Abstract
Purpose
There is a need for research to facilitate the widespread implementation, dissemination, and sustained utilization of evidence-based primary care screening, monitoring, and care coordination guidelines, thereby increasing the impact of dental hygienists’ actions on patients’ oral and general health. The aims of this formative study are to: (1) explore dental hygienists’ and dentists’ perspectives regarding the integration of primary care activities into routine dental care; and (2) assess the needs of dental hygienists and dentists regarding primary care coordination activities and use of information technology to obtain clinical information at chairside.
Methods
This qualitative study recruited ten hygienists and six dentists from ten New York City area dental offices with diverse patient mixes and volumes. A New York University faculty hygienist conducted semi-structured, in-depth interviews, which were digitally recorded and transcribed verbatim. Data analysis consisted of multilevel coding based on the Consolidated Framework for Implementation Research, resulting in emergent themes with accompanying categories.
Results
The dental hygienists and dentists interviewed as part of this study fail to use evidence-based guidelines to screen their patients for primary care sensitive conditions. Overwhelmingly, dental providers believe that tobacco use and poor diet contribute to oral disease, and report using electronic devices at chairside to obtain web-based health information.
Conclusion
Dental hygienists are well positioned to help facilitate greater integration of oral and general health care. Challenges include lack of evidence-based knowledge, coordination between dental hygienists and dentists, and systems-level support, with opportunities for improvement based upon a theory-driven framework.
Keywords: Dental Hygienist, Primary Care, Interoperability, Technology, Evidence-based Guidelines, Chairside Screening
INTRODUCTION
US national health care reform presents the dental profession with new opportunities to examine its current place and future role in the healthcare environment. Scope of practice concerns are at the heart of the debate.1,2 Oral health care providers--notably dental hygienists and dentists--are poised to contribute substantially to innovative service delivery models that stress prevention and integrate primary care with oral health services.3,4 This designation is critically important given the aging of the US population. Increased numbers of patients with chronic conditions are expected that will benefit from patient-centered, evidence-based screening, monitoring, and care coordination.5 Moreover, as authoritatively documented by the Institute of Medicine, oral health and general health are inextricably linked.6 Notably, diabetes is a risk factor for periodontal disease and, when poorly controlled, can complicate periodontal treatment outcomes.7
According to the US Department of Labor, there were 196,520 licensed dental hygienists and 97,990 general dentists employed in the United States in 2014.8 With 9,960 licensed dental hygienists in New York State (NYS) and 48 active dental hygienists per 100,000 population in 2011, NYS is consistent with the national average of 50 dental hygienists per 100,000 population, notwithstanding wide regional variation.9 The vast majority (95%) of dental hygienists in NYS work in private dental offices,8 underscoring the importance of targeting this setting. Thus, the potential impact of supporting dental hygienists to undertake primary care activities at chairside on the health of both NYS and US residents overall is substantial, especially for populations with limited access to primary care providers.
An urgent need exists to expand the primary care workforce, given the considerable increase in patient volumes now being realized with mandatory insurance provisions that have taken effect under the Patient Protection and Affordable Care Act.10 Evidence-based approaches to implement dental office system changes that take into account the resource, staffing, and time constraints that dental hygienists and dentists face may be one potential mechanism for leveraging oral health providers to conduct primary care activities in dental offices. Evidence-based primary care guidelines are not yet a standard part of dental visits. Yet until care coordination activities between dental and medical providers are closely integrated, the potential of dentists to “scope up,” as it were, to become a more active part of the primary care workforce, and “scope down” to dental hygienists certain primary care screening, monitoring, and care coordination functions will remain untapped.2
Our rationale for this study is that dental hygienists want to more actively engage with their patients around the prevention of and screening for diabetes and hypertension. They also seek to gain confidence in providing tobacco cessation services and nutrition counseling. Accordingly, they need simple, evidence-based tools that—with training and technical assistance—they can implement with the time and resources available to them during dental visits.11–18 The development of a web-based clinical decision support tool for use by dental hygienists at chairside has the potential to augment the primary care workforce, improve screening for primary care sensitive conditions, provide decision support for evidence-based patient management, improve coordination of care through timely referrals, and ensure greater consistency in the delivery of health promotion and disease prevention in dental settings, as per findings in community health centers.19,20 In essence, a web-based CDSS is an information technology-based system designed to provide expert support to improve clinical decision-making. But to translate into improved patient care outcomes, formative studies are needed of the dental practice environment to adapt the technology to the intended setting.
This is critical, as many adults visit a dental office in a given year, but not a primary health care professional,21 providing an opportunity to leverage dental providers to meet general health needs. The approximately 196,520 dental hygienists in the United States are especially well situated to serve as patient care coordinators and positively influence quality of care, notably for low-income and older adult patients who may require assistance in navigating the health care system. Often interacting with patients during long appointment sessions and over extended periods of time, dental hygienists' education in and knowledge of the oral-general health connection enables them to provide trusted, patient-centered care.22 Their scope of practice typically involves: taking a comprehensive health history, including medications and therapies; screening for early stages of disease, e.g., taking blood pressure and pulse readings); and assuming a primary role in patients’ oral-general health education.
There is a need for research to facilitate the widespread implementation, dissemination, and sustained utilization of evidence-based primary care screening, monitoring, and care coordination guidelines, thereby increasing the impact of dental hygienists’ actions on patients’ oral and general health. The aims of the formative study presented here are to: (1) explore dental hygienists’ and dentists’ perspectives regarding the integration of primary care activities and routine dental care; and (2) assess the needs of dental hygienists and dentists regarding primary care coordination activities and use of information technology to obtain clinical information at chairside.
METHODS AND MATERIALS
Conceptual Framework
The conceptual framework informing this research is the Consolidated Framework for Implementation Research (CFIR).23 A CFIR technical assistance website is available for individuals considering using the CFIR to evaluate an implementation or design an implementation study.24 The CFIR provides a menu of constructs that have been associated with effective implementation and can be used in a range of applications.24 For instance, culture and tension for change are part of the inner setting domain; knowledge and beliefs about the intervention and self-efficacy are part of the characteristics of individuals domain.
Figure 1a presents the five major domains of the CFIR (the intervention, the inner and outer setting, the individuals involved, and the process by which implementation is accomplished), and Figure 1b identifies these domains for the research at hand (primary care coordination, dental and primary care practices, dental providers and patients, and the implementation process).
Figure 1.
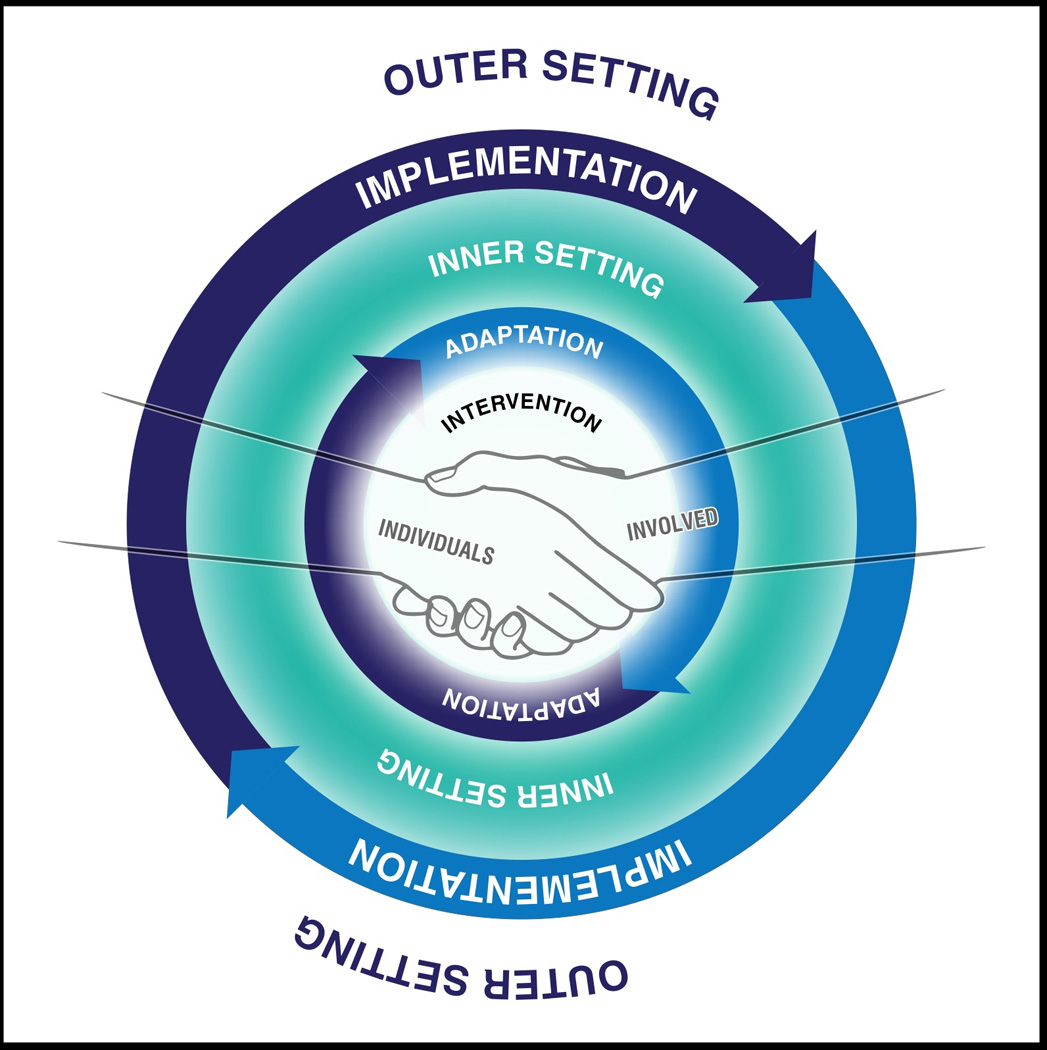
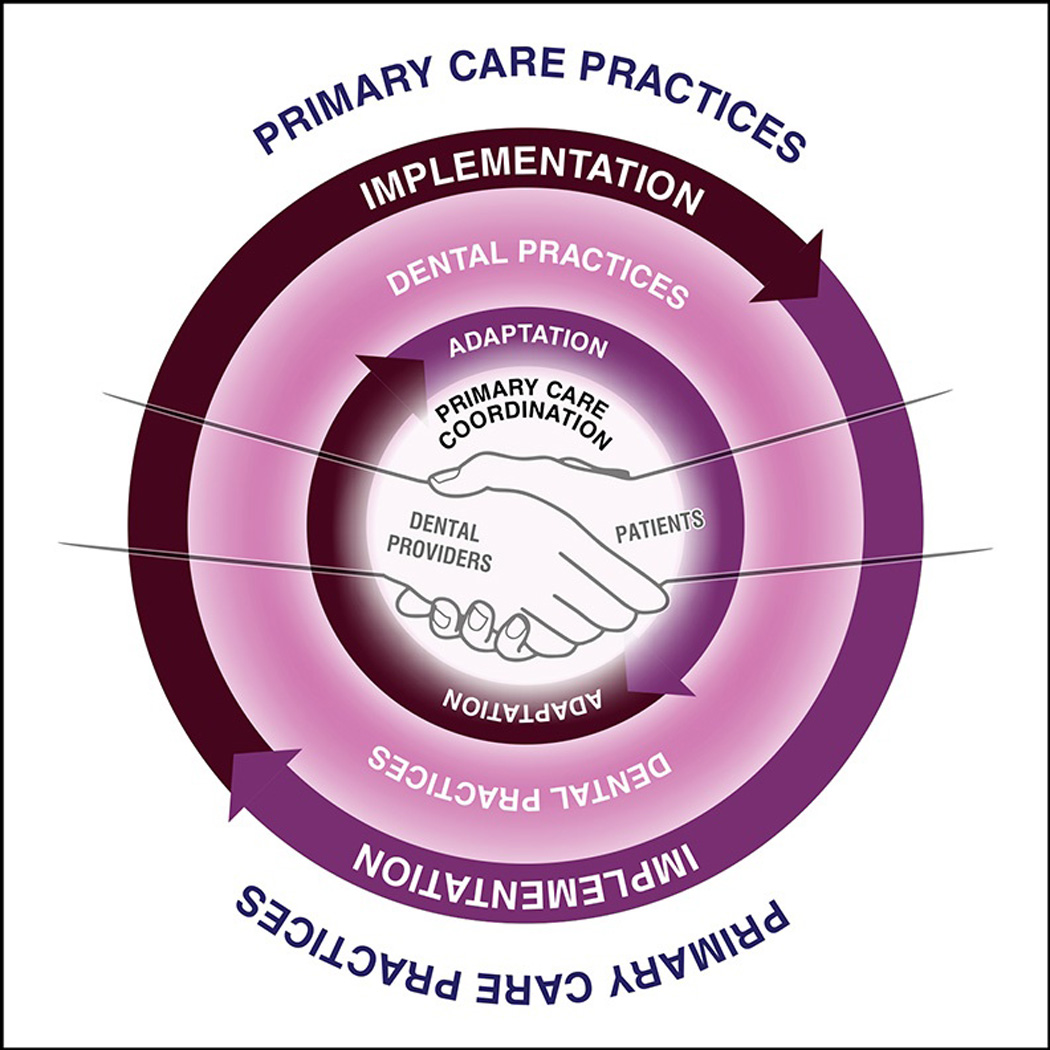
The five major domains of the Consolidated Framework of Implementation Research (CFIR), displayed for both a general implementation science scenario (Figure 1a) and the present study (Figure 1b). Adapted from Damschroder et al.23
The figures are necessarily simplifications of complicated implementation processes and the domains involved. These are elaborated elsewhere.23,24 We elected to be concrete to aid understanding. Hence, the domains depicted in Figure 1b and discussed next ought to be interpreted as examples, rather than comprehensive renderings.
This study is centrally focused on the views of dental providers. Nonetheless, improving the health and well-being of patients is the mission of all health care entities,23 and patient attitudes and characteristics may influence provider behavior. Hence, Figure 1b overtly depicts dental providers working hand-in-hand with patients to enhance primary care coordination at chairside.
Also explicitly included in both Figures 1a and 1b is the process of adaptation. According to Damschroder and colleagues, absent adaptation, interventions are usually a poor fit for any given setting.23 Thus, they are often resisted by the individuals who will be affected by the intervention.23 To address this challenge, we conducted the following formative research study to gain the views of dental providers on primary care coordination at chairside before designing a clinical decision support tool with their active engagement.
Research Design and Informed Consent Procedures
This exploratory pilot study design utilized an innovative and adaptive qualitative approach. The study was descriptive in design and drew on purposive sampling25 of dental providers within the investigators’ networks to examine the perspectives of dental hygienists and dentists regarding the integration of primary care activities into routine dental care. This multi-site study employed maximum variation sampling to recruit dental hygienists (n=10) and dentists (n=6) from heterogeneous New York City area dental offices (n=10) representing diverse patient mixes and volumes, practice types, and neighborhood contexts.
Purposeful sampling of information-rich cases facilitates gaining in-depth knowledge, maximizing variation/heterogeneity of perspectives and experiences of the research topics at hand, and ensuring cross-location comparability and generalizability of the data. Participants were selected to establish a typical sample in order to gain a rich and varied description of dental hygienists’ and dentists’ experiences of their work environment from informants who were willing to openly discuss these issues.25
At the beginning of each interview session, informed consent and Health Insurance Portability and Accountability Act (HIPAA) authorization forms were distributed and signed by the participants. These forms assured participants that the information they provided would be kept confidential and explicated the scope, aims, methods, and participation conditions of the study. The participants were also informed that they were free to withdraw from the study at any time, and that they would be compensated $50 for their participation.
Key Informant Interviews
A New York University faculty dental hygienist conducted semi-structured, in-depth interviews, which were digitally recorded and transcribed verbatim. Ten interviews were conducted with dental hygienists and six interviews were conducted with dentists to ask them their opinions about working with their patients to identify and manage diabetes (high blood sugar), hypertension (high blood pressure), use of tobacco products such as cigarettes and cigars, and problem areas of their diets such as heavy consumption of sugary drinks, all of which may lead to oral health care problems.
The interviewer utilized a topic guide that was comprised of non-directive questions, which sought to elicit accounts or descriptions of standard care dynamics and the potential utility of an electronic clinical decision support tool. The topic guide was based upon CFIR constructs23,24 and refined according to the expert input of the research team and senior advisory board members. Items queried about included: current practices regarding primary care screening, management, and care coordination activities for diabetes and hypertension; activities conducted and referrals made for smoking cessation and nutrition counseling; the physical environment and social context of the dental offices; patient management services and systems; structural barriers to technology adoption; and perceived and actual challenges to primary care screening at chairside. Each interview lasted from 45 to 60 minutes.
The recorded interviews were then uploaded onto a secure website and transcribed verbatim by a professional firm. Upon receipt, each transcript was read by at least two study personnel and every interview digital file was played back in order to increase understanding of the nuances of the research participants’ language and meanings and attend more closely to respondents’ feelings and views.
Qualitative Analysis
The study team has developed a method of conducting thematic content analysis of qualitative text that allows for the systematic identification of themes present, reveals the relationships among these themes while keeping them in context, and ensures that the codes and their application to the text are valid and reliable (see also below).26–30 ATLAS.ti qualitative data software, version 7, was used as a data management tool to facilitate data retrieval, coding, thematic analysis, memos, and displays as part of the analysis.31
First, a “start list” of a priori codes (that is, prior to beginning the analysis) was created based on questions and topics from the research instrument. Respective themes were developed by the study team members, who included dental hygienists and dentists, after conducting an in-depth literature review on relevant topics, holding discussions with other oral health professionals (including experts that served as senior advisory board members), and envisioning characteristics and dynamics related to facilitating the greater integration of oral and general health care. As part of the descriptive level of analysis, in vivo codes or indigenous categories were incorporated, which are concepts that use the actual words of the research participants rather than being named by the researchers.32
Following the first cycle coding method, or initial coding, focused coding was employed as a second cycle analytic process.30 Focused coding searches for the most frequent or significant initial codes to develop the most salient categories in the data corpus and requires decisions about which initial codes make the most analytic sense.29 Each incident in the data is compared with other incidents for similarities and differences. Incidents found to be conceptually similar are grouped together under a higher-level descriptive content. Theoretical coding then assisted in specifying the potential relationships between categories and shifting the analytic narrative toward a CFIR theoretical orientation.30
Emergent Themes
Data analysis consisted of multilevel coding, which resulted in emergent themes with accompanying categories. Eight to ten generalized codes were identified that generally corresponded to the primary domains of the topic guide. Content analysis guided the development, testing, and refinement of a coding scheme that enabled systematic identification and conceptual definition of the main themes and subthemes displayed in the transcripts, along with the relationships among the themes. Because the investigators were interested in similarities and differences between the views of dental hygienists and the views of dentists, the number of dental hygienists and the number of dentists who endorsed each theme were totaled separately, and quotes were selected and identified by the individuals involved (dental hygienists or dentists) to both illustrate the theme and present any alternate views.
RESULTS
Study Participant Characteristics
The self-reported characteristics of the dental hygienists and dentists who participated in the key informant interviews, along with salient information about the dental offices where they practice, are provided in Table 1.
Table 1.
Self-reported characteristics of dental hygienists and dentists who participated in key informant interviews and the dental offices where they practice, New York Metropolitan Area, 2013.
| Characteristic | Dental Hygienists (n=10) | Dentists (n=6) | ||
|---|---|---|---|---|
| Mean (SD) |
Median (Range) |
Mean (SD) |
Median (Range) |
|
| Number of years of professional experience | 10.8 (10.8) | 6 (2–33) | 32.8 (5.1) | 33.5 (28–40) |
| Number of patients treated daily | 11.4 (5.9) | 10 (6–30) | 8.4 (1.0) | 8 (7–10) |
| Number of dental professionals per office | 6 (3.8) | 4 (3–16) | 6.3 (4.3) | 4.5 (4–16) |
| Minutes allotted per patient | 46.2 (15.1) | 47.5 (17.5–60) | - | - |
| n (%) | n (%) | |||
| Accepts Medicaid | 2 (20%) | 0 (0%) | ||
| Accepts private dental insurance | 7 (70%) | 3 (50%) | ||
| Group practice* | 2 (20%) | 2 (33%) | ||
| General practice* | 5 (50%) | 2 (33%) | ||
| Holistic practice* | 1 (10%) | 1 (17%) | ||
| Prosthodontics practice* | 5 (50%) | 2 (33%) | ||
| Owns a smartphone | 10 (100%) | 6 (100%) | ||
| Owns both a smartphone and a tablet | 4 (40%) | 3 (50%) | ||
More than one type of practice may apply
Notably, the dentists interviewed had considerably more years of professional experience than did the dental hygienists interviewed. This also speaks to the eras when these dental practitioners were trained (three or four decades ago for the dentists versus less than a decade ago to three decades ago for the dental hygienists). Few dental providers interviewed work in offices that accept Medicaid, and only about one-half work in dental offices that accept private insurance. A range of practice types were represented in the study sample, meaning that the purposive sampling was effective in gaining input from dental providers who work in a variety of dental offices. Finally, all of the participants reported owning smartphones, meaning that they had the technological capability of accessing health information or using a clinical decision support system at chairside.
Qualitative Findings
The main findings of the key informant interviews with dental professionals are summarized in Table 2, along with illustrative quotes that support the findings, and alternate view quotes, where applicable.
Table 2.
Summary of main findings of key informant interviews with dental professionals,* New York Metropolitan Area, 2013.
| Main finding | Number of interviews with hygienists where finding was endorsed |
Number of interviews with dentists where finding was endorsed |
Total number of interviews where finding was endorsed |
Illustrative quotes from hygienists and dentists |
Alternate view quotes from hygienists and dentists, where applicable |
|---|---|---|---|---|---|
| Screening for diabetes and hypertension is not especially relevant for the dental practices where the participating dental providers work |
6/10 | 3/6 | 9/16 | HYGIENIST: On a scale from one to ten, barely average, because most of our clientele are working professionals who tend to be a little bit more active. Any health situation that they have, they usually have taken advantage of their insurance and had it checkin’ out, so they bring it to our attention gladly. DENTIST: I don't generally screen myself. If we were suspect—in other words, if something happened, and it had not initially been reported in a medical history, we would, therefore, maybe have them checked at that point. |
HYGIENIST: I think it’s very important. The patients don’t see their doctors usually, so since they see us more we would make a change for ‘em. DENTIST: I think it’s very important to do that [screen for hypertension]. Obviously, in our profession, we can’t really work on someone who is not stable. It will surface in a sense of lots of factors— stress, anxiety, bleeding, and other factors. It can affect the type of anesthesia we use, of course, in order to still perform that particular procedure that day, so I think it’s important to screen for it, yes. Yeah. |
| Patients were generally responsive to being offered referrals to primary care providers by dental providers |
7/10 | 6/6 | 13/16 | HYGIENIST: They like that they’re being taken care of. DENTIST: If there’s a problem and I see that there might be something that I don’t feel comfortable with or that the patient should be address, either somehow they’re not feeling good and for some reason that day it seems like it may be an issue and we took their blood pressure and we tell them they better go to see somebody today, yeah, we go ahead and usually have pretty good compliance. Oh, I didn’t know that doc, thank you very much. Let me go ahead and see somebody in the next week or so or that day. Yeah, generally, I don’t get hassled. Once in a while in the past, I don’t know, people might follow-up, not follow-up, but in general, people take our advice. Yeah, yeah. |
HYGIENIST: Not too happy. Because they think that we are exaggerating. They think that is irrelevant to their dental visit. |
| Dental providers do not always encourage testing for patients who have not been screened for diabetes or hypertension |
5/10 | 6/6 | 11/16 | HYGIENIST: I have. Not on a regular basis, but I have especially if there’s some kind of oral implication or I get some other kind of cues then I will, but not on a regular basis. DENTIST: I guess it depends on the patient's age, sex, risk, again family history. There's a part on there. We don't necessarily encourage it unless there's—we're assuming that they're under medical care and that they're being screened for all that. |
HYGIENIST: Yes. I definitely. Even when they don't have a medical doctor listed, I encourage them to go see somebody at least once a year. If I felt like maybe they were describing some symptoms, then I would say, you know, it would be a good idea to go see your primary care physician. |
| Participating dental providers infrequently see oral disease that they believe is related to diabetes or hypertension |
7/10 | 4/6 | 11/16 | HYGIENIST: Well, I mean I don’t have a lot of patients who have diabetes that I know of, but those who have it, it’s very relevant. They definitely have oral conditions related to their diabetes. DENTIST: How often do I see hypertension issues, high blood pressure problems, tissue, anxiety, bleeding? Not too often. Not too often do I see someone that has hypertension issues. I don’t know. If I threw out a number like, I don’t know, I don’t know. I’d say about 20, 25 percent off the top of my head. If I look in the chart and see they’re hypertensive, that’s probably my answer. All right? |
HYGIENIST: I would say often, but because it's related to their medication. I see dry mouth a lot, xerostomia, because of the medication that people are on for diabetes and hypertension. DENTIST: Good percentage of the periodontal cases probably have some diabetes or pre- diabetic, anybody over 40, let’s say. |
| Participating dental providers counsel patients in the hypertensive range only insofar as referring them to see their primary care physicians |
7/10 | 5/6 | 12/16 | HYGIENIST: How I consult? Like I say before if I know they are taking the medication and they still have some problems I can reinforce on the going back to the doctor for changing the medication. DENTIST: I don’t really counsel them. No. Well again, only if they’re uncontrolled. Then I definitely counsel them to see their physicians, but no. Not specific in terms of what they should be doing. |
HYGIENIST: Diet, exercise, have a physical to have it definitely checked by their physician. I counsel them that this needs to be addressed immediately. I make it a matter of urgency. DENTIST: Diet. Lifestyle. Diet, lifestyle, and referral. |
| Participating dental providers do not cite evidence-based guidelines in deciding what blood pressure reading is too high to perform dental treatment |
10/10 | 6/6 | 16/16 | HYGIENIST: I guess no matter which reading I get, if I felt like anything was over like 140 over 90, I would have to ask my doctor, and she would let me know whether what she felt was okay to treat. In my own opinion? To be honest, I guess I would say like, I mean, 90 is pretty high. I would say like maybe 155 over like 95 or something or a hundred. Something like that would make me really nervous. No. DENTIST: Yeah. Yes. Yes, there is, and I—but I must admit that I don’t routinely screen for high blood pressure either. I would say I’d be very—I’d be concerned about anything systolic of 160 and above. |
|
| Participating dental providers believe that it is important for their dental colleagues to screen and treat for tobacco use |
7/10 | 4/6 | 11/16 | HYGIENIST: I’d say pretty important. It’s very—smoking brings about many risk factors for health in general, so it’s a good idea to. Not if it makes more work for them. [Laughs] DENTIST: I think it’s, again, if it’s any practice, group practice, and I guess we’re out there as practitioners, healers, in society, we should continue to spread the word and educate the population that smoking is not good for you and do our best to try to cut it down amongst our whole population in the office that we see. |
HYGIENIST: ‘Cause it seems to be something that has to happen outside of the office, and which [sighs]—there’s no monetary benefit. DENTIST: Some say, “I’d like to try. What do you have to offer?” Others say, “I’m still just gonna keep doing it. Give me some paperwork and stuff,” and then they just walk out of the office. I think that most of ‘em agree that it’s not good for them, but it’s difficult to motivate people to try to stop smoking, be it through mechanisms of paperwork, literature, chewing gums, or maybe giving ‘em something a little stronger. |
| Participating dental providers often see dental disease that they believe is related to poor diet |
6/10 | 3/6 | 9/16 | HYGIENIST: I would say often. Not all the time, but I do think that there are some patients that because of their diet they're at a higher risk for caries. If they have any health issues, it just exacerbates like the whole. They're at risk for decay. DENTIST: Often. In the college age student, they go off with perfect teeth and come back with all sorts of trouble from late nights with a bottle of Coke and M&M's. |
HYGIENIST: Children will be more of an issue or place where I would see that, but we don’t see that many children. DENTIST: Not very often, but every once in a while. |
| Participating dental providers use their phones or other devices at chairside to obtain clinical information related to the care of their patients |
9/10 | 5/6 | 14/16 | HYGIENIST: WebMD. WebMD and PubMed…But honestly, I use a search engine, and then I go to like a couple different ones to get what I'm looking for. DENTIST: I have Hippocrates on my phone to look up drugs, but generally I don’t use it much more [than] that. |
HYGIENIST: Not really. I’m a hygienist, 30 years. A hygienist. 30 years, okay? I pretty much go with what I know. [Laughing together] I’m being really honest. If I get stumped, I will Google a word or a topic, but I pretty much go with what I know. Not really, no. DENTIST: You know, it’s interesting. I don’t necessarily go online. I come to the school since we’re fortunate to work in a faculty practice I’ll go to my colleagues who are oral surgeons or oral medicine. I speak to them direct. I figure I’ll go to them direct. They know more than I do… |
Ten key informant interviews were conducted with dental hygienists and six key informants interviews were conducted with dentists.
Screening for Diabetes and Hypertension
At the time the key informant interviews were conducted (2013), screening for diabetes and hypertension was not deemed by the participants to be especially relevant for the dental practices where they worked.
HYGIENIST: On a scale from one to ten, barely average, because most of our clientele are working professionals who tend to be a little bit more active. Any health situation that they have, they usually have taken advantage of their insurance and had it checkin’ out, so they bring it to our attention gladly.
Nonetheless, there were many alternate views expressed.
HYGIENIST: I think it’s very important. The patients don’t see their doctors usually, so since they see us more we would make a change for ‘em.
Further, the key informants reported that their patients were generally responsive to being offered referrals by them to primary care providers, especially the dentists.
DENTIST: If there’s a problem and I see that there might be something that I don’t feel comfortable with or that the patient should be address, either somehow they’re not feeling good and for some reason that day it seems like it may be an issue and we took their blood pressure and we tell them they better go to see somebody today, yeah, we go ahead and usually have pretty good compliance. Oh, I didn’t know that doc, thank you very much. Let me go ahead and see somebody in the next week or so or that day. Yeah, generally, I don’t get hassled. Once in a while in the past, I don’t know, people might follow-up, not follow-up, but in general, people take our advice. Yeah, yeah.
Other main findings were that the dental providers interviewed do not always encourage testing for patients who have not been screened for diabetes or hypertension, and infrequently see oral disease that they believe is related to diabetes or hypertension.
HYGIENIST: Well, I mean I don’t have a lot of patients who have diabetes that I know of, but those who have it, it’s very relevant. They definitely have oral conditions related to their diabetes.
Even when dental providers examine patients with blood pressures in the hypertensive range, they only counsel them insofar as referring them to see their primary care physicians. All of the dental providers interviewed failed to cite evidence-based guidelines in deciding what blood pressure reading is too high to perform dental treatment.
DENTIST: Yeah. Yes. Yes, there is, and I—but I must admit that I don’t routinely screen for high blood pressure either. I would say I’d be very—I’d be concerned about anything systolic of 160 and above.
Screening and Treatment for Tobacco Use
Most of the participating dental providers believe that it is important for their dental colleagues to screen and treat for tobacco use.
DENTIST: I think it’s, again, if it’s any practice, group practice, and I guess we’re out there as practitioners, healers, in society, we should continue to spread the word and educate the population that smoking is not good for you and do our best to try to cut it down amongst our whole population in the office that we see.
Nonetheless, alternate views were expressed, including a sense of fatalism around reimbursement.
HYGIENIST: ‘Cause it seems to be something that has to happen outside of the office, and which [sighs]—there’s no monetary benefit.
Relevance of Diet and Use of Technology
Most of the participating dental providers often see dental disease that they believe is related to poor diet, especially among younger patients.
DENTIST: Often. In the college age student, they go off with perfect teeth and come back with all sorts of trouble from late nights with a bottle of Coke and M&M's.
Importantly, the overwhelming majority of participants use their smart phones or other devices at chairside to obtain clinical information related to the care of their patients.
HYGIENIST: WebMD. WebMD and PubMed…But honestly, I use a search engine, and then I go to like a couple different ones to get what I'm looking for.
Findings Relative to the CFIR
The present study focused primarily on the views of dental providers (individuals involved) around primary care coordination at chairside (the intervention), but it also touched on other domains of the CFIR. For instance, dental providers were directly queried about incentives to follow professional guidelines, part of the domain known as the outer setting that includes the construct, external policies and incentives.23,24 While two dental hygienists mentioned receiving incentives for selling certain dental devices or procedures, none of the participants mentioned receiving incentives to follow professional guidelines.
HYGIENIST: [Laughs] Can you repeat that? There aren’t incentives. It’s all patient care oriented. My incentive is that my office is very patient care oriented so I don’t have to worry about anything else. I know about what’s best for the patient, the patient’s gonna get, whether or not they can afford it.
DENTIST: Incentives? Incentives is they keep their job [laughs]. Everybody’s got ethical standards…We don’t. No. But we do promote wellness as a general holistic rule. But there isn’t any specific financial compensation to the hygienist. I’m not averse to that idea, and we’ve talked about offering different products, including oral cancer screening, which I will often do myself. Right now, the oral cancer screening is usually done by the doctor, and I wouldn’t say the hygienists are involved with that. Or some of the other tests.
In addition, there were many office-related challenges that were identified to conducting primary care activities in dental offices, especially by the dental hygienists, which fall under the domain of the inner setting.
HYGIENIST: Time is always a challenge in a hygiene appointment. It seems, especially since I’m being taped, this is my thing, that they keep adding more responsibilities in the hygiene department and less time and salary. ‘Cause there’s a lot that we do because we are the first line of dental health care professional. There’s a lot that the doctor expects us to do before the patient gets in his chair, but our focus and specialty is cleaning teeth.
But what came across memorably in the interviews is that dental hygienists possessed values oriented toward patient-centered care, including but not limited to oral health care.
HYGIENISTS: In my years of hygiene, my patients appreciate the fact that I seem to care. That’s what I was taught in hygiene school: that we were the carers or the caregivers. They like when I seem concerned about how they feel, and how their health, and want to talk to them more about taking care of themselves, and not just their teeth.
DISCUSSION
One of the important take-home messages from this formative study is that there are multiple and significant missed opportunities at dental offices to screen, manage, and refer patients that might benefit from primary care treatment and/or tobacco use and nutrition counseling. The CFIR (see Figure 1) provides a pragmatic structure for approaching the complex, multi-level, and dynamic processes necessary for successfully implementing and adapting primary care coordination at chairside in dental offices, toward improving patient care outcomes.23
Another major finding is that dental hygienists are not being supported to provide patient care at the level of their full scope of practice. Self-identified challenges that prohibit dental hygienists from providing their patients with the highest quality standard of care (including screening, monitoring, and care coordination of diabetes and hypertension) include resource constraints, lack of confidence in their knowledge or training, problems with patient compliance and truthfulness, lack of institutional or systems-level support, and perception of these activities as falling within the domains of other health professionals.
Finally, it is noteworthy that all of the participating dental hygienists and dentists reported using electronic devices at chairside to obtain web-based health information in caring for their patients. The use of clinical decision support at chairside is a well-documented approach to increasing provider adherence to guideline-recommended screening, treatment, and referral, and may be easily integrated into an electronic dental record.33 Unfortunately, their effectiveness in improving patient morbidity across clinical settings is only modest, at best.34
Still, the dental profession is embarking on a new era with regard to electronic health records (EHRs).35 The New York University College of Dentistry recently instituted EHRs in its dental clinics. It is expected that both dental hygienists and dentists will gain confidence in expanding their scopes of practice to include primary care screening and referral in this setting, and that dissemination of these activities to dental offices will be abetted by this development.
Limitations of this formative study include the targeted recruitment strategy, which was supported by local professional contacts within the social networks of the involved study personnel. Thus, the participants were not necessarily representative of dental professionals in the New York City area overall. For instance, the dentists interviewed had all been practicing for a minimum of 28 years. Further, this pilot research prioritized in-depth qualitative data over a larger sample size, thus limiting the scope of perspectives, experiences, and demographics represented. Finally, the findings presented here represent a narrower account of the key informants’ perspectives and experiences that were present in the full data corpus. Nonetheless, the study findings selected for dissemination here may constitute a basis for future systematic research.
In summary, these findings suggest that increasing the role of dental hygienists in primary care coordination at chairside and incorporating evidence-based dentistry into patient care at dental offices will require the commitment of a wide range of individuals in both the inner setting of the involved dental practices and the outer setting of the primary care practices with which they partner (see Figure 1). By leveraging the existing workforce that already plays a central role in offering preventive services, patient education, and care coordination, dental hygienists may yet play an even more significant role in improving the health and well-being of their patients and the public at large.
CONCLUSION
Dental hygienists occupy a unique and vital role in providing trusted patient-centered dental care and are well positioned to help facilitate the greater integration of oral and general health care coordination. A theory-driven approach to implementing primary care coordination at chairside holds promise for successfully adapting evidence-based technological interventions to dental offices. Building upon these findings, a web-based clinical decision support system (CDSS) was developed.36 We are seeking funding to evaluate the developed CDSS with the active engagement of dental hygienists and dentists. This implementation research agenda seeks to support dental hygienists in primary care coordination at chairside, with the ultimate goal of improving patient outcomes.
Acknowledgments
FUNDING SOURCES:
The authors were supported in the research, analysis, and writing of this paper by the National Center for Advancing Translational Sciences of the US National Institutes of Health for the project titled, Primary Care Screening by Dental Hygienists at Chairside: Developing and Evaluating an Electronic Tool (grant UL1TR000038) and by the National Institute for Dental and Craniofacial Research and the Office of Behavioral and Social Sciences Research of the US National Institutes of Health for the project titled, Integrating Social and Systems Science Approaches to Promote Oral Health Equity (grant R01-DE023072).
The authors are grateful to the participants in this study who were forthcoming about their roles and challenges, and members of the senior advisory board who gave of their expertise and research materials toward advancing patient-centered care at chairside.
This study supports the NDHRA priority area, Health Services Research: Evaluate strategies that position and gain recognition of dental hygienists as primary care providers in the health care delivery system.
Footnotes
Disclaimers/Disclosures: The authors have no known conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
This study received institutional review board approval from the New York University School of Medicine.
Contributor Information
Mary E. Northridge, Department of Epidemiology & Health Promotion, New York University College of Dentistry.
Shirley Birenz, Dental Hygiene Program and Department of Epidemiology & Health Promotion, New York University College of Dentistry.
Danni Gomes, Dental Hygiene Program, New York University College of Dentistry.
Cynthia A. Golembeski, Department of Epidemiology & Health Promotion, New York University College of Dentistry.
Ariel Port Greenblatt, Department of Epidemiology & Health Promotion, New York University College of Dentistry.
Donna Shelley, Department of Population Health, New York University School of Medicine.
Stefanie L. Russell, Department of Epidemiology & Health Promotion, New York University College of Dentistry.
REFERENCES
- 1.Flieger SP, Doonan MT. Issue Brief. Putting the Mouth Back in the Body: Improving Oral Health Across the Commonwealth. Waltham, MA: Massachusetts Health Policy Forum; 2009. [Accessed May 4, 2015]. Available at: http://masshealthpolicyforum.brandeis.edu/ [PubMed] [Google Scholar]
- 2.Sparer M. Health reform and the future of dentistry. Am J Public Health. 2011;101(10):1841–1844. doi: 10.2105/AJPH.2011.300358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glick M. A home away from home: the patient-centered health home. J Am Dent Assoc. 2009;140(2):140–142. doi: 10.14219/jada.archive.2009.0110. [DOI] [PubMed] [Google Scholar]
- 4.Lamster IB, Eaves K. A model for dental practice in the 21st century. Am J Public Health. 2011;101(10):1825–1830. doi: 10.2105/AJPH.2011.300234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Northridge ME, Glick M, Metcalf SS, Shelley D. Public health support for the health home model. Am J Public Health. 2011;101(10):1818–1820. doi: 10.2105/AJPH.2011.300309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Improving access to oral health care for vulnerable and underserved populations. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 7.Mealey BL, Rose LF. Diabetes mellitus and inflammatory periodontal diseases. Curr Opin Endocrinol Diabetes Obes. 2008;15(2):135–141. doi: 10.1097/MED.0b013e3282f824b7. [DOI] [PubMed] [Google Scholar]
- 8.US Department of Labor. Bureau of Labor Statistics. Occupational Employment and Wages; 2014. May, [Accessed May 4, 2015]. Available at: http://www.bls.gov/oes/ [Google Scholar]
- 9.Center for Health Workforce Studies. A profile of active dental hygienists in New York. Rensselaer, NY: University at Albany School of Public Health; 2011. Jun, [Accessed May 4, 2015]. Available at: http://www.health.ny.gov/health_care/medicaid/redesign/docs/profile_active_dental_hygienists_in_ny.pdf. [Google Scholar]
- 10.Patient Protection and Affordable Care Act. Pub. L. No. 111–148. 2010 [Google Scholar]
- 11.Amemori M, Virtanen J, Korhonen T, Kinnunen TH, Murtomaa H. Impact of educational intervention on implementation of tobacco counseling among oral health professionals: a cluster-rendomized community trial. Community Dent Oral Epidemiol. 2013;41(2):120–129. doi: 10.1111/j.1600-0528.2012.00743.x. [DOI] [PubMed] [Google Scholar]
- 12.Bell KP, Phillips C, Paquette DW, Offenbacher S, Wilder RS. Incorporating oral-systemic evidence into patient care: practice behaviors and barriers of North Carolina dental hygienists. J Dent Hyg. 2011;85(2):99–113. [PubMed] [Google Scholar]
- 13.Bell KP, Phillips C, Paquette DW, Offenbacher S, Wilder RS. Dental hygienists’ knowledge and opinions of oral-systemic connections: implications for education. J Dent Educ. 2012;76(6):682–694. [PubMed] [Google Scholar]
- 14.Boyd LD, Hartman-Cunningham ML. Survey of diabetes knowledge and practices of dental hygienists. J Dent Hyg. 2008;82(5):43. [PubMed] [Google Scholar]
- 15.Efurd MG, Bray KK, Mitchell TV, Williams K. Comparing the risk identification and management behaviors between oral health providers for patients with diabetes. J Dent Hyg. 2012;86(2):130–140. [PubMed] [Google Scholar]
- 16.Hughes CT, Thompson AL, Browning WD. Blood pressure screening practices of a group of dental hygienists: a pilot study. J Dent Hyg. 2004;78(4):11. [PubMed] [Google Scholar]
- 17.Strauss SM, Singh G, Tuthill J, Brodsky A, Rosedale M, Bytyci A, Drayluk I, Llambini A, Savice K, Russell SL. Periodontal patients' knowledge about diabetes: the importance of dental hygienists' support. J Dent Hyg. 2013;87(2):82–99. [PMC free article] [PubMed] [Google Scholar]
- 18.Swanson Jaecks KM. Current perceptions of the role of dental hygienists in interdisciplinary collaboration. J Dent Hyg. 2009;83(2):84–91. [PubMed] [Google Scholar]
- 19.Millery M, Shelley D, Wu D, Ferrari P, Tseng TY, Kopal H. Qualitative evaluation to explain success of multifaceted technology-driven hypertension intervention. Am J Manag Care. 2011;17(12 Spec No):SP95–SP102. [PubMed] [Google Scholar]
- 20.Shelley D, Tseng TY, Matthews AG, Wu D, Ferrari P, Cohen A, Millery M, Ogedegbe O, Farrell L, Kopal H. Technology-driven intervention to improve hypertension outcomes in community health centers. Am J Manag Care. 2011;17(12 Spec No):SP103–SP110. [PubMed] [Google Scholar]
- 21.Strauss SM, Alfano MC, Shelley D, Fulmer T. Identifying unaddressed systemic health conditions at dental visits: patients who visited dental practices but not general health care providers in 2008. Am J Public Health. 2012;102(2):253–255. doi: 10.2105/AJPH.2011.300420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilder RS. Promotion of oral health: need for interprofessional collaboration. J Dent Hyg. 2008;82(2):13. 2008. [PubMed] [Google Scholar]
- 23.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.CFIR Research Team. CFIR Technical Assistance Website. Ann Arbor, MI: Center for Clinical Management Research; [Accessed September 11, 2015]. Available at: http://cfirguide.org/index.html. [Google Scholar]
- 25.Polit D-F, Beck C-T. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 8th. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008. [Google Scholar]
- 26.Glaser BG, Strauss A. The Discovery of Grounded Theory. Strategies for Qualitative Research. Chicago, IL: Aldline; 1967. [Google Scholar]
- 27.Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. California: Sage Publications; 1990. [Google Scholar]
- 28.Strauss A, Corbin J. Basic of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 2nd. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 29.Charmaz K. Grounded Theory: objectivist and constructivist methods. In: Denzin NK, Lincoln YS, editors. Handbook of Qualitative Research. 2nd. Thousand Oaks, CA: Sage Publications; 2000. pp. 509–536. [Google Scholar]
- 30.Charmaz K. Constructing Grounded Theory. A Practical Guide through Qualitative Analysis. London: Sage Publications; 2006. [Google Scholar]
- 31.ATLAS.ti, version 7. Qualitative Data Analysis. Berlin, Germany: ATLAS.ti Scientific Software Development GmbH; 2014. [Google Scholar]
- 32.Corbin J, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3–21. [Google Scholar]
- 33.Forrest JL, Miller SA, Miller G. Keeping current: clinical decision support systems. J Dent Hyg. 2012;86(1):18–20. [PubMed] [Google Scholar]
- 34.Moja L, Kwag KH, Lytras T, Bertizzolo L, Brandt L, Pecoraro V, Rigon G, Vaona A, Ruggiero F, Mangia M, Iorio A, Kunnamo I, Bonovas S. Effectiveness of computerized decision support systems linked to electronic health records. Am J Public Health. 2014;104(12):e12–e22. doi: 10.2105/AJPH.2014.302164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalenderian E, Walji M, Ramoni RB. “Meaningful use” of HER in dental school clinics: how to benefit from the U.S. HITECH Act’s financial and quality improvement incentives. J Dent Educ. 2013;77(4):401–415. [PubMed] [Google Scholar]
- 36.Russell SL, Greenblatt AP, Gomes D, Birenz S, Golembeski CA, Shelley D, McGuirk M, Eisenberg E, Northridge ME. Toward implementing primary care at chairside: developing a clinical decision support system for dental hygienists. J Evid Based Dent Pract. doi: 10.1016/j.jebdp.2015.08.003. (in press) Note: Drs. Russell and Greenblatt share first co-authorship. [DOI] [PMC free article] [PubMed] [Google Scholar]


