Abstract
Background: The purpose of this study is to evaluate the role of radiographic and clinical exams in predicting screw penetration into the proximal radioulnar joint and ulnohumeral joint during open reduction and internal fixation of the radial head and proximal ulna. Methods: Olecranon and radial head plates were applied to 15 cadaveric elbows. Screws were assessed for intra-articular joint penetration using both clinical exam and radiographic evaluation. Clinical exam consisted of evaluation for crepitus. Radiographs demonstrating screws positioned near the joint surface were evaluated for penetration by 3 fellowship trained hand surgeons. Elbows were disarticulated and screw prominence was determined and recorded using standardized calipers. The ability of clinical and radiographic exams to correctly predict a breach in the articular surface was determined by calculating sensitivity, specificity, and predictive values. Consideration was given to screw position. Results: The sensitivity of crepitus was 81.1% for screws in the radial head plate and 72.6% for screws in the olecranon plate. The sensitivity of radiographs was 72.4% for the screws in the radial head plate and 55.0% for screws in the olecranon plate. Correct radiographic assessment of penetration varied but position o-2 on the olecranon plate consistently resulted in the lowest sensitivity of 30.3%. Conclusions: The study evaluates sensitivity and specificity of clinical and radiographic means when assessing for articular penetration of screws during olecranon and radial head locking plate fixation. Certain screw locations are more difficult to evaluate than others and may go undetected by standard means of assessment used in a surgical setting.
Keywords: radial head, olecranon, crepitus, ORIF, screw penetration, proximal radioulnar, ulnohumeral
Introduction
Fractures of the radial head/neck and fractures of the olecranon are common injuries with incidences of around 2.8 and 1.15 per 10 000 person-years, respectively.16,18 Open reduction and internal fixation is currently the preferred method for treating certain types of olecranon fractures including those that are comminuted, distal to the midpoint of the trochlear notch, or involve the medial coronoid facet.5,6,11,12,15,26 Similarly, open reduction and internal fixation (ORIF) is a commonly used surgical technique for radial head fractures that are displaced and in 2 or 3 fracture parts.13,14,17,21,24
Despite the increasing popularity of ORIF for these elbow fractures, the technique is not without potential complications. Previous studies have documented the anatomical variance of the proximal radius and ulna and have aimed at establishing guidelines to achieve proper osteosynthesis and avoid proximal radioulnar joint (PRUJ) impingement.10,23,28 Inadvertent intra-articular screw penetration can lead to early joint degeneration, pain, and loss of function.24 Lindenhovius et al evaluated 16 patients who underwent plate fixation for fractures of the radial head. Two patients experienced limited forearm rotation due to screws penetrating the PRUJ and underwent additional procedures to modify screw length.20 Similarly, a recent retrospective review of 18 patients who received ORIF for comminuted olecranon fractures reported that 2 patients required revision surgery for impingement.8
Intraoperative radiographs and evaluation for crepitus are standard surgical practice for determining if screws violate the articular surface. The PRUJ and the ulnohumeral joint (UHJ) can be difficult to assess fluoroscopically and the accuracy of clinical exam to detect intra-articular screw penetration is unknown. Other reports have examined the reliability of these methods in a variety of joints other than the PRUJ and UHJ.1,3,4,29 The purpose of this study is to determine how reliable these methods are in instances when the PRUJ or UHJ may be penetrated during ORIF of the olecranon or radial head.
Materials and Methods
Fifteen cadaveric elbows had both olecranon and radial head/neck plates applied via a midline posterior approach. A 3-hole, Accumed standard curvature plate was affixed to the radial head in the “safe zone”28 using a 2.3-mm screw placed through the available slotted hole (see Figure 1). A second, stabilizing screw was placed in the distal-most hole in the plate (see Figure 1). Using the available targeted locking guide, bicortical drill holes aimed into the PRUJ were made through the 2 screw holes termed position r-1 and position r-2 (see Figure 1). The depth of each hole was measured and recorded using a calibrated depth gauge. This measurement was used as a starting point for determining the minimum screw length that would penetrate the articular surface and produce crepitus. Three fluoroscopic views of the elbow were obtained to evaluate the PRUJ. The views included a direct lateral, hypersupinated oblique, and fully pronated lateral. Next, screw lengths were decreased in 2-mm increments until passive range of motion (PROM) confirmed no crepitus, implying the screw tip had sunk below the articular surface. This screw length was recorded and repeat views were obtained.
Figure 1.
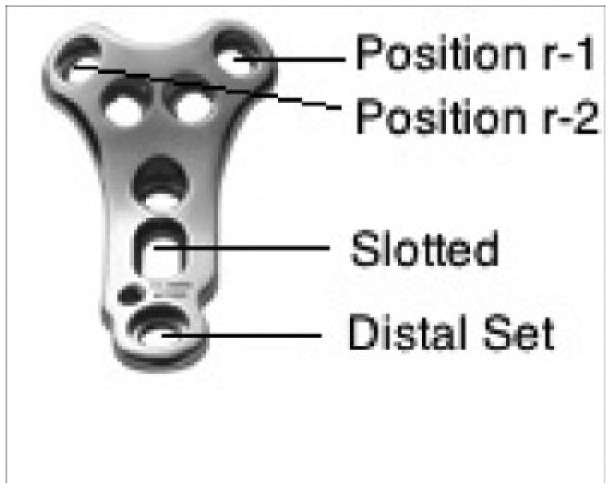
Radial head plate.
A similar process was used using the Acumed Locking Olecranon Plate system. A 3-hole olecranon plate (Acumed Locking Elbow Plating System) was provisionally fixed to the ulnar shaft by a 3.5-mm screw placed through the available slotted hole (see Figure 2). A second, stabilizing 3.5-mm screw was then placed through the distal set hole in the plate. Bicortical drill holes penetrating the UHJ were then made in the proximal 2.7-mm screw cluster at position o-1 and position o-2 (see Figure 2). Not all screw holes were used in this proximal cluster; rather those screws deemed most likely to penetrate the UHJ were selected. A third bicortical drill hole was made at position o-3, and a 3.5-mm screw was inserted (see Figure 2). Position o-3 was chosen because it is the only screw with the potential to penetrate the PRUJ. The steps used to determine minimum screw length required to cause crepitus were repeated. Both the UHJ and PRUJ were manually loaded and taken through a PROM to confirm crepitus. Three fluoroscopic views of the UHJ and PRUJ were obtained. These included a standard anteroposterior (AP) and lateral, as well as the hypersupinated oblique view best positioned to assess intra-articular penetration at the PRUJ. Similarly, screw lengths were decreased in 2-mm increments until crepitus was no longer present with PROM. Repeat fluoroscopic images were taken with the shorter no crepitus producing screw.
Figure 2.
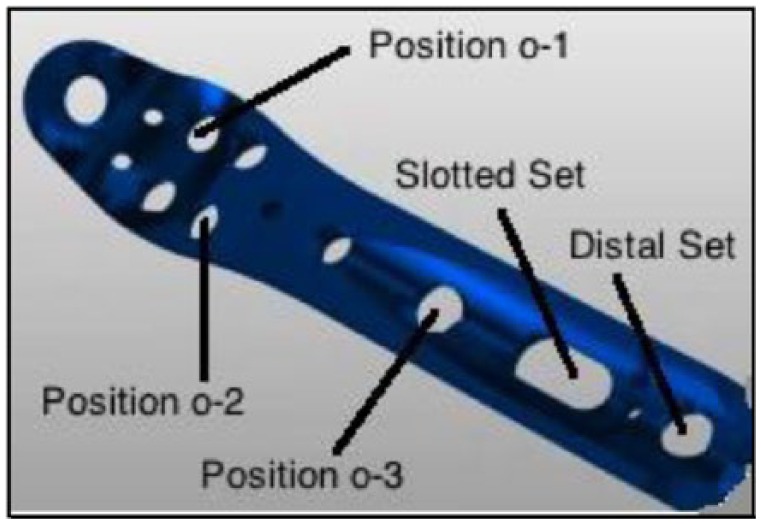
Olecranon plate.
Once all radiographs were obtained and examinations for crepitus were complete, the elbow was disarticulated. The joint surface of the UHJ and PRUJ was evaluated for screw penetration with both screws lengths (those that produced crepitus as well as those that did not (see Figure 3). The length of any intra-articular portion of the screws was measured using a calibrated Vernier digital caliper (no. 101-101; Tresna Guangxi, China). Screws that did not surface through the cartilage enough to ascertain a height measurement (<0.8 mm) were simply noted as visible (vis).
Figure 3.
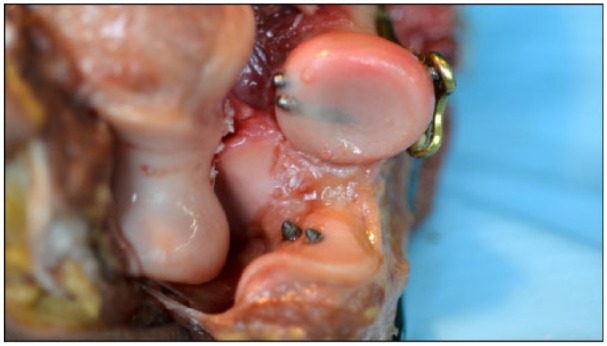
Example of intra-articular trajectory of radial head and olecranon screws.
Three, blinded, fellowship trained orthopedic hand surgeons reviewed the radiographs on 2 separate occasions, 6 weeks apart, and were asked not to discuss the images in the interim. The reviewers were asked to determine the presence or absence of screw penetration after examining radiographs. Each screw position was evaluated independently to determine whether certain screw positions were more problematic.
Sensitivity, specificity, positive predictive values, and negative predictive values were calculated for both diagnostic tests assessed in this study. A chi-square analysis was performed for each reviewer to determine whether the distribution of accuracy differed by screw positions. To minimize the possibility of chance in predicting joint penetration kappa statistics were performed to determine intraobserver and interobserver reliability. Kappa values range from 0.00 to 1.00, with 1.00 indicating perfect agreement and 0.00 demonstrating agreement due solely to chance. The method described by Fleiss was used to calculate interobserver agreement between multiple observers, using the system described by Landis and Koch to interpret numerical values.9,19 Using the aforementioned system, ≤0 indicates poor agreement, 0.00 to 0.20 indicates slight agreement, 0.20 to 0.40 indicates fair agreement, 0.40 to 0.60 indicates moderate agreement, 0.60 to 0.80 indicates substantial agreement, and 0.80 to 1.00 indicates almost perfect agreement.
Results
Clinical Evaluation
Two screw positions were assessed on the radial head plate termed positions r-1 and r-2. The shortest screws observed to cause crepitus had an average intra-articular height of 1.49 mm (range 0.78-2.48 mm) at position r-1, and 1.28 mm (range vis: 1.91 mm) at position r-2. Two of the screws that produced crepitus at position r-2 did not surface out of the radial head enough to ascertain a height measurement thus noted as vis; see Table 1). Of the screws that did not produce crepitus at position r-1, 4 were found to be visible and 1 had an intra-articular height of 0.7 mm. Of the screws that did not produce crepitus at position r-2, 1 was found to be visible and 1 had an intra-articular height of 0.7 mm. In total, 7 (23%) of the radial head screws that did not produce crepitus were observed to penetrate the PRUJ. Of note was the finding of radial head cartilage thinning in 2 of the cadaveric specimens, both of which were observed to have screws at position r-1 that extended into the joint and yet did not produce crepitus (cadaver 3 and cadaver 4). The sensitivity of crepitus as a clinical exam finding was found to be 81.1% for the radial head plate. Complete calculations including sensitivity, specificity, positive predictive values, and negative predictive values are provided in Table 2.
Table 1.
Radial Head Plate Intra-articular Screw Height.
| Specimen no. | Side | Position R-1 |
Position R-2 |
|---|---|---|---|
| Crepitus screw intra-articular height | Crepitus screw intra-articular height | ||
| 1 | L | 1.53 | 0.91 |
| 2 | L | 1.52 | 1.5 |
| 3 | L | 0.88 | 1.73 |
| 4 | R | 2.48 | 1.34 |
| 5 | R | 2.01 | 1 |
| 6 | R | 1.33 | 1.81 |
| 7 | R | 1.55 | visa |
| 8 | R | 0.94 | 1.13 |
| 9 | R | 1.78 | 0.99 |
| 10 | R | 0.88 | visa |
| 11 | R | 1.66 | 1.22 |
| 12 | R | 1.59 | 1.21 |
| 13 | R | 0.78 | 0.5 |
| 14 | R | 2.04 | 1.91 |
| 15 | R | 1.38 | 1.37 |
| Mean | 1.5 | 1.3 | |
| SD | 0.48 | 0.40 |
Screws that penetrated the joint <0.80 mm are marked as vis (visible).
Table 2.
Radial Head Plate Sensitivity, Specificity, Positive Predictive Values, and Negative Predictive Values.
| Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | |
|---|---|---|---|---|
| Crepitus | ||||
| Position r-1 | 75.0 | 100.0 | 100.0 | 66.7 |
| Position r-2 | 88.2 | 100.0 | 100.0 | 86.7 |
| Total | 81.1 | 100.0 | 100.0 | 76.7 |
| Radiographs | ||||
| Position r-1 | 71.7 | 85.0 | 90.5 | 60.0 |
| Position r-2 | 73.2 | 86.1 | 88.8 | 68.1 |
| Total | 72.4 | 85.6 | 89.7 | 64.2 |
Three screw positions were assessed on the olecranon plate termed positions o-1, o-2, and o-3. The screws observed to produce crepitus had an average intra-articular height of 1.67 mm (range vis: 2.68 mm) at position o-1, 2.00 mm (range 0.93-3.09 mm) at position o-2, and 1.86 mm (range vis: 3.48 mm) at position o-3. One screw at position o-1 and 6 screws at position o-3 did not emerge from the ulnar aspect of the UHJ enough to ascertain a height measurement and were noted as visible (see Table 3). Of the screws that did not produce crepitus, 6 were visible at position o-1, 5 were visible at position o-2, and 4 were visible at position o-3. In addition, two screws at position o-2 were found to have an intra-articular height of 0.87 mm and 1.57 mm without producing any crepitus, bringing the total to 7 screws at position o-2 that entered the joint without clinical evidence of doing so. In total, 13 (29%) of the screws on the olecranon plate did not produce crepitus yet were observed to have entered the UHJ and 4 (9%) were found to not produce crepitus but to have entered the PRUJ. The sensitivity of crepitus as a clinical exam finding was found to be 72.6% for the olecranon plate. Complete calculations including sensitivity, specificity, positive predictive values, and negative predictive values are provided in Table 4.
Table 3.
Olecranon Plate Intra-articular Screw Height.
| Specimen no. | Side | Position o-1 |
Position o-2 |
Position o-3 |
|---|---|---|---|---|
| Crepitus screw intra-articular height | Crepitus screw intra-articular height | Crepitus screw intra-articular height | ||
| 1 | L | visa | 2.85 | 2.52 |
| 2 | L | 1.65 | 3.2 | 2.67 |
| 3 | L | 2.21 | 2.2 | visa |
| 4 | R | 1.85 | 1.37 | visa |
| 5 | R | 2.13 | 3.09 | 1.12 |
| 6 | R | 0.75 | 2.15 | 0.75 |
| 7 | R | 1.74 | 1.65 | visa |
| 8 | R | 1.24 | 1.81 | 1.72 |
| 9 | R | 1.7 | 0.93 | visa |
| 10 | R | 2.68 | 2.61 | 2.07 |
| 11 | R | 1.65 | 1.39 | 1.25 |
| 12 | R | 1.2 | 1.89 | visa |
| 13 | R | 2.33 | 1.13 | visa |
| 14 | R | 0.89 | 1.6 | 1.17 |
| 15 | R | 1.32 | 2.22 | 3.48 |
| Mean | 1.7 | 2.0 | 1.9 | |
| SD | 0.55 | 0.73 | 0.89 |
Screws that penetrated the joint <0.80 mm are marked as vis (visible).
Table 4.
Olecranon Plate Sensitivity, Specificity, Positive Predictive Values, and Negative Predictive Values.
| Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | |
|---|---|---|---|---|
| Crepitus | ||||
| Position o-1 | 71.4 | 100.0 | 100.0 | 60.0 |
| Position o-2 | 68.2 | 100.0 | 100.0 | 53.3 |
| Position o-3 | 79.0 | 100.0 | 100.0 | 73.3 |
| Total | 72.6 | 100.0 | 100.0 | 62.2 |
| Radiographs | ||||
| Position o-1 | 60.6 | 66.7 | 83.3 | 38.1 |
| Position o-2 | 30.3 | 75.0 | 76.9 | 28.1 |
| Position o-3 | 77.2 | 78.8 | 86.3 | 66.7 |
| Total | 55.0 | 74.1 | 83.2 | 41.4 |
Radiographic Analysis
The overall sensitivity and specificity of radiographic analysis of the radial head plate was found to be 72.4% and 85.6%, respectively. There was not a notable difference in specificity and sensitivity between the 2 screw positions assessed on the radial head plate (see Table 2). The overall sensitivity and specificity of radiographic analysis of the olecranon plate was found to be 55.0% and 74.1%, respectively. The sensitivity of the radiographs taken of position o-2 was 30.3%, compared with 60.1% for position o-1 and 77.2% for position o-3 (see Table 4).
The kappa statistic for each reviewer was 0.77, 0.73, and 0.90 for the radial head plate and 0.77, 0.87, and 0.71 for the olecranon plate demonstrating a substantial degree of intraobserver agreement (see Table 5). The averaged Fleiss kappa statistic for both viewings was 0.76 and 0.80 for the radial head plate and 0.67 and 0.69 for the olecranon plate, demonstrating a moderate to substantial degree of interobserver reliability (see Table 6).
Table 5.
Intraobserver Reliability.
| Surgeon | Radial head |
Olecranon plate |
||
|---|---|---|---|---|
| κ | 95% CI | κ | 95% CI | |
| 1 | 0.77 | 0.61-0.93 | 0.70 | 0.55-0.85 |
| 2 | 0.73 | 0.56-0.90 | 0.87 | 0.76-0.97 |
| 3 | 0.90 | 0.79-1.00 | 0.71 | 0.57-0.85 |
Note. CI, confidence interval.
Table 6.
Interobserver Reliability.
| Viewing | Radial head |
Olecranon plate |
||
|---|---|---|---|---|
| Fleiss κ | 95% CI | Fleiss κ | 95% CI | |
| 1 | 0.76 | 0.61-0.90 | 0.67 | 0.55-0.79 |
| 2 | 0.80 | 0.65-0.94 | 0.69 | 0.57-0.81 |
Note. CI, confidence interval.
Discussion
With improved instrumentation and surgical technique, ORIF of 2 and 3 part radial head fractures has been shown to provide patients with better functional results when compared with radial head excision or radial head replacement.27 The surgical exposure required to fix a radial head is often limited, as a more extensile dissection to improve visualization may further destabilize an already compromised elbow joint. As such, it can be difficult to evaluate the entirety of the articular surface of the radial head, specifically with respect to screw penetration.
Similarly, plate fixation has become the recommended treatment for olecranon fractures with significant comminution, oblique fractures exiting distal to the coronoid, and Monteggia fractures.12 Recent evidence has also included fractures associated with elbow dislocation.22,30 The main complication associated with plate fixation is hardware prominence that often requires plate removal but, as in all peri-articular fractures, care must be taken to prevent screw penetration.2,7 Screw prominence of the UHJ is particularly difficult to evaluate on standard AP/lat/oblique X-ray films because the trochlear notch is bisected by an elevated guiding ridge that splits the notch into medial (ulnar) and lateral (radial) parts. The ridge is elevated with respect to the medial and lateral articular surface and may overlap or hide a prominent screw on a lateral or oblique radiograph.
Our results are the first to define the sensitivity of standard intraoperative diagnostic tests (radiographs and clinical exam) in assessing screw penetration in the UHJs and PRUJs. The sensitivity of crepitus was 81.1% for screws in the radial head plate and 72.6% for screws in the olecranon plate. The sensitivity of radiographs was 72.4% for the screws in the radial head plate and 55.0% for screws in the olecranon plate. It should be mentioned that the sensitivity of crepitus in detecting the penetration of screws into their respective joints is affected by the fact that the positive predictive value of this test is 100%, as was to be expected given that there was no other possible cause of crepitus in the context of this study (ie, degenerative joints or loose or foreign bodies). Overall, the usefulness of crepitus and radiographic assessment as means of intraoperative evaluation of screw prominence is moderate and care must be taken in interpreting negative results.
Specific to the radial head plate, 23% of the screws were shown to have penetrated into the PRUJ and yet produced no crepitus on PROM. With respect to the olecranon plate, 29% of the screws penetrated the UHJ and another 9% penetrated the PRUJ without discreet crepitus. Of these screws, 35% were placed in position o-1, 41% in position o-2, and 24% in position o-3. This demonstrates that screws placed in certain locations are more likely to penetrate their respective joints and go undetected by standard means of assessment in a surgical setting. The most problematic screws were located in the proximal screw cluster of the olecranon plate in the area of the previously described guiding trochlear ridge. The finding is further supported as screw position o-2 had the lowest sensitivity on radiographic exam of 30.3%. Although it is possible that this finding is implant specific, we believe this observation can be applied to multiple systems as position o-2 can be generalized to represent the position at which the trochlear ridge is the highest.
The amount of screw penetration was variable and ranged from just visible to 1.57 mm above the joint surface. Although it is possible that a screw with minimal prominence (vis) has no clinical impact, it is also possible that as the patient ages and cartilage thins, a barely prominent screw might become more prominent and may contribute to an accelerated degenerative process. The clinical implication of these particular results is not known; however, elbow stiffness after ORIF has been well documented and is presumed to occur from nonunion, migration of hardware, degenerative arthritis, and/or osteonecrosis.25,27,28
The radiographic data suggest there is substantial difficulty in the assessment of UHJ penetration with olecranon plates and to a lesser degree PRUJ penetration with olecranon and radial head plates. Coupled to the difficulty in assessing screw penetration using clinical exam, namely, crepitus, surgeons likely need to substantially decrease screw lengths or use alternate views to evaluate screw prominence. The costs and benefits of using shorter screw lengths must be calculated as these fractures are often times very comminuted and adequate fixation may mean the difference of a couple more threads crossing the fracture line.
In a previously published article, the lateral views were not sensitive enough to detect screw penetration.1 This study found that using multiple positions of rotation in the AP view was a relatively reliable method for detecting screw penetration of the radial head in an operative setting. In the current study a finding that was noted incidentally was the relative ease with which screw prominence can be evaluated in the PRUJ using the fully pronated lateral view compared with the hypersupinated oblique. This observation is one the authors plan to explore in a future study.
Other literature supports the conclusions of the authors that certain screw locations are more difficult to evaluate than others and may go undetected by standard means of assessment. According to Matthews et al routine radiographs are usually sufficient for follow-up exam after olecranon osteosynthesis. However, for cases where the patient exhibits impaired forearm rotation accompanied by noticeable crepitation, they recommend acquiring a three-dimensional computed tomographic scan of the elbow to help visualize possible anterior protrusion of Kirschner wires or screws that may have been undetectable on plain AP and lateral radiographs.22
The limitations of this study are inherent in design that was cadaver based. The in vivo assessment for crepitus may be more sensitive although no data exist to validate this assumption. Crepitus was evaluated by 3 separate orthopedic residents but to standardize the evaluation, all 3 had to agree if crepitus was present or absent. Two cadavers were noted to have mild cartilage wear that may confound the clinical evaluation for crepitus but contrary to the results, this would have underestimated the minimal screw length required to cause crepitus. Finally, plating was not done on fractures or simulated fractures. It is reasonable to assume that fractures and fracture pieces may also simulate crepitus when there is no screw prominence and may make fluoroscopic assessment even more difficult. Therefore, the difficulty in evaluating for screw penetration is likely underestimated by our results.
The final limitation involves the fact that we only examined screw positions on one plating system, which may cause some restrictions in generalizing our results to other radial head and olecranon plates. However, due to the standard position of screws relative to certain anatomical landmarks, we feel our data are relevant in a broader context.
In conclusion, our study confirms the hypothesis that clinical exam and radiographic assessment may not be sensitive enough to accurately exclude screw penetration during olecranon and radial head ORIF. We have identified at least one position on the olecranon locking plate that should be carefully scrutinized for long screws.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was generously supported by a donation of equipment by the Acumed Company.
References
- 1. Abdelgawad AA, Hussain A, Ebraheim NA. Screw fixation of the radial head: radiological assessment of the proximal radio-ulnar joint and average radial head diameter-an anatomic study. Arch Orthop Trauma Surg. 2010;130(4):465-467. doi: 10.1007/s00402-009-0922-9. [DOI] [PubMed] [Google Scholar]
- 2. Anglen JO, DiPasquale T. The reliability of detecting screw penetration of the acetabulum by intraoperative auscultation. J Orthop Trauma. 1994;8(5):404-408. [DOI] [PubMed] [Google Scholar]
- 3. Bailey CS, MacDermid J, Patterson SD, King GJ. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. 2001;15(8):542-548. [DOI] [PubMed] [Google Scholar]
- 4. Bengard MJ, Gardner MJ. Screw depth sounding in proximal humerus fractures to avoid iatrogenic intra-articular penetration. J Orthop Trauma. 2011;25(10):630-633. doi: 10.1097/BOT.0b013e318206eb65. [DOI] [PubMed] [Google Scholar]
- 5. Boyer M, Korcek K, Gelberman R, Gilula LA, Ditsios K, Evanoff BA. Anatomical tilt X-rays of the distal radius: an ex vivo analysis of surgical fixation. J of Hand Surg. 2004;24:116-122. doi: 10.1016/j.jhsa.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 6. Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Joint Surg Am. 2009;91:2416-2420. doi: 10.2106/JBJS.H.01419. [DOI] [PubMed] [Google Scholar]
- 7. Donegan RP, Bell J-E. Olecranon fractures. Oper Tech Orthop. 2010;20:17-23. doi: 10.1053/j.oto.2009.09.016. [DOI] [Google Scholar]
- 8. Edwards SG, Cohen MS, Lattanza LL, et al. Surgeon perceptions and patient outcomes regarding proximal ulna fixation: a multicenter experience. J Shoulder Elbow Surg. 2012;21:1637-1643. doi: 10.1016/j.jse.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 9. Erturer RE, Sever C, Sonmez MM, Ozcelik IB, Akman S, Ozturk I. Results of open reduction and plate osteosynthesis in comminuted fracture of the olecranon. J Shoulder Elbow Surg. 2011;20(3):449-454. doi: 10.1016/j.jse.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 10. Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971;76(5):378-382. [Google Scholar]
- 11. Giannicola G, Manauzzi E, Sacchetti FM, et al. Anatomical variations of the proximal radius and their effects on osteosynthesis. J Hand Surg Am. 2012;37(5):1015-1023. doi: 10.1016/j.jhsa.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 12. Gordan MJ, Budoff JE, Yeh ML, Luo ZP, Noble PC. Comminuted olecranon fractures: a comparison of plating methods. J Shoulder Elbow Surg. 2006;15(1):94-99. doi: 10.1016/j.jse.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 13. Hak DJ, Golladay GJ. Olecranon fractures: treatment options. J Am Acad Orthop Surg. 2000;8:266-275. [DOI] [PubMed] [Google Scholar]
- 14. Herbertsson P, Per-Olif H, Hasserius R, et al. Uncomplicated mason type-II and III fractures of the radial head and neck in adults: a long-term follow-up study. J Bone Joint Surg Am. 2004;86(3):569-574. [DOI] [PubMed] [Google Scholar]
- 15. Ikedo M, Sugiyama K, Kang C, Takagaki T, Oka Y. Comminuted fractures of the radial head: a comparison of resection and internal fixation. J Bone Joint Surg Am. 2006;87:76-84. doi: 10.2106/JBJS.E.00841. [DOI] [PubMed] [Google Scholar]
- 16. Joglekar SB, Hyas AM. The role of locking technology in the upper extremity. J Hand Microsurg. 2009;1(2):82-91. doi: 10.1007/s12593-009-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Karlsson MK, Kasserius R, Karlsson C, Besjakov J, Josefsson PO. Fractures of the olecranon: a 15- to 25-year follow up of 73 patients. Clin Orthop Relat Res. 2002;204:205-212. doi: 10.1097/01.blo.0000022181.66847.50. [DOI] [PubMed] [Google Scholar]
- 18. Kass L, van Riet RP, Vroemen JP, Eygendaal D. The epidemiology of radial head fractures. J Shoulder Elbow Surg. 2010;19:520-523. doi: 10.1016/j.jse.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 19. King GJW, Evans DC, Kellam JF. Open reduction and internal fixation of radial head fractures. J Orthop Trauma. 1991;5:21-28. [DOI] [PubMed] [Google Scholar]
- 20. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. [PubMed] [Google Scholar]
- 21. Lindenhovius AL, Felsch Q, Ring D, Kloen P. The long-term outcome of open reduction and internal fixation of stable displaced isolated partial articular fractures of the radial head. J Trauma. 2009;67:143-146. doi: 10.1097/TA.0b013e31818234d6. [DOI] [PubMed] [Google Scholar]
- 22. Matthews F, Trentz O, Jacob AL, Kikinis R, Jupiter JB, Messmer P. Protrusion of hardware impairs forearm rotation after olecranon fixation: a report of two cases. J Bone Joint Surg Am. 2007;89(3):638-642. doi: 10.2106/JBJS.E.01238. [DOI] [PubMed] [Google Scholar]
- 23. Pike JM, Athwal GS, Faber KJ, King GJ. Radial head fractures—an update. J Hand Surg. 2009;34:557-565. doi: 10.1016/j.jhsa.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 24. Pike JM, Grewal R, Athwal GS, Faber KJ, King GJ. Open reduction and internal fixation of radial head fractures: do outcomes differ between simple and complex injuries? Clin Orthop Relat Res. 2014;472:2120-2127. doi: 10.1007/s11999-014-3519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Puchwein P, Schildhauer TA, Schoffmann S, Heidari N, Windisch G, Pichler W. Three-dimensional morphometry of the proximal ulna: a comparison to currently used anatomically preshaped ulna plates. J Shoulder Elbow Surg. 2012;21:1081-1023. doi: 10.1016/j.jse.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 26. Ring D. Displaced, unstable fractures of the radial head: fixation vs. replacement—what is the evidence? Injury. 2008;39(12):1329-1337. doi: 10.1016/j.injury.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 27. Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84(10):1811-1815. [DOI] [PubMed] [Google Scholar]
- 28. Ruchelsman DE, Christoforou D, Jupiter JB. Fractures of the radial head and neck. J Bone Joint Surg. 2013;95(5):469-478. doi: 10.2106/JBJS.J.0198. [DOI] [PubMed] [Google Scholar]
- 29. Sahajpal D, Wright T. Proximal ulna fractures. J Hand Surg. 2009;34:357-362. doi: 10.1016/j.jhsa.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 30. Smith GR, Hotchkiss RN. Radial head and neck fractures: anatomic guidelines for proper placement of internal fixation. J Shoulder Elbow Surg. 1996;5:113-117. [DOI] [PubMed] [Google Scholar]


