Abstract
Hemophagocytosis shows engulfment of hematopoietic cells by histiocytes and is a property generally associated with cells of the histiocytic lineage. It can be familial or is seen in a wide spectrum of acquired disorders. Hemophagocytosis by leukemic blasts is an uncommon phenomenon and has been reported mainly in acute myeloid leukemia. Its association with acute lymphoblastic leukemia is rare. We present a case of hemophagocytosis by blasts in the bone marrow in a 11 year old boy with T cell-acute lymphoblastic leukemia.
Keywords: Blasts, Hemophagocytosis, T-ALL
Introduction
Hemophagocytic syndrome is a disorder of the mononuclear phagocytic system, characterized by benign, generalized histiocytic proliferation with marked hemophagocytosis in the bone marrow. There is engulfment of hematopoietic cells by activated macrophages acting outside of usual immune system regulations. Hemophagocytosis can be familial or acquired. Common acquired causes associated with this syndrome are infections, autoimmune disorders, malignancies and metabolic disorders. In most cases, the histiocytes engulf hematopoietic cells [1]. However, hemophagocytosis by leukemic blasts is an uncommon phenomenon and has been reported in patients with acute myeloid leukemia (AML) especially acute megakaryoblastic leukemia [2]. Its occurrence in lymphoblastic leukemic blasts is rare [3].
We present a patient with T cell acute lymphoblastic leukemia (ALL) with hemophagocytosis by blasts in the bone marrow.
Case History
An 11 years old boy presented with multiple nodular swellings in the neck and fatigue since 1 month. He had no history of fever or bleeding from any site. On examination, he had mild pallor with bilateral cervical, axillary and inguinal lymphadenopathy. There was no icterus. Liver was palpable 5 cm below the right costal margin and spleen, 4 cm below the left costal margin.
Investigations showed hemoglobin of 7.3 gm/dL, total leucocyte count—1,24,000/cu mm and platelet count—24,000/cu mm. Differential leucocyte count on peripheral blood showed blasts—90 %, metamyelocytes—02 %, neutrophils—01 %, lymphocytes—07 % and 3 erythroblasts per 100 WBC. The blasts were of size 14–20 microns with high nucleo-cytoplasmic ratio, immature chromatin, regular nuclear margin and 1–2 conspicuous nucleoli. The cytoplasm was scanty with no granules or Auer rods. No hemophagocytosis was seen in the peripheral smear.
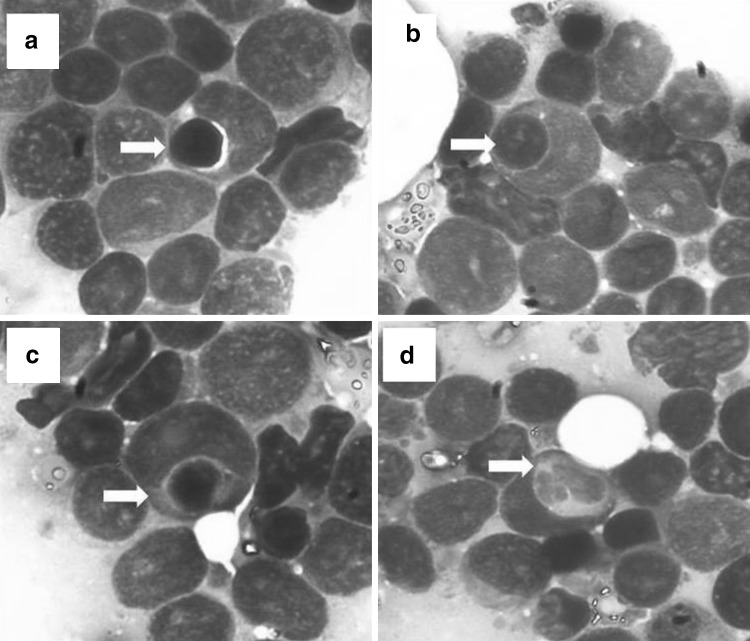
Bone marrow aspirate showed hypercellular marrow with blasts—88 %, lymphocytes—3 % and nucleated red blood cells—9 %. All three hemopoietic lineages were depressed. The morphology of blasts was similar to that seen in the peripheral blood smear, except that prominent hemophagocytosis (1 in 5 oil immersion fields) was seen. The blasts were seen to engulf mainly erythroblasts (Fig. 1a, b, c). Rare blasts showed neutrophilic phagocytosis (Fig. 1d).
Fig. 1.
Bone marrow aspirate smears showing engulfment of erythroblasts by T-lymphoblasts (a, b, c). Note the larger blasts with immature chromatin, conspicuous nucleoli engulfing the much smaller erythroblasts with clumped chromatin. Rare blasts also showed neutrophilic phagocytosis (d)
Myeloperoxidase and periodic acid Schiff stains were negative. Immunophenotyping by flow cytometry showed strong positivity for CD34 (95.4 %) and CD45 (96.0 %) along with positivity for T cell markers, CD7 (94.5 %) and CD3 (54.1 %). CD5 (22.5 %) was weakly positive. Monocytic marker, CD14 was negative (4.8 %). Aberrant positivity for myeloid marker, CD33 (87.9 %) was also seen. Cytogenetic study was not done.
Biochemical investigations showed blood urea—29 mg/dL, serum creatinine—0.4 mg/dL, hyponatremia (Na—123 meq/L) and hypokalemia (K—2.2 meq/L). Lactate dehydrogenase levels were raised—4990 U/L. Ferritin and triglyceride levels were not done. Chest X-ray showed right sided mediastinal mass. A diagnosis of T cell ALL with aberrant expression of CD33 and hemophagocytosis by blasts was made.
The patient was initiated on BFM ALL protocol. However, he had underlying infection with mucormycosis of the neck at the site of lymph node biopsy done from elsewhere which progressed in-spite of antifungal therapy and he subsequently succumbed to systemic bacterial infection.
Discussion
Hemophagocytic lymphohistiocytosis (hemophagocytic syndrome) is a condition of immune dysregulation characterized by severe organ damage induced by a hyperinflammatory response and uncontrolled T cell and macrophage activation. It has been traditionally divided into a primary/genetic form, which typically manifests in children with genetic abnormalities of the cytotoxic function of NK cells and T cells, and a secondary/acquired form that tends to occur at older ages in the setting of associated infections, autoimmune/rheumatologic, malignant, or metabolic conditions, without an identifiable genetic abnormality [1]. Two histiocytes demonstrating phagocytosis of erythrocytes, lymphocytes, neutrophils, platelets or nuclear debris should be present in each slide for certainty of diagnosis. The phagocytosis is associated with proliferation of benign histiocytes [3].
Hemophagocytosis by leukemic blasts is an uncommon phenomenon and has been described in AML [2, 4, 5], ALL [6, 7], chronic myelogenous leukemia (CML) in blast crisis [8] and myelodysplastic syndrome (MDS) [9].
Imashuku et al. in their study on 7 cases hypothesized that hemophagocytosis by leukemic blasts is a common and characteristic morphological finding in AML with specific chromosome aberration of t(16;21)(p11;q22). All patients in their study had a relatively young age and poor prognosis [4]. In another study of 5 cases of AML showing hemophagocytosis by myeloid blasts, t(16;21)(p11;q22) was found. Four of these patients had acute megakaryoblastic leukemia [2].
The specificity of hemophagocytosis by leukemic blasts has been controversial and the exact pathogenesis of this phenomenon is not known. However, Shikami et al. in their study on cellular characteristics in AML with t(16;21)(p11;q22) have reported that AML blasts with t(16;21) continue to express a number of stem cell markers such as CD34 and c-kit which permit differentiation into monocytic lineage and hence enabling the cells to have phagocytic activity [10]. Morphologically, hemophagocytic blasts with t(16;21) show single or multiple cytoplasmic vacuoles some of which are filled with homodense, creamy material. In addition, honeycomb like vacuoles with phagosomes have also been reported [4]. Two other cases of AML with complex cytogenetic abnormality showing hemophagocytosis have been described by Coulthard et al. These patients had inv(8)(p11q13) [5].
Hemophagocytosis by lymphoid blasts is rare and very few cases have been reported [3]. Foadi et al. noted hemophagocytosis by lymphoblasts in four patients with ALL relapse. They attributed the unusually aggressive behavior of the disease in these patients to the emergence of cells with phagocytic properties [6]. Lymphoblasts showing hemophagocytosis has also been reported in a 3 years old boy with B lymphoblastic leukemia with t(12;21)(p13;q22); TEL-AML1 (ETV6-RUNX1) [7].
Patients in whom hemophagocytosis by myeloid blasts has been reported showed complex cytogenetic abnormalities [2, 4, 5,], poor response to therapy [5] and poor prognosis [8]. No reports of hemophagocytosis by T lymphoblasts were found on a detailed literature search. However, Histiocytosis/HLH has been reported in patients with T-ALL [11–13] although the leukemic blasts showed no engulfment of hematopoietic cells.
Since hemophagocytosis is mainly associated with myeloblasts, its association with lymphoid blasts in our patient could be explained by the aberrant myeloid expression found on immunophenotyping.
Conclusion
Hemophagocytosis by leukemic blasts is a rare phenomenon mostly associated with myeloid blasts. Its association with T cell ALL is extremely rare and could possibly have implications in adversely affecting prognosis.
Acknowledgments
Conflicts of Interest
None.
References
- 1.Rosado FG, Kim AS. Hemophagocytic lymphohistiocytosis. An update on diagnosis and pathogenesis. Am J Clin Pathol. 2013;139:713–727. doi: 10.1309/AJCP4ZDKJ4ICOUAT. [DOI] [PubMed] [Google Scholar]
- 2.Imashuku S, Hibi S, Kuriyama K, Todo S. Hemophagocytosis by leukemic blasts in a case of acute megakaryoblastic leukemia with t(16;21)(p11;q22) Int J Hematol. 1999;70:36–39. [PubMed] [Google Scholar]
- 3.Gupta A, Modi CJ, Gujral S. Hemophagocytosis by leukemic cells in biphenotypic acute leukemia: a rare case. Indian J Pathol Microbiol. 2010;53:370–371. doi: 10.4103/0377-4929.64282. [DOI] [PubMed] [Google Scholar]
- 4.Imashuku S, Hibi S, Sako M, et al. Hemophagocytosis by leukemic blasts in 7 acute myeloid leukemia cases with t(16;21)(p11;q22): common morphologic characteristics for this type of leukemia. Cancer. 2000;88:1970–1975. doi: 10.1002/(SICI)1097-0142(20000415)88:8<1970::AID-CNCR28>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 5.Coulthard S, Chase A, Orchard K, et al. Two cases of inv(8)(p11q13) in AML with erythrophagocytosis: a new cytogenetic variant. Br J Haematol. 1998;100:561–563. doi: 10.1046/j.1365-2141.1998.00587.x. [DOI] [PubMed] [Google Scholar]
- 6.Foadi MD, Slater AM, Pegrum GD. Erythrophagocytosis by acute lymphoblastic leukaemic cells. Scand J Haematol. 1978;20:85–88. doi: 10.1111/j.1600-0609.1978.tb01558.x. [DOI] [PubMed] [Google Scholar]
- 7.Park JE, Park IJ, Lim YA, Lee WG, Cho SR. Hemophagocytosis by leukemic blasts in B lymphoblastic leukemia with t(12;21)(p13;q22); TEL-AML1 (ETV6-RUNX1): a case report. Ann Clin Lab Sci. 2013;43:186–189. [PubMed] [Google Scholar]
- 8.Shanley JD, Cline MJ. Phagocytosis of hematopoietic cells by blast cells in blast crisis of chronic myelocytic leukemia. West J Med. 1977;126:139–141. [PMC free article] [PubMed] [Google Scholar]
- 9.Kuyama J, Fushino M, Take H, Kanayama Y. Myelodysplastic syndrome associated with erythrophagocytosis by blasts and myeloid cells. Int J Hematol. 1995;62:243–246. doi: 10.1016/0925-5710(95)00409-2. [DOI] [PubMed] [Google Scholar]
- 10.Shikami M, Miwa H, Nishii K, et al. Myeloid differentiation antigen and cytokine receptor expression on acute myelocytic leukemia cells with t(16;21)(p11;q22): frequent expression of CD56 and interleukin-2 receptor alpha chain. Br J Haematol. 1999;105:711–719. doi: 10.1046/j.1365-2141.1999.01384.x. [DOI] [PubMed] [Google Scholar]
- 11.Irfan A, Sahin F, Kaptan K, Safal M, Beyan C. A case of adult acute T-cell lymphoblastic leukemia presented with hemophagocytic syndrome. Turk J Hematol. 2008;25:155–156. [PubMed] [Google Scholar]
- 12.Trebo MM, Attarbaschi A, Mann G, Minkov M, Kornmüller R, Gadner H. Histiocytosis following T-acute lymphoblastic leukemia: a BFM study. Leuk Lymphoma. 2005;46:1735–1741. doi: 10.1080/10428190500160017. [DOI] [PubMed] [Google Scholar]
- 13.Moritake H, Kamimura S, Nunoi H, et al. Clinical characteristics and genetic analysis of childhood acute lymphoblastic leukemia with hemophagocytic lymphohistiocytosis: a Japanese retrospective study by the Kyushu-Yamaguchi Children’s Cancer Study Group. Int J Hematol. 2014;100:70–78. doi: 10.1007/s12185-014-1591-1. [DOI] [PubMed] [Google Scholar]