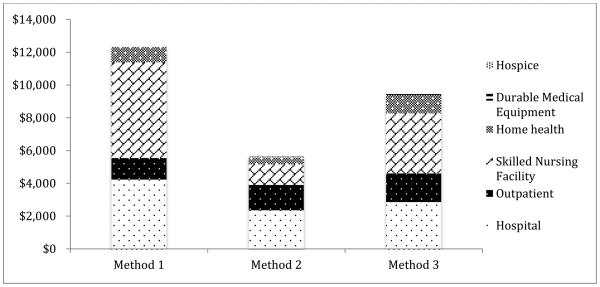
Figure 1. Adjusted Annual Medicare Expenditures by Service Category for Older Adults Experiencing a Fall-related Injury (FRI) Using Three Methods to Identify FRIs in Medicare Claims Data, 2007-9.
Note: The expenditure outcome is expenditures in the post period minus expenditures in the pre period (“expenditures change score”) and the predictor of interest is an indicator for whether the observation is from the FRI vs. non-FRI cohort. The estimated marginal effect of this indicator, or the beta coefficient, therefore reflects the differential change in expenditures experienced over time between individuals who did and did not have an FRI. Because this methodology controls for measurable and unmeasurable confounders that do not vary within an individual over time, the difference in change scores can be interpreted as the incremental expenditures associated with an FRI during the year after falling. The models control for baseline sociodemographic, health, and geographic characteristics. Method 1 involves the use of e-codes (880, 881, 882, 884, 885, or 888) only. Method 2 uses the same e-codes plus primary inpatient diagnostic codes indicating fractures, dislocations, sprains, strains, head injuries, and contusions (ICD-9 diagnostic codes 800-848, 850-854, and 920-924). Method 3 involves FRIs identified using the adapted UCLA/RAND algorithm15 in which FRIs are identified using inpatient (hospital and SNF) ICD-9 primary diagnoses and the same e-codes plus outpatient diagnoses and procedural codes. Models were estimated using OLS regression with robust standard errors. The respective analytic sample sizes for models estimated separated using FRI identification Methods 1-3 were 5,518, 5,479, and 5,497. The models do not include individuals who died during the post-index period. Separate models were estimated for each payment source. The percentage of total estimated expenditures across the three methods for hospital, outpatient, skilled nursing facility, home health, durable medical equipment, and hospice were: 35%, 11%, 48%, 8%, 0%, 0% (Method 1); 42%, 27%, 22%, 8%, 1%, 0% (Method 2); and 31%, 18%, 39%, 12%, 1%, 0% (Method 3).