Highlights
-
•
Difficult diagnosis due to the paucity of symptoms and atypical radiological findings.
-
•
Primary site of infection was not detected.
-
•
Splenectomy is the best therapeutic choice in case of splenic abscess.
Keywords: Splenectomy, Splenic abscess, Splenic hematic collection
Abstract
Introduction
Isolated splenic abscess is a rare clinical condition and remains a diagnostic dilemma. Clinical presentation is non-specific and the diagnosis is often delayed. Ultrasonography and CT scan are the gold standard. The treatment is still controversial: antibiotic therapy, percutaneous drainage (PCD) or splenectomy.
Case presentation
We present the clinical case of a patient, admitted to our Department because of abdominal pain, without fever. The preoperative radiological assesment showed three intrasplenic liquid collections, whose differential diagnosis was made between hematic collection and abscess. The treatment was splenectomy. The samples of collected liquid were positive for Escherichia Coli.
Conclusion
In case of splenic abscess, splenectomy is the best therapeutic choice. The other therapeutical options like antibiotic therapy and PCD, can be used only in particular cases, but without the same efficacy.
1. Introduction
Splenic abscess is an uncommon disease, whose incidence in autoptical studies varies from 0.14% to 0.7% [1], [2]. The recognized risk factors are neoplasm, immunodeficiency, trauma, metastatic infection, splenic infarction and diabetes [3]. The improvement of diagnostic imaging modalities such as computerized tomography (CT) and ultrasonography (US) allows a faster and more accurate diagnosis [4], [5], [6]. The treatment of splenic abscess is still controversial and is based on antibiotic therapy, percutaneous drainage (PCD) or splenectomy, which still remains the best option [7], [8], [9], [10].
2. Case presentation
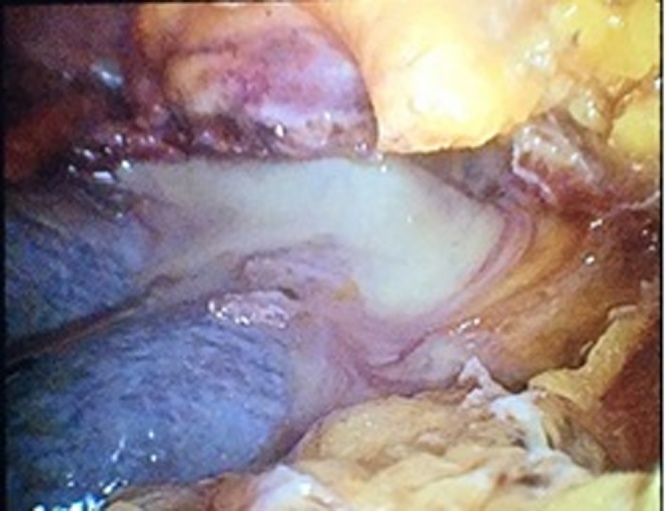
In June 2015, a 80-year-old man was admitted to our Department because of abdominal pain mainly localized in left hypocondrium, without fever. The patient’s medical history was significant for left hemicolectomy for adenocarcinoma of the sigmoid colon followed by adjuvant chemotherapy and appendectomy in 2003, one episode of ocular myasthenia gravis in 2013 treated with steroids, ischemic ictus in 2014 in therapy with Clopidogrel and monoclonal gammopathy of undetermined significance (MGUS) since 2014. No abdominal or thoracic trauma or features suggestive of local/systemic infections, cardiomiopathy or valvulopathy were referred. Abdominal examination showed mild pain in the left upper quadrant and no splenomegaly. Laboratory exams showed leucocytosis (21.000/mm3 with high neutrophilia), other routine hematological and biochemical investigations were normal, and both serological viral markers and the hemocoltures were all negative. A US of the spleen showed three hypoechoic lesions, the greater measuring 6 cm in diameter, with mixed echostructure, mostly liquid. A CT scan showed moderate splenomegaly with hypodense lesions attributable to the presence of liquid content and reactive thickening of perisplenic tissue, associated to subcapsular lesions at the superior pole of the spleen (Fig. 1). An antibiotic therapy with amoxicillin + clavulanic acid 875 mg + 125 mg × 2/die was started. Nonetheless after seven days the pain localized in the left upper quadrant of the abdomen persisted. A CT scan was therefore repeated showing no image changes compared to the previous exam. Neither US nor CT scan were helpful in the differential diagnosis between hematic collections or abscess. Intrasplenic hematic collections represented the most likely diagnosis and we therefore chose the surgical approach because of the risk of delayed rupture and consequent hemoperitoneum. We started with a laparoscopic approach and after sectioning the spleno-colic ligament we found the spleen completely wrapped by omental adhesions and multiple cystic lesions protruding from the splenic capsule, both in the hilar region and on the convex aspect of the organ. Because of the chronic inflammation of the cyst walls and their consequent adhesions with the diaphragm, the isolation of the spleno-diaphragmatic ligament was difficult. During the dissection performed with a radiofrequency device (LigaSure Vessel Sealing System, Valleylab, Boulder, Colo), an opening of a splenic cyst with important leak of pus occurred (Fig. 2). The liquid was collected for bacterial culture. Due to the strong adhesions and to the proximity between the abscess’ wall and the splenic pedicle, a conversion of the procedure to a laparotomic subcostal incision was decided. Splenectomy was completed by means of a sharp dissection of the perisplenic tissue and by separate splenic artery and vein ligation, according to the technique described in literature [11]. Intravenous antibiotic therapy (piperacillin + tazobactam 4 g + 0.5 g × 3/die) was continued for seven days. The postoperative course was uneventful and the patient was discharged at 8 p.o. day. The samples of collected liquid were positive for Escherichia Coli. Histological and immunohistochemical analysis revealed spleen with diffuse areas of parenchymal necrosis associated with signs of aspecific inflammation. The inflammatory reaction was extended to the adipose tissue with perivisceral steatonecrosis. No immunomorphologic evidence of neoplasia or morphologic histochemical evidence of alcohol-acid resistant bacilli and hyphae and/or fungal spores was shown.
Fig. 1.
CT SCAN: splenic hypodense lesions with liquid content associated to a reactive thickening of perisplenic tissue.
Fig. 2.
INTRAOPERATIVE VIEW: ruptured cyst with pus.
3. Discussion
Isolated splenic abscess is an unusual disease. The incidence is between 0.2% and 0.7% [12].The diagnosis of splenic abscess can be difficult because the clinical features are nonspecific; fortunately modern imaging has improved the diagnostic process, even if in our case both the CT scan and the US did not give us the right diagnosis. To confirm the diagnosis of splenic abscess 3 typical features were lacking at CT scan: the “rim-enhancement” of the outside-facing portion of the abscess wall, inhomogeneous density of the content and gas formation [13]. Fever is the most common symptom seen followed by abdominal pain and tender mass to the palpation [14]. However, in our case, the patient only had abdominal pain. Since the most likely hypothesis was that of a blood collection we decided to monitor the patient and repeat a CT scan after 7 days to detect any evolution of the lesions. However, we put the patient under antibiotic coverage. Predisposing conditions to the development of a splenic abscess are trauma, metastatic hematogenous infection, immunodeficiency, and contiguous site of infection. The pathogens most frequently recognised as responsible of splenic abscesses have been aerobic microbes, in particular Streptococci and Escherichia coli [15], [16], followed by M. Tuberculosis, Salmonella typhi and Bartonella hensalae [17], [18], [19]. Some studies also report that gram-negative K. pneumonia was one of the most frequently involved microbacterial pathogens [20]. If the lesions were the result of an intrasplenic hemorrhage, the causes could be either traumatic or spontaneous. The patient denied any kind of major traumatic event in his life even in the past; he was in therapy with anticoagulants (Clopidogrel) because of the previous ischemic ictus; the combination of the two factors could cause the bleeding phenomena. If the collections were infected as suggested by the results of the bacterial colture and the spreading was hematogenous, we still do not know the origin. In literature, the positivity to E. Coli is related to urinary infection [21] or to complication of colonic cancer [22]. In our case no contiguous nor distant sites of infection were detected. The fact that the diagnosis was not established preoperatively posed an issue in respect to the most suitable treatment. Since the treatment of a splenic abscess and of a hematoma at risk of rupture or infection is in both cases splenectomy, we were reassured about the validity of the surgical treatment option. There is no gold standard treatment for splenic abscess. Traditionally, treatment includes high dosage antibiotic with or without splenectomy [13]. Percutaneous aspiration or PCD may be a less invasive option in patients who are at high risk for surgery, or a temporary solution used as a bridge to surgery, avoiding the risk of a fulminant and potentially life-threatening infection [7]. PCD is a successful approach when the abscess collection is unilocular or bilocular, with a complete and thick wall and no internal septations, and when the content is liquid enough to be drained. If there are more than two collections, surgical treatment is to be preferred [22].
4. Conclusions
In conclusion, the best therapeutic approach for splenic abscess is still controversial. However, based on our case experience and current literature, percutaneous aspiration of splenic abscess can be used not only in particular cases, in all other cases splenectomy represents the best therapeutic choice.
Conflicts of interest
There is no conflict of interest to declare.
Funding
None.
Ethical approval
The paper is not a research study.
Consent
Written informed consent was obtained from the patient for publication of this case report.
Author contribution
Marco Casaccia, ideated the study and drafted the article.
Simona Macina, acquisition of data, drafting the article.
Rosario Fornaro, revising it critically for important intellectual content.
Marco Frascio, substantial contributions to conception and design.
Tommaso Testa, revising it critically for important intellectual content.
Cesare Stabilini, drafting the article revising it critically for important intellectual content.
Ezio Gianetta, final approval of the version to be submitted.
All authors approved the final draft.
Guarantor
Dr. Simona Macina.
References
- 1.Chun C.H., Raff M.J., Contreras L., Varghese R., Waterman N., Daffner R. Splenic abscess. Medicine (Baltimore) 1980;59:50–65. doi: 10.1097/00005792-198001000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Nelken N., Ignatius J., Skinner M., Christensen N. Changing clinical spectrum of splenic abscess: a multicenter study and review of the literature. Am. J. Surg. 1987;154:27–34. doi: 10.1016/0002-9610(87)90285-6. [DOI] [PubMed] [Google Scholar]
- 3.Ng K.K., Lee T.Y., Wan Y.L., Tan C.F., Lui K.W., Cheung Y.C. Splenic abscess: diagnosis and management. Hepatogastroenterology. 2002;49:567–571. [PubMed] [Google Scholar]
- 4.Chang K.C., Chuah S.K., Changchien C.S., Tsai T.L., Lu S.N., Chiu Y.C. Clinical characteristics and prognostic factors of splenic abscess: a review of 67 cases in a single medical center of Taiwan. World J. Gastroenterol. 2006;12:460–464. doi: 10.3748/wjg.v12.i3.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smyrniotis V., Kehagias D., Voros D., Fotopoulos A., Lambrou A., Kostopanagiotou G. Splenic abscess. An old disease with new interest. Dig. Surg. 2000;17:354–357. doi: 10.1159/000018878. [DOI] [PubMed] [Google Scholar]
- 6.Anyfantakis D., Kastanakis M., Katsougris N., Papadomichelakis A., Petrakis G., Bobolakis E. Acute torsion of a wandering spleen in a post-partum female: a case report. Int. J. Surg. Case Rep. 2013;4(8):675–677. doi: 10.1016/j.ijscr.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chou Y.H., Hsu C.C., Tiu C.M., Chang T. Splenic abscess: sonographic diagnosis and percutaneous drainage or aspiration. Gastrointest. Radiol. 1992;17:262–266. doi: 10.1007/BF01888563. [DOI] [PubMed] [Google Scholar]
- 8.Ralls P.W., Quinn M.F., Colletti P., Lapin S.A., Halls J. Sonography of pyogenic splenic abscess. AJR Am. J. Roentgenol. 1982;138:523–525. doi: 10.2214/ajr.138.3.523. [DOI] [PubMed] [Google Scholar]
- 9.Carbonell A.M., Kercher K.W., Matthews B.D., Joels C.S., Sing R.F., Heniford B.T. Laparoscopic splenectomy for splenic abscess. Surg. Laparosc. Endosc. Percutan. Tech. 2004;14:289–291. doi: 10.1097/00129689-200410000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Tung C.C., Chen F.C., Lo C.J. Splenic abscess: an easily overlooked disease? Am. Surg. 2006;72:322–325. [PubMed] [Google Scholar]
- 11.Casaccia M., Torelli P., Cavaliere D., Santori G., Panaro F., Valente U. Minimal-access splenectomy: a viable alternative to laparoscopic splenectomy in massive splenomegaly. JSLS. 2005;9(October–December (4)):411–414. [PMC free article] [PubMed] [Google Scholar]
- 12.Alabousi A., Patlas M.N., Scaglione M., Romano L., Soto J.A. Cross-sectional imaging of nontraumatic emergencies of the spleen. Curr. Probl. Diagn. Radiol. 2014;43(September–October (5)):254–267. doi: 10.1067/j.cpradiol.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Paris S., Weiss S.M., Ayers W.H., Jr., Clarke L.E. Splenic abscess. Am. Surg. 1994;60:358–361. [PubMed] [Google Scholar]
- 14.Sarr M.G., Zuidema G.D. Splenic abscess—presentation, diagnosis, and treatment. Surgery. 1982;92:480–485. [PubMed] [Google Scholar]
- 15.Ooi L.L., Leong S.S. Splenic abscesses from 1987 to 1995. Am. J. Surg. 1997;174:87–93. doi: 10.1016/s0002-9610(97)00030-5. [DOI] [PubMed] [Google Scholar]
- 16.Llenas-García J., Fernández-Ruiz M., Caurcel L., Enguita-Valls A., Vila-Santos J., Guerra-Vales J.M. Splenic abscess: a review of 22 cases in a single institution. Eur. J. Intern. Med. 2009;20:537–539. doi: 10.1016/j.ejim.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 17.Allal R., Kastler B., Gangi A., Bensaid A.H., Bouali O., Cherrak C. Splenic abscesses in typhoid fever: uS and CT studies. J. Comput. Assist. Tomogr. 1993;17:90–93. doi: 10.1097/00004728-199301000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Lee W.S., Choi S.T., Kim K.K. Splenic abscess: a single institution study and review of the literature. Yonsei Med. J. 2011;52(March (2)):288–292. doi: 10.3349/ymj.2011.52.2.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anyfantakis D., Kastanakis M., Papadomichelakis A., Petrakis G., Bobolakis E. Cat-scratch disease presenting as a solitary splenic abscess in an immunocompetent adult: case report and literature review. Infez. Med. 2013;21(June (2)):130–133. [PubMed] [Google Scholar]
- 20.Gayol Mde C., Sopena N., Camps I., Pedro-Botet M.L. Splenic abscess secondary to urinary tract infection caused by Escherichia coli. Med. Clin. (Barc.) 2006;127(October (6)):638–639. doi: 10.1157/13094433. [DOI] [PubMed] [Google Scholar]
- 21.Gervaise A., De Saint Roman C., Sockeel P., Lapierre M., Darbois H., Rousset J. Splenic abscess secondary to a colosplenic fistula as the presenting manifestation of colon cancer. J. Radiol. 2010 Dec;91(12 Pt. 1):1259–1262. doi: 10.1016/s0221-0363(10)70184-0. [DOI] [PubMed] [Google Scholar]
- 22.Conzo G., Docimo G., Palazzo A., Della Pietra C., Stanzione F., Sciascia V. The role of percutaneous US-guided drainage in the treatment of splenic abscess. Case report and review of the literature. Ann. Ital. Chir. 2012;83(September–October (5)):433–436. [PubMed] [Google Scholar]