Abstract
The deleterious effects of radiotherapy, including hypovascularity and hypocellularity, have made distraction of irradiated bones challenging. Animal studies, however, have demonstrated adjunctive measures such as the administration of deferoxamine to significantly improve bone regeneration across irradiated distraction gaps. In this report, we demonstrate, for the first time, enhanced bone formation following deferoxamine application in a patient following distraction of a previously irradiated maxilla. CT imaging of the pterygomaxillary buttress on the side of administration revealed significantly increased bone area and density relative to the contralateral buttress. This is the first presentation of clinical deferoxamine use to promote bone formation following irradiated bone distraction and highlights the promise for this adjunctive measure to make outcomes after distraction of irradiated bone more reliable.
Keywords: Distraction osteogenesis, radiotherapy, deferoxamine, malocclusion
Introduction
Distraction osteogenesis (DO) is routinely performed on the craniofacial skeleton with favorable clinical outcomes (1-5). However, adequate perfusion is considered a prerequisite for successful bone regeneration (6-8), thus clinical reports of DO of the irradiated craniofacial skeleton are rare (9-12). Outcomes have been variable, stimulating clinicians and researchers to explore adjunctive measures to augment bone formation (10, 12-15). A particularly promising approach has been the administration of deferoxamine during the activation/distraction period. An augmentation of vascular density and restoration of metrics of bony union have been reported with the use of deferoxamine in animal models (16, 17). Here we present the first clinical use of deferoxamine in a patient who underwent DO of the previously irradiated maxilla.
Case Report
The patient was a 16-year old male who had a past medical history significant for bilateral retinoblastoma diagnosed at age 3 for which he was treated with chemotherapy, enucleation of the left eye, and radiotherapy. A total of 44 Gy external beam radiation was delivered in 2.0 Gy fractionated doses to the posterior orbit through horizontal opposed lateral fields. He subsequently developed radiation-induced maxillary hypoplasia (Figure 1), resulting in a 12 mm negative overjet requiring a LeFort I distraction.
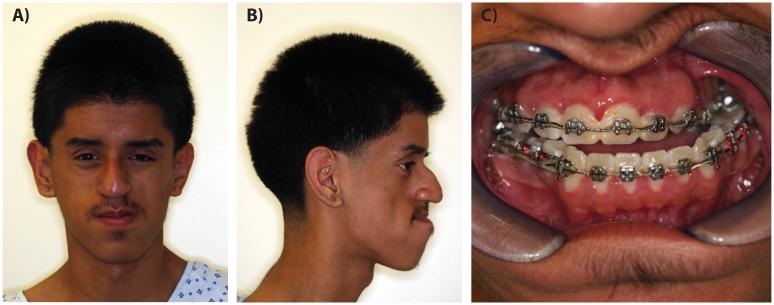
Figure 1.
Preoperative photographs. A) Frontal, B) Lateral and C) Intraoral views displaying severe radiation-induced midface hypoplasia. Note class III malocclusion with 12 mm negative overjet.
Intraoperatively, a LeFort I osteotomy was made and 30 mm telescoping maxillary distractors (KLS Martin, Tuttlingen, Germany) were placed on each side. In order to administer deferoxamine, TLS catheters were laid along the osteotomy sites bilaterally (Figure 2). The catheters were brought through soft tissue, exiting the skin within the nasolabial fold, and secured with 5-0 nylon.
Figure 2.
Intraoperative photograph demonstrating placement of catheters for deferoxamine administration.
Bilateral symmetric distraction was started on postoperative day 1 at a rate of 1 mm/day. Extrapolating from experimental data (16), 0.5 mg of deferoxamine per side was administered every other day. Unfortunately, the right catheter became dislodged prior to the first administration. Thus, deferoxamine was administered to the left side only. Distraction of 16 mm was achieved with correction of the class III malocclusion (Figure 3), and no adverse reactions to deferoxamine, such as pain and swelling at injection site, were reported by the patient.
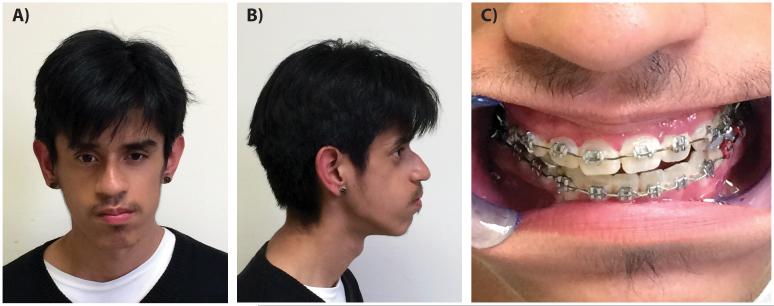
Figure 3.
Postoperative photographs after maxillary distraction. A) Frontal, B) Lateral, and C) Intra-oral views displaying advancement of maxilla and correction of class III malocclusion.
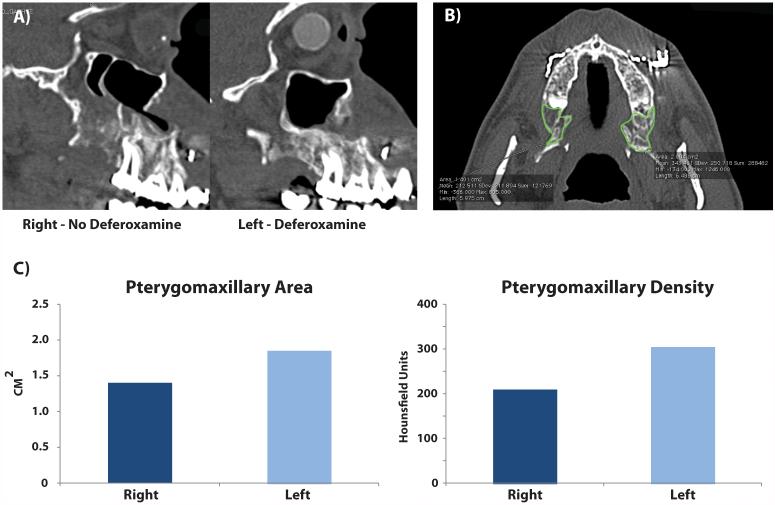
CT imaging obtained at three months demonstrated bony consolidation bilaterally. Bone at the pterygomaxillary osteotomy site, defined by the area posterior to the last molar and anterior to the pterygoid plates across 10 sections on each side, was evaluated, as this region is known to be the main site of bone formation and structural support in distraction of the midface. (18, 19) Two dimensional area and density from Hounsfield units, given consistent thresholding, were calculated from the CT scan. Interestingly, both bone area and density on the deferoxamine-treated (left) side were increased relative to the untreated side after three months (Figure 4). And while they represent secondary sites of support in maxillary distraction, increased bone formation was also noted at both the zygomaticomaxillary buttress and pyriform rim (Figure 5). On removal of the distractors, the maxilla was noted to be stable, with bone found across the distraction gap bilaterally.
Figure 4.
CT imaging following three months of consolidation. A) Sagittal sections through maxilla showing advancement. B) Axial section through pterygomaxillary buttress with region of interest highlighted inside green lines. C) Quantification of CT images demonstrated increased pterygomaxillary buttress area and density on left side.
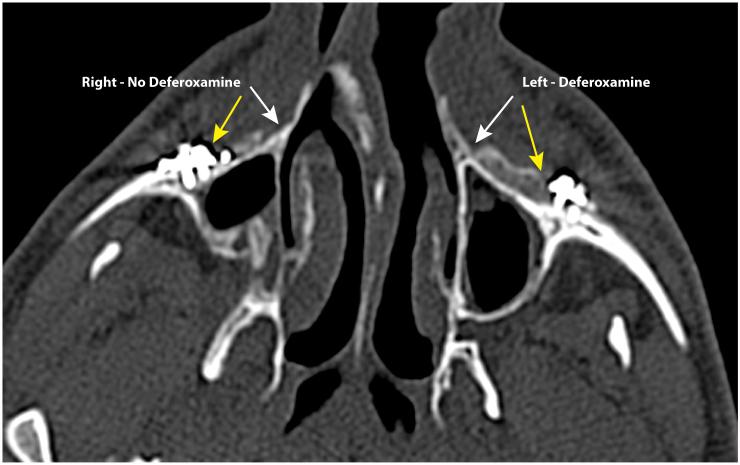
Figure 5.
Axial CT section through region of distraction. Yellow arrows point to region of zygomaticomaxillary buttress and white arrows point to region of pyriform rim. Note increased bone formation at this site on left side treated with deferoxamine.
Discussion
Distraction osteogenesis of the irradiated craniofacial skeleton is rarely reported but has been successful in some cases (9, 20). In particular, Nolte et al. presented successful DO in two adult patients with midface hypoplasia following radiation therapy during childhood (12). These favorable outcomes are contrasted by unfavorable results in two patients presented by Holmes et al., who noted that “DO may not be successful in the irradiated tissue” (10). This sentiment was echoed by Raghoebar and colleagues who stated that “DO in an irradiated mandible is not a treatment modality with a predictable outcome” (11). In light of these reports, clinicians have focused on hyperbaric oxygen (HBO) therapy as an adjunctive measure, though with variable success (10-12, 21).
It seems intuitive to improve vascularity at the osteotomy/distraction site, considering that adequate local blood supply and angiogenesis are prerequisites to ensure successful bone regeneration during DO (22, 23). Importantly, emerging data derived from animal models have suggested a beneficial role for deferoxamine to enhance local vascularity, thus, mitigating the deleterious effects of radiation (16, 24, 25). While use of deferoxamine in this manner is off-label, it is already clinical employed at much higher amounts and with minimal side-effects as an FDA-approved iron chelator for acute iron poisoning and chronic iron overload.
While it was unfortunate that the right catheter became dislodged in our patient, this provided a unique opportunity for the patient to serve as his own control. Though bilateral ossification was noted, the left ptyergomaxillary buttress exposed to deferoxamine during activation/distraction had increased bone area and density compared to the contralateral side. Importantly, the effects of transcutaneous catheter placement on bone formation at the distraction site cannot be completely ruled out. However, overall successful distraction was achieved, albeit with an anterior open bite secondary to premature posterior contact. The patient will still require a finishing osteotomy and rotation of the mandible to properly align his dental midlines.
Our results are limited, however, and reflect findings in only one patient. Furthermore, distraction of the irradiated maxilla may not be as compromised as the mandible, as evidenced by bone formation on the contralateral irradiated maxilla in our patient and by other case reports in the literature.(26) Finally, though in close proximity in a 3 year old, radiotherapy for treatment of this patient's retinoblastomas were not directed at the pterygomaxillary buttresses and instead were directed at the orbits. This still resulted in severe maxillary hypoplasia and our observations do parallel experimental data regarding potential beneficial effects of deferoxamine in the context of DO and radiation.(17, 27, 28) Numerous questions remain unanswered, such as ideal dosing, timing of deferoxamine, etc. Nonetheless, we hope that our experience promotes further clinical use and critical assessment of outcomes of deferoxamine in the context of DO and irradiated craniofacial bone.
Summary
We present the first report, to our knowledge, of clinical deferoxamine use to enhance bone formation with DO of irradiated craniofacial bone. Future prospective studies will need to determine whether this adjunctive measure results in improved outcomes after DO of the irradiated craniofacial skeleton.
Acknowledgement of Support
D.C.W. received support from NIH grant K08 DE024269, S.R.B. received support from NIH grant R01 CA125187
Disclosure of Funding: D.C.W. received support from NIH grant K08 DE024269, S.R.B. received support from NIH grant R01 CA125187
Footnotes
Conflicts of Interest: None declared, all authors have no conflicts of interest to report
References
- 1.Taylor BA, Brace M, Hong P. Upper airway outcomes following midface distraction osteogenesis: a systematic review. J Plast Reconstr Aesthet Surg. 2014;67:891–899. doi: 10.1016/j.bjps.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Saltaji H, Altalibi M, Major MP, et al. Le Fort III distraction osteogenesis versus conventional Le Fort III osteotomy in correction of syndromic midfacial hypoplasia: a systematic review. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2014;72:959–972. doi: 10.1016/j.joms.2013.09.039. [DOI] [PubMed] [Google Scholar]
- 3.Al-Daghreer S, Flores-Mir C, El-Bialy T. Long-term stability after craniofacial distraction osteogenesis. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2008;66:1812–1819. doi: 10.1016/j.joms.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plastic and reconstructive surgery. 1992;89:1–8. [PubMed] [Google Scholar]
- 5.Flores RL. Neonatal mandibular distraction osteogenesis. Seminars in plastic surgery. 2014;28:199–206. doi: 10.1055/s-0034-1390173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donneys A, Tchanque-Fossuo CN, Farberg AS, Deshpande SS, Buchman SR. Bone regeneration in distraction osteogenesis demonstrates significantly increased vascularity in comparison to fracture repair in the mandible. The Journal of craniofacial surgery. 2012;23:328–332. doi: 10.1097/SCS.0b013e318241db26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deshpande SS, Donneys A, Kang SY, et al. Vascular analysis as a proxy for mechanostransduction response in an isogenic, irradiated murine model of mandibular distraction osteogenesis. Microvascular research. 2014;95:143–148. doi: 10.1016/j.mvr.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fang TD, Salim A, Xia W, et al. Angiogenesis is required for successful bone induction during distraction osteogenesis. J Bone Miner Res. 2005;20:1114–1124. doi: 10.1359/JBMR.050301. [DOI] [PubMed] [Google Scholar]
- 9.Taub PJ, Bradley JP, Kawamoto HK. Closure of an oronasal fistula in an irradiated palate by tissue and bone distraction osteogenesis. J Craniofac Surg. 2001;12:495–499. doi: 10.1097/00001665-200109000-00018. discussion 500. [DOI] [PubMed] [Google Scholar]
- 10.Holmes SB, Lloyd T, Coghlan KM, Newman L. Distraction osteogenesis of the mandible in the previously irradiated patient. J Oral Maxillofac Surg. 2002;60:305–309. doi: 10.1053/joms.2002.30581. [DOI] [PubMed] [Google Scholar]
- 11.Raghoebar GM, Jansma J, Vissink A, Roodenburg JL. Distraction osteogenesis in the irradiated mandible. A case report. J Craniomaxillofac Surg. 2005;33:246–250. doi: 10.1016/j.jcms.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Nolte JW, Jansma J, Becking AG. Distraction osteogenesis of maxilla and midface in postradiotherapy patients. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2012;70:1145–1151. doi: 10.1016/j.joms.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 13.Hong P, Boyd D, Beyea SD, Bezuhly M. Enhancement of bone consolidation in mandibular distraction osteogenesis: a contemporary review of experimental studies involving adjuvant therapies. J Plast Reconstr Aesthet Surg. 2013;66:883–895. doi: 10.1016/j.bjps.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 14.Page EE, Deshpande SS, Nelson NS, et al. Prophylactic administration of amifostine protects vessel thickness and luminal diameter in the setting of irradiation. Plast Reconstr Surg. 2014;134:1. doi: 10.1016/j.bjps.2014.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page EE, Deshpande SS, Nelson NS, et al. Prophylactic administration of Amifostine protects vessel thickness in the setting of irradiated bone. J Plast Reconstr Aesthet Surg. 2014 doi: 10.1016/j.bjps.2014.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Felice PA, Ahsan S, Donneys A, Deshpande SS, Nelson NS, Buchman SR. Deferoxamine administration delivers translational optimization of distraction osteogenesis in the irradiated mandible. Plastic and reconstructive surgery. 2013;132:542e–548e. doi: 10.1097/PRS.0b013e31829fe548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donneys A, Deshpande SS, Tchanque-Fossuo CN, et al. Deferoxamine expedites consolidation during mandibular distraction osteogenesis. Bone. 2013;55:384–390. doi: 10.1016/j.bone.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kusnoto B, Figueroa AA, Polley JW. Radiographic evaluation of bone formation in the pterygoid region after maxillary distraction with a rigid external distraction (RED) device. J Craniofac Surg. 2001;12:109–117. doi: 10.1097/00001665-200103000-00003. discussion 118. [DOI] [PubMed] [Google Scholar]
- 19.Polley JW, Figueroa AA. Rigid external distraction: its application in cleft maxillary deformities. Plast Reconstr Surg. 1998;102:1360–1372. discussion 1373-1364. [PubMed] [Google Scholar]
- 20.Gonzalez-Garcia R, Rodriguez-Campo FJ, Naval-Gias L, Sastre-Perez J, Diaz-Gonzalez FJ. The effect of radiation in distraction osteogenesis for reconstruction of mandibular segmental defects. Br J Oral Maxillofac Surg. 2007;45:314–316. doi: 10.1016/j.bjoms.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Sawaki Y, Hagino H, Yamamoto H, Ueda M. Trifocal distraction osteogenesis for segmental mandibular defect: a technical innovation. J Craniomaxillofac Surg. 1997;25:310–315. doi: 10.1016/s1010-5182(97)80032-7. [DOI] [PubMed] [Google Scholar]
- 22.Ai-Aql ZS, Alagl AS, Graves DT, Gerstenfeld LC, Einhorn TA. Molecular mechanisms controlling bone formation during fracture healing and distraction osteogenesis. Journal of dental research. 2008;87:107–118. doi: 10.1177/154405910808700215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aronson J. Temporal and spatial increases in blood flow during distraction osteogenesis. Clin Orthop Relat Res. 1994:124–131. [PubMed] [Google Scholar]
- 24.Donneys A, Farberg AS, Tchanque-Fossuo CN, Deshpande SS, Buchman SR. Deferoxamine enhances the vascular response of bone regeneration in mandibular distraction osteogenesis. Plast Reconstr Surg. 2012;129:850–856. doi: 10.1097/PRS.0b013e31824422f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Farberg AS, Jing XL, Monson LA, et al. Deferoxamine reverses radiation induced hypovascularity during bone regeneration and repair in the murine mandible. Bone. 2012;50:1184–1187. doi: 10.1016/j.bone.2012.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grover R, Murray D, Fialkov JA. Distraction osteogenesis of radiation-induced orbitozygomatic hypoplasia. The Journal of craniofacial surgery. 2008;19:678–683. doi: 10.1097/SCS.0b013e31805344a4. [DOI] [PubMed] [Google Scholar]
- 27.Farberg AS, Sarhaddi D, Donneys A, Deshpande SS, Buchman SR. Deferoxamine enhances bone regeneration in mandibular distraction osteogenesis. Plastic and reconstructive surgery. 2014;133:666–671. doi: 10.1097/01.prs.0000438050.36881.a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Donneys A, Ahsan S, Perosky JE, et al. Deferoxamine restores callus size, mineralization, and mechanical strength in fracture healing after radiotherapy. Plastic and reconstructive surgery. 2013;131:711e–719e. doi: 10.1097/PRS.0b013e3182865c57. [DOI] [PMC free article] [PubMed] [Google Scholar]