%, P = 0.001). By multivariate analysis of patients with multisegments involved, SC was a risk factor for SRFS and CRFS (hazard ratio [HR] = 4.637, 95% confidence interval [CI] = 1.387–15.509, P = 0.013 and HR = 32.407, 95% CI = 2.873–365.583, P = 0.005).
TC patients have significantly increased CRFS and TC in patients with multisegment involvement may affect improved SRFS and CRFS. Among patients with multisegmental Crohn colitis, SC is an independent risk factor for CRFS and SRFS.
INTRODUCTION
Although Crohn disease (CD) can involve any part of the alimentary tract, the terminal ileum, with or without involvement of the proximal right colon, appears to be the most common initial site of involvement.1,2 In comparisons of terminal ileal involvement of CD, the incidence of primary Crohn colitis is uncommon and varies from 7% to 44%, depending upon the referral pattern and treatment center.2–4 In ∼25% of patients with Crohn colitis, the rectum and/or the distal sigmoid colon are mostly free of disease.5
Most patients (>70%) with Crohn colitis eventually require surgical intervention.6 The decision on which surgery to perform depends upon the extent and site of disease, the presence of perianal disease, the patient's age and lifestyle, and the willingness of a patient to accept a stoma.3 Total proctocolectomy (TPC) removes all colonic and rectal disease and avoids the use of a diseased anus. TPC has yielded the best long-term results for Crohn colitis based on a recurrence rate of 20% to 26%.7–9 Segmental colectomy can often restore young patients to good health without the risk of impaired sexual function and can delay or avoid the need for a permanent stoma. Some studies that have been published since 2000 reported that surgical recurrence rates after SC ranged from 23% to 67%,10–13 and a recent study also showed that stoma-free survival was similar between patients who underwent segmental and subtotal colectomy (76.8% vs 84.2%, P = 0.62).14
We aimed in the present study to investigate the clinicopathological characteristics and postoperative results of different surgical interventions used to treat Crohn colitis. We also compared recurrence rates according to the surgical interventions and assessed potential risk factors associated with surgical recurrence-free survivals (SRFS) and clinical recurrence-free survivals (CRFS).
METHODS
Patient Enrollment and Exclusion Criteria
Patients who underwent colonic resection for CD at Asan Medical Center (Seoul, Korea) between August 1997 and July 2011 were enrolled in this retrospective study. A total of 229 patients underwent colonic resection for pathologically confirmed CD during the study period. Exclusion criteria for this current study included a history of previous bowel surgery, such as small or large bowel resection or strictureplasty; a concurrent or previous history of other malignancies; emergency surgery; indeterminate colitis; and the absence of a precisely defined location. Patients undergoing segmental resection of the colon for pathologically confirmed ileocecal valve- or terminal ileum-involved CD were also excluded. A total of 116 patients were included in our present analyses. The following variables were retrospectively collected from the medical records of these patients: demographics, preoperative disease characteristics, disease phenotype (Montreal classification),15 operative indications, any history of perianal disease (eg, abscess or fistula), the presence of extraintestinal manifestations, a history of smoking, comorbidity, the operative approach (open vs laparoscopy), operative findings (stricture, fistula, or abscess), postoperative morbidity, the rate of stoma formation, the reoperation rate, follow-up duration, postoperative complications, and pre- and postoperative nutritional parameters (eg, levels of hemoglobin and albumin, or body weight).
The study protocol was approved by the institutional review board of Asan Medical Center (registration no: 2015–0050), in accordance with the Declaration of Helsinki.
Patient Classification
The 116 enrolled patients were classified by the type of surgery into the following 2 groups: patients who had undergone a single segmental colectomy (SC) or multiple SC (SC group, n = 71) and patients who had received a total, or total proctocolectomy (TC group, n = 45). The SC group included patients who underwent right-sided colectomy (RC, n = 52), anterior resection (AR, n = 2), Hartmann operation (n = 2), RC/AR or segmental resection of the sigmoid colon (n = 11), RC/Hartmann operation (n = 3), and RC/low anterior resection (n = 1). The procedures in TC group included total colectomy with anastomosis (n = 23), total colectomy, or TPC with end-ileostomy (n = 22).
Assessment and Follow-Up of Crohn Colitis
CD distribution was assessed based on pathological and intraoperative findings, imaging findings using a small bowel series (SBS), computed tomography (CT) enterography, magnetic resonance imaging (MRI), and colon-fiberscopy (CFS). Perianal disease included stricture, fistula, or an abscess in the perianal area, anal canal, or perirectal space at any time during the course of CD. Surgical recurrence was defined as a repeated operation on any section of the bowel for pathologically confirmed CD. Repeated operations for pathologically confirmed anastomotic disease, including cases in which the small bowel was diseased at the anastomosis or the stoma site, were also defined as surgical recurrences. Clinical recurrence was defined as a definite change in the imaging study (SBS, CT, or MRI) or the CFS following the onset of symptoms in a patient (eg, any type of fistula with an abscess on imaging or a stricture or an ulcer that was difficult to pass by CFS).
Recovery of the Nutritional State
After ascertaining recovery of the nutritional state, the pre- and post-operative levels of hemoglobin and albumin, and the body weight were collected from patient medical records. Maximal levels of preoperative hemoglobin and albumin, as well as body weight (nutritional parameters) at any preoperative period were compared with the maximal postoperative values. Recovery of the nutritional parameter levels was defined as when the maximal level of a postoperative nutritional parameter reached the maximal level of a preoperative nutritional parameter.
Medical Treatment of Crohn's Disease
Our medical treatment policy for treating CD was based on a step-up approach, and more potent therapies were added if and when patients became unresponsive to first-line or less toxic agents, as mentioned in previous report from our institution.16 Oral aminosalicylates, systemic corticosteroid therapy, an immunomodulator, such as methotrexate or azathioprine/6-mercaptopurine, and antitumor necrosis factor (TNF) agents were administered to the patients according to the disease activity. The use of anti-TNF agents in this study was less frequent than in Western studies because of the strict Korean government health insurance reimbursement policy during our study period.16 During the study period, an infliximab as an anti-TNF agent was only used for the enrolled patients.
Statistical Analysis
Data for patient groups were compared using the χ2 test for discrete variables and the unpaired Student t test or Mann-Whitney U test for continuous variables. SRFS and CRFS curves were plotted using the Kaplan-Meier method and compared using the log-rank test. Multivariate analyses for survival, among the variables that were significantly different in the log-rank test, were performed using Cox proportional hazards model with a 95% confidence interval (CI) to assess the risk factors associated with SFRS and CRFS. Statistical significance was defined as P < 0.05; all analyses were performed using SPSS software version 21 (SPSS Inc, Chicago, IL).
RESULTS
Clinicopathologic Characteristics of Patients Undergoing Segmental or Total Colectomy
The SC group contained more women than the TC group (71.8% vs 48.9%, P = 0.02). Patients in the TC group had a longer duration between the diagnosis and the first operation than patients in the SC group (80 vs 41 months, P = 0.001). Compared with the SC group, more patients in the TC group had a history of perianal disease (P = 0.02), and left-sided, rectum, and multiple involvement of the colon (P = 0.001, respectively). The median age at diagnosis of the study cohort was 21 years (interquartile range [IQR] 18–27 years), the median age at the first operation was 26 years (IQR 22–31 years), and the both of age parameter was not significantly different between the SC and TC group (Table 1). The following preoperative parameters were also similar in both group: duration of follow-up, the presence of extraintestinal manifestations, a history of smoking, disease behavior at the time of operation, preoperative state of medical treatment, and American Society Anesthesiologists (ASA) scores (Table 1).
TABLE 1.
Clinical Characteristics of the Study Patients Undergoing Segmental or Total Colectomy for Crohn Colitis

For the operative procedure, more patients in the SC group underwent laparoscopic surgery (12.7% vs 0%, P = 0.01), whereas more patients in the TC group underwent fistula repair or resection (56.3% vs 77.8%, P = 0.02). Regarding other operative details and outcomes, there was no significant difference between 2 groups for the rates of hand-sewn anastomosis, intraoperative abscess drainage, lysis of adhesion, hospital stay, postoperative complications, or the recovery rates of all nutritional parameters except for hemoglobin between the 2 groups (Table 2). Notably, postoperative levels of hemoglobin recovered in more patients in the TC group (86.7% vs 66.2%, P = 0.02). Additionally, more patients in the TC group were administered anti-TNF agent after the first surgery than patients in the SC group (48.9% vs 23.9%, P = 0.008; Table 2). The rates of permanent stoma formation are presented in Table 2, and reoperation details after the second or third surgery are shown in Figure 1.
TABLE 2.
Operative Details and Outcomes of Patients Undergoing Colectomy for Crohn Colitis
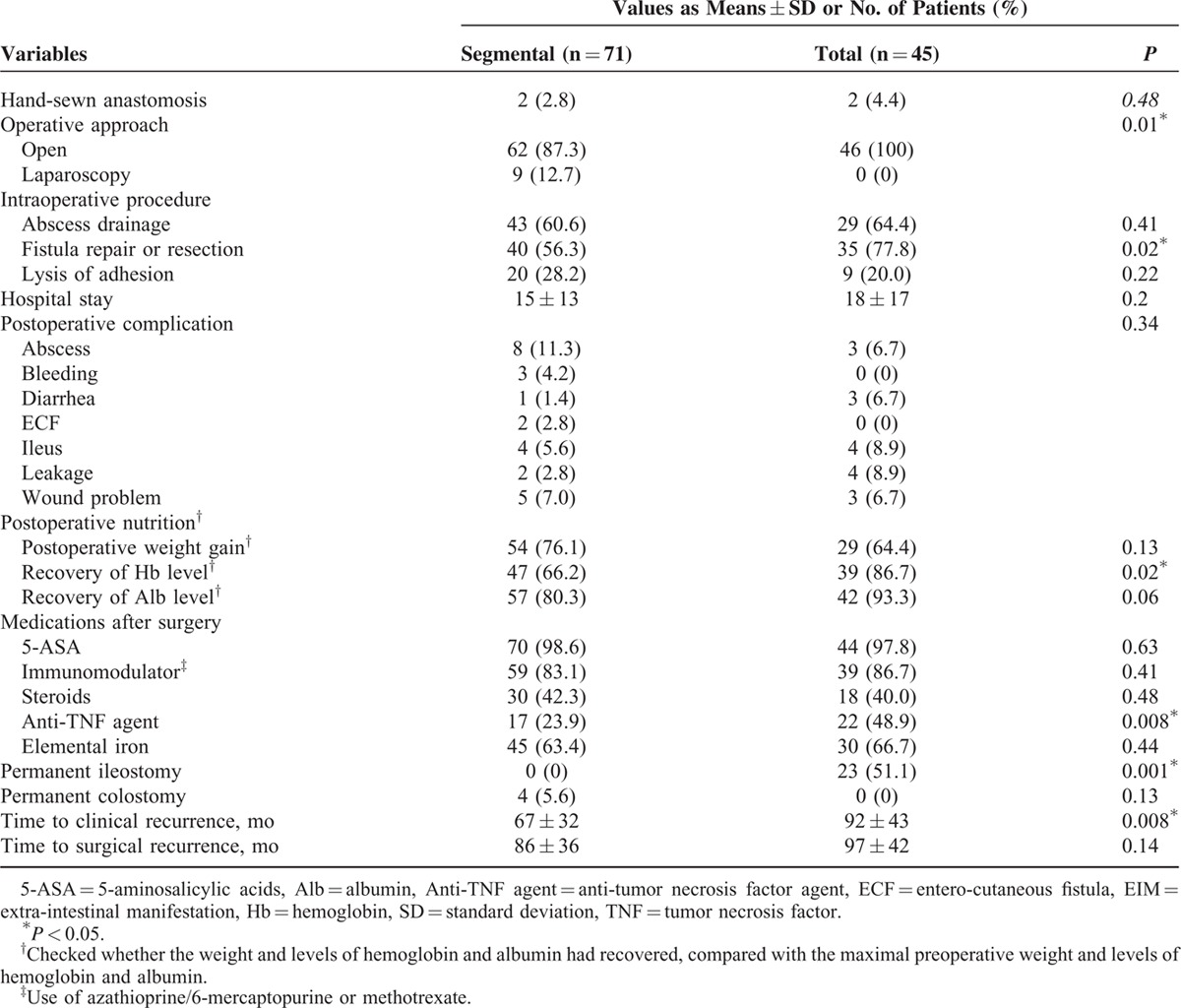
FIGURE 1.

Flow diagram for the study patients undergoing reoperation and permanent stoma formation after an initial resection for Crohn colitis. Inv. = involvement, Pt. = patients or patient. ∗Subtotal, total, or total proctocolectomy with or without end-ileostomy. †Permanent ileostomy formation with or without either total colectomy or total proctocolectomy.
Survival and Recurrence Period
The mean duration of the period between the first and second surgery was not significantly different between the groups, whereas the mean duration time to clinical recurrence was significantly different (SC group, 67 ± 32 months; TC group, 92 ± 42 months; P = 0.008; Table 2). Among the 54 patients who had ≥2 involved colonic segments (multisegments), the mean duration time to surgical and clinical recurrence was significantly shorter in the SC group compared with the TC group (surgical recurrence, 60 ± 33 vs 91 ± 42 months, P = 0.02; clinical recurrence, 40 ± 21 vs 83 ± 42 months, P = 0.002).
Among 116 patients with Crohn colitis, 45 patients in the TC group exhibited a significantly higher CRFS compared with 71 patients in the SC group (5-year CRFS: 82.0% ± 5.8% vs 66.8% ± 5.7%, P = 0.001). By contrast, the SRFS was similar between the 2 groups (Figure 2). Among the 54 patients with multisegments involvement, the TC group showed a significantly higher 5-year CRFS and 5-year SRFS compared with the SC group (5-year CRFS: 82.0% ± 5.8% vs 22.2% ± 13.9%, P = 0.001; 5-year SRFS: 88.1% ± 5.0% vs 44.4% ± 16.6%, P = 0.001; Figure 2). When we divided the SC group into patients who underwent single-segmental resection (SSR) or multi-segmental resection (MSR), the survival outcomes were significantly different between SSR and MSR and between MSR and TC (SSR vs MSR vs TC; 5-year SRFS: 73.6% ± 16.6% vs 57.5% ± 14.6% vs 88.1% ± 5.0%, P = 0.001 and 5-year CRFS: 73.3% ± 5.9% vs 38.5% ± 13.5% vs 82.0% ± 5.8%, P = 0.001; Figure 2).
FIGURE 2.

Surgical and clinical recurrence-free survival in the study patients who underwent colonic resection as an initial resection for Crohn colitis. (A) Surgical recurrence-free survival (SRFS) in 116 patients who underwent segmental colectomy (SC) vs total colectomy (TC); 5-year SRFS, 88.0% ± 4.0% vs 88.1% ± 5.0% (P = 0.17). (B) SRFS in 54 patients with multisegmental Crohn colitis; 5-year SRFS, SC vs TC: 44.4% ± 16.6% vs 88.1% ± 5.0% (P = 0.001). (C) SRFS in 116 patients undergoing single-segmental resection (SSR) vs multisegmental resection (MSR) vs TC; 5-year SRFS, 88.1% ± 5.0% vs 73.6% ± 16.6% vs 57.5% ± 14.6%, (P = 0.001). (D) Clinical recurrence-free survival (CRFS) in 116 patients with Crohn colitis; 5-year CRFS, SC vs TC: 66.8% ± 5.7% vs 82.0% ± 5.8% (P = 0.001) (E) CRFS in 54 patients with multisegmental Crohn colitis; 5-year CRFS, SC vs TC: 22.2% ± 13.9% vs 82.0% ± 5.8% (P = 0.001). (F) CRFS in 116 patients undergoing SSR vs MSR vs TC; 5-year CRFS, 73.3% ± 5.9% vs 38.5 ± 13.5% vs 82.0% ± 5.8% (P = 0.001).
In a univariate analysis of our study subjects, SRFS was associated with a preoperative history of perianal disease, perianal disease after the first operation, the extent of involvement, and the extent of the operation. In subsequent multivariate analysis that included these variables, a history of perianal disease after the first operation, rectal involvement, and SC were found to be risk factors for SRFS (Table 3). The variables that correlated with CRFS by univariate analysis were perianal disease after the first operation, a family history of CD, disease behavior for an operation, multiple involvements, the extent of operation, and recovery of hemoglobin levels. By multivariate analysis, CRFS was associated with penetrating behavior and the operative extent of SC (Table 3).
TABLE 3.
Univariate and Multivariate Analysis of Factors Associated With Surgical and Clinical Recurrence-Free Survival After Colonic Resection to Treat Crohn Colitis

In univariate analysis of 54 patients with multisegment involvement, SRFS was associated with a family history of CD, the extent of operation, and recovery of hemoglobin levels. By multivariate analysis of the 54 patients, SC (hazard ratio [HR] = 4.637, 95% confidence interval [CI] = 1.387–15.509, P = 0.013) and recovery of hemoglobin levels (HR = 0.296, 95% CI = 0.095–0.923, P = 0.036) were risk factors for SRFS. Variables that correlated with CRFS by univariate analysis for the 54 patients with multisegment involvement were perianal disease after the first operation, disease behavior for operation, multiple involvements, the extent of operation, and recovery of hemoglobin levels. Multivariate analysis showed that SC was a risk factor for CRFS (HR = 32.407, 95% CI = 2.873–365.583, P = 0.005) (Supplement Table 1).
No types of medications except anti-TNF agent that were administered after surgery affected CRFS or SFRS. Subgroup analysis of 39 patients who were administered anti-TNF agents after the first operation revealed that there was a significant difference in the CRFS, but not the SRFS between the SC and TC groups (SC vs TC: 5-year SRFS; 87.1% ± 8.6% vs 90.7% ± 6.3%, P = 0.23 and 5-year CRFS; 64.7% ± 11.6% vs 76.4% ± 9.3%, P = 0.024) (Supplement Figure 1). In the subgroup analysis of 77 patients who did not receive anti-TNF agents after the first operation, the survival outcomes were similar to those of anti-TNF-treated patients (SC vs TC: 5-year SRFS; 86.1% ± 4.9% vs 85.6% ± 7.8%, P = 0.29 and 5-year CRFS; 65.6% ± 6.6% vs 82.4% ± 8.0%, P = 0.003). In subgroup analyses of 54 patients with multisegment involvement, the TC group showed a significantly higher 5-year CRFS and 5-year SRFS compared with the SC group, regardless of anti-TNF agents (Supplement Figure 1).
DISCUSSION
Although the 116 Crohn colitis patients treated at our institution during our present study period underwent various types of surgery, we classified these patients into 2 groups depending upon the surgical strategy. We found that the clinical and surgical recurrence rates increased after segmental resection of colon, which was similar to other studies.7,17 Furthermore, we found that the SC group could be defined as an independent risk factor for SRFS and CRFS. Especially, when disease was detected in multisegments, the differences in SRFS and CRFS became severe between the SC and TC groups.
In a comparison of the SC and TC groups, the demographics of these 2 groups of patients differed significantly for sex, duration between the time of diagnosis and the first operation, and segments involved. Although several studies have shown an increased rate of recurrence for females,11,18 we found in our present study that sex had no effect on the recurrence of Crohn colitis (5-year SRFS: female vs male, 82.7% ± 6.0% vs 88.4% ± 3.9%, P = 0.76), which was in accord with the findings of other studies.12,19 Considering the natural history of CD,20 a longer duration between the time of diagnosis and the first operation in the TC group appeared to affect the extent of disease, disease behavior, and the choice of a surgical treatment.
Although the extent of colonic disease affected the choice of surgical treatment, our present findings suggest that TC in patients with multisegment involvement had a lower risk of causing clinical or surgical recurrence and was associated with a prolonged time to clinical and surgical recurrence. Patients in the TC group exhibited a lower crude recurrence rate (10.9%), compared with previous reports that described a 44% crude recurrence risk after resection in Crohn colitis patients.12,21,22 Previous studies have indicated that the recurrence rate for SC varies from 33% to 62%, and that the rate for TC varies from 4% to 79.9%.7,8,11,14,23 In our present study, the 5-year SFRS that we observed after SC and TC was 88.0% and 88.1%, respectively; however, the 5-year SFRS for the patients with multisegment involvement was 44.4% and 88.1% for SC and TC, respectively. For the 5-year CFRS, the patterns of differences were similar to those of the 5-year SFRS between the 2 groups. Based on these findings and our present multivariate analysis, we suggest that SC in patients with multisegmental Crohn colitis could represent an independent risk factor for both surgical and clinical recurrence. Although SC is considered to be a valuable approach for treating single and short segment Crohn colitis,23 multiple SC to treat cases of multisegmental Crohn colitis might not be an optimal choice because of the strong effect on surgical recurrence.
Our present findings also suggested that the surgical recurrence rate of TC with ileorectal anastomosis (IRA) was 10.9% (Figure 1), which contrasted with the increased recurrence rates, that have been previously reported,12,24,25 after IRA. An earlier study reported a rate of recurrence of only 8% after IRA,26 and a meta-analysis by Polle et al11 showed there was no significant difference in the rate of recurrence between patients treated by SC versus TC with IRA. Those previous findings, along with the present results, suggest that TC with IRA could represent the surgical treatment of choice for multisegmental Crohn colitis that spares the rectum and anus.
Previous studies have demonstrated that perianal CD could represent a risk factor for surgical recurrence.12,27 Our present study has also revealed that a history of perianal disease after a first CD-related surgery could be an independent risk factor for surgical recurrence. It was previously suggested that the high risk of recurrence in patients with perianal disease might reflect a subcategory of CD that was associated with a more severe course of disease.12 Other studies that did not use biologics or autologous stem cell transplantation reported that 43% to 46% of patients potentially needed to undergo proctectomy for severe proctitis or perianal disease.28,29 The choice of a “best” operation for colonic CD cannot be solely based on the rate of recurrence, but in high-risk patients with multisegmental Crohn colitis and perianal CD, a permanent stoma might avoid the need for additional surgeries.
In contrast to a previous report,8 we did not find that TC was associated with increased complications compared with SC in our current analyses. Furthermore, patients in TC group exhibited a comparable or better nutritional state, as assessed by the recovery of weight, and levels of hemoglobin and albumin. For the nutritional state, the postoperative levels of hemoglobin significantly recovered in TC group, which might be associated with a lower rate of clinical recurrence in the TC group, compared with the SC group. Anemia is the most common systemic complication and extraintestinal manifestation of CD.30 Similar to a recent study that evaluated the effects of anti-TNF agents on levels of hemoglobin,31 we also found in our present analyses that recovery of hemoglobin levels was a risk factor for SRFS among patients with multisegmental Crohn colitis.
Whether the introduction of immunosuppressive and biological drugs can have a direct effect on the risk for surgery among patients with CD remains the subject of debate.32,33 Our present study could not demonstrate the recurrence-free survival effect of immunosuppressive drug because almost patients (83% and 86%) used the immunosuppressive drug after surgery. Into the subgroup analysis of the patients with multisegment involvement, the administration of anti-TNF agents seemed to mitigate the difference of SRFS between the SC and TC groups (CRFS, P = 0.02 and SRFS, P = 0.043; Supplement Figure 1). However, anti-TNF treatment was not a risk factor of surgical and clinical recurrence-free survival, although further studies will be needed to better characterize this potential association.
Our present study had several notable limitations. As in most single-institution retrospective observational cohort studies, potential biases for both patient referral and selection existed. Additionally, our study design lacked random experimental allocation to the SC or TC group and 2 groups were not comparable for all of the risk factors. Although the formation of permanent stoma is an important consideration for young, socially, and physically active patients, we could not collect data on the quality of life or psychological acceptance of permanent stoma because of the retrospective design of our study.
In conclusions, we found that patients who undergo TC to treat Crohn colitis exhibit a significantly reduced CRFS. We identified SC as an independent risk factor for both SRFS and CRFS. Our data also support the conclusion that total colectomy might be helpful for patients with multisegments involvement, resulting in improved SRFS and CRFS. Recovery of hemoglobin levels after surgery might represent an indicator of surgical recurrence among patients with multisegmental Crohn colitis.
Supplementary Material
Footnotes
Abbreviations: AR = anterior resection, ASA = American Society of Anesthesiologists, CD = Crohn disease, CFS = colon-fiberscopy, CI = confidence interval, CRFS = clinical recurrence-free survival, CT = computed tomography, HR = hazard ratio, IRA = ileorectal anastomosis, MRI = magnetic resonance imaging, MSR = multi-segmental resection, RC = right-sided colectomy, SBS = small bowel series, SC = segmental colectomy, SRFS = surgical recurrence-free survival, SSR = single-segmental resection, TC = total colectomy, TNF = tumor necrosis factor, TPC = total proctocolectomy.
The authors report no conflicts of interest.
Supplemental digital content is available for this article.
REFERENCES
- 1.Farmer RG, Hawk WA, Turnbull RB. Clinical patterns in Crohn's disease: a statistical study of 615 cases. Gastroenterology 1975; 68:627–635. [PubMed] [Google Scholar]
- 2.Farmer RG, Whelan G, Fazio VW. Long-term follow-up of patients with Crohn's disease. Relationship between the clinical pattern and prognosis. Gastroenterology 1985; 88:1818. [DOI] [PubMed] [Google Scholar]
- 3.Tjandra JJ, Fazio VW. Surgery for Crohn's colitis. Int Surg 1991; 77:9–14. [PubMed] [Google Scholar]
- 4.Ritchie JK. The results of surgery for large bowel Crohn's disease. Ann R Coll Surg Engl 1990; 72:155. [PMC free article] [PubMed] [Google Scholar]
- 5.Block GE. Surgical management of Crohn's colitis. N Engl J Med 1980; 302:1068–1070. [DOI] [PubMed] [Google Scholar]
- 6.Goligher JC. Surgical treatment of Crohn's disease affecting mainly or entirely the large bowel. World J Surg 1988; 12:186–190. [DOI] [PubMed] [Google Scholar]
- 7.Longo WE, Ballantyne GH, Cahow CE. Treatment of Crohn's colitis: segmental or total colectomy? Arch Surg 1988; 123:588–590. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto T, Allan RN, Keighley MRB. Audit of single-stage proctocolectomy for Crohn's disease. Dis Colon Rectum 2000; 43:249–256. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto T. Proctocolectomy is associated with a higher complication rate but carries a lower recurrence rate than total colectomy and ileorectal anastomosis in Crohn colitis. Scand J Gastroenterol 1999; 34:1212–1215. [DOI] [PubMed] [Google Scholar]
- 10.Martel P, Betton PO, Gallot D, et al. Crohn's colitis: experience with segmental resections; results in a series of 84 patients. J Am Coll Surg 2002; 194:448–453. [DOI] [PubMed] [Google Scholar]
- 11.Polle SW, Slors JFM, Weverling GJ, et al. Recurrence after segmental resection for colonic Crohn's disease. Br J Surg 2005; 92:1143–1149. [DOI] [PubMed] [Google Scholar]
- 12.Bernell O, Lapidus A, Hellers G. Recurrence after colectomy in Crohn's colitis. Dis Colon Rectum 2001; 44:647–654. [DOI] [PubMed] [Google Scholar]
- 13.Andersson P, Olaison G, Bodemar G, et al. Surgery for Crohn colitis over a twenty-eight-year period: fewer stomas and the replacement of total colectomy by segmental resection. Scand J Gastroenterol 2002; 37:68–73. [DOI] [PubMed] [Google Scholar]
- 14.Kiran RP, Nisar PJ, Church JM, et al. The role of primary surgical procedure in maintaining intestinal continuity for patients with Crohn's colitis. Ann Surg 2011; 253:1130–1135. [DOI] [PubMed] [Google Scholar]
- 15.Satsangi J, Silverberg MS, Vermeire S, et al. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 2006; 55:749–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park SH, Yang S-K, Park S-K, et al. Long-term prognosis of Crohn's disease and its temporal change between 1981 and 2012: a hospital-based cohort study from Korea. Inflamm Bowel Dis 2014; 20:488–494. [DOI] [PubMed] [Google Scholar]
- 17.Allan A, Andrews H, Hilton CJ, et al. Segmental colonic resection is an appropriate operation for short skip lesions due to Crohn's disease in the colon. World J Surg 1989; 13:611–614. [DOI] [PubMed] [Google Scholar]
- 18.Lennard-Jones JE, Stalder GA. Prognosis after resection of chronic regional ileitis. Gut 1967; 8:332–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chardavoyne C, Flint GW, Pollack S, et al. Factors affecting recurrence following resection for Crohn's disease. Dis Colon Rectum 1986; 29:495–502. [DOI] [PubMed] [Google Scholar]
- 20.Freeman HJ. Natural history and long-term clinical course of Crohn's disease. World J Gastroenterol 2014; 20:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andrews HA, Lewis P, Allan RN. Prognosis after surgery for colonic Crohn's disease. Br J Surg 1989; 76:1184–1190. [DOI] [PubMed] [Google Scholar]
- 22.Raab Y, Bergström R, Ejerblad S, et al. Factors influencing recurrence in Crohn's disease. Dis Colon Rectum 1996; 39:918–925. [DOI] [PubMed] [Google Scholar]
- 23.Fichera A, McCormack R, Rubin MA, et al. Long-term outcome of surgically treated Crohn's colitis: a prospective study. Dis Colon Rectum 2005; 48:963–969. [DOI] [PubMed] [Google Scholar]
- 24.Longo WE, Oakley JR, Lavery IC, et al. Outcome of ileorectal anastomosis for Crohn's colitis. Dis Colon Rectum 1992; 35:1066–1071. [DOI] [PubMed] [Google Scholar]
- 25.Ambrose NS, Keighley MR, Alexander-Williams J, et al. Clinical impact of colectomy and ileorectal anastomosis in the management of Crohn's disease. Gut 1984; 25:223–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khubchandani IT, Sandfort MR, Rosen L, et al. Current status of ileorectal anastomosis for inflammatory bowel disease. Dis Colon Rectum 1989; 32:400–403. [DOI] [PubMed] [Google Scholar]
- 27.Andersson P, Olaison G, Hallböök O, et al. Segmental resection or subtotal colectomy in Crohn's colitis? Dis Colon Rectum 2002; 45:47–53. [DOI] [PubMed] [Google Scholar]
- 28.Lock MR, Fazio VW, Farmer RG, et al. Proximal recurrence and the fate of the rectum following excisional surgery for Crohn's disease of the large bowel. Ann Surg 1981; 194:754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stern HS, Goldberg SM, Rothenberger DA, et al. Segmental versus total colectomy for large bowel Crohn's disease. World J Surg 1984; 8:118–121. [DOI] [PubMed] [Google Scholar]
- 30.Oustamanolakis P, Koutroubakis IE, Kouroumalis EA. Diagnosing anemia in inflammatory bowel disease: beyond the established markers. J Crohns Colitis 2011; 5:381–391. [DOI] [PubMed] [Google Scholar]
- 31.Koutroubakis IE, Ramos-Rivers C, Regueiro M, et al. The influence of anti-tumor necrosis factor agents on hemoglobin levels of patients with inflammatory bowel disease. Inflamm Bowel Dis 2015; 21:1587–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nguyen GC, Nugent Z, Shaw S, et al. Outcomes of patients with Crohn's disease improved from 1988 to 2008 and were associated with increased specialist care. Gastroenterology 2011; 141:90–97. [DOI] [PubMed] [Google Scholar]
- 33.Rungoe C, Langholz E, Andersson M, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979-2011. Gut 2014; 63:1607–1616. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


