Abstract
Purpose
Primary intraocular lymphoma (PIOL) is a rare malignancy with an aggressive clinical course. It is usually considered as a subset of primary central nervous system lymphoma. Differential diagnosis should include infectious and non-infectious aetiologies, particularly the common masqueraders sarcoidosis, tuberculosis, viral retinitis and syphilis.
Patient
The article presents a case of bilateral vitreoretinal lymphoma manifesting as uveitis and vitritis resistant to corticosteroid therapy. The final diagnosis was based on a retinal biopsy.
Results
The patient was successfully treated with systemic and local therapy. Long-term complete remission (CR) was reached. The relapse of diffuse large B-cell lymphoma was revealed in the frontal left lobe after 48 months of CR duration.
Conclusion
The diagnosis of PIOL is always very difficult. Cooperation of pathologists, ophthalmologists and hematologists is required for a quick and accurate diagnosis. Local and systemic treatment is needed to achieve CR, but the relapse rate remains very high.
Keywords: Lymphoma, Vitritis, Retinal infiltration, Uveitis, Chemotherapy
Introduction
Primary intraocular lymphoma (PIOL) is a rare malignancy with an aggressive clinical course. It is usually considered as a subset of primary central nervous system lymphoma (PCNSL) [1]. The vast majority of PIOL cases are diffuse large B-cell lymphoma (DLBCL). Less common histologies include T-cell PCNSL, Burkitt, lymphoblastic and marginal zone lymphomas [1]. Nearly 20 % of PCNSL cases present with intraocular involvement with cellular infiltrates in the vitreous and retina. Diagnosis is always a challenge, as the disease can mimic steroid-resistant ocular inflammation [2]. Here we present a case of retinochoroidal primary DLBCL of both eyes, successfully diagnosed by a retinal biopsy and treated with systemic and intravitreal chemotherapy.
Case Presentation
A 59-year-old, European woman with a 15-year history of pulmonary tuberculosis initially had presented a decrease of visual acuity (VA) in the left eye, which had slowly progressed since July 2008. The patient was admitted to the Department of Ophthalmology in Wroclaw Medical University in December 2008 with a significant decrease of vision in this eye. Her VA was 1.0 cc + 1.25 Dsph in the right eye and counting fingers from 10 cm in the left eye. Anterior segment was within normal limits in both eyes. The posterior segment was normal in the right eye, and vitritis in the left eye was noticed with a poor view of the optic nerve and macula. In the fluorescent angiography the right eye was within normal limits, and the left eye was difficult to evaluate because of the vitreous cells. In January 2009, she was again admitted to the Department of Ophthalmology with the presence of deep infiltrations of the retina, mild vitritis and macular oedema in the left eye confirmed by fluorescent angiography. The right eye was normal (Fig. 1). She received prednisone 1 mg/kg mc and tuberculostatic treatment because she was RT 23 (Mantoux test) positive and had a history of pulmonary tuberculosis. Laboratory tests were within normal limits, HIV negative, anti-Toxoplasma and Borrelia negative, normal serology for Herpes simplex virus (HSV) and Cytomegalovirus (CMV). In March 2009, despite systemic steroid and anti-tuberculosis therapy, her condition continued to deteriorate, with the development of optic nerve oedema and progressive retinal infiltrates in both eyes (Fig. 2a, b). Finally, she was diagnosed with an ocular DLBCL based on a retinal biopsy. Staging procedures including a whole-body CT scan, cranial MRI and bone marrow biopsy did not reveal infiltration of DLBCL apart from the ocular localization. The patient was admitted to the Department of Hematology, Blood Neoplastic Disorders and Bone Marrow Transplantation of Wroclaw Medical University (Poland) in June 2009. She started systemic chemotherapy with methotrexate (MTX)–5.0 g intravenously (i.v.) every 3 weeks for 8 doses and intravitreal therapy of MTX–400.0 μg/0.1 ml for both eyes monthly. Moreover, intrathecal treatment was given: MTX 15 mg, cytarabine (Ara-C) 40 mg and dexamethasone 4 mg every 3 weeks for 11 times. Intravitreal MTX injections were repeated monthly for a total of 33 injections, resulting in complete regression of retinal infiltrations and functional recovery (Fig. 3, December 2009). The control MRI of the orbits and the brain was within normal limits. The response to treatment was monitored by hematologists and ophthalmologists every 3 months. That included systemic examination with regular MRIs and eye examination for local tumour control.
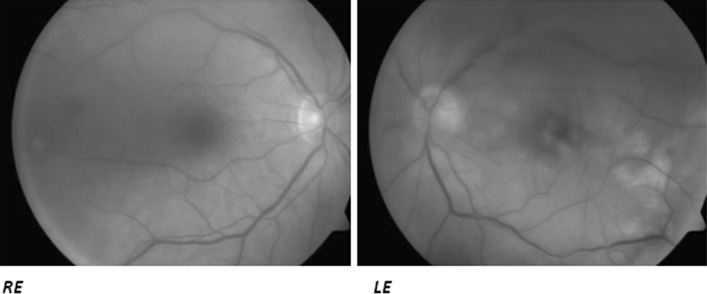
Fig. 1.
January 2009. Fundus photography: right eye (RE) normal fundus, left eye (LE) retinal deep infiltrations near lower temporal vascular arcade, macular oedema, vitritis
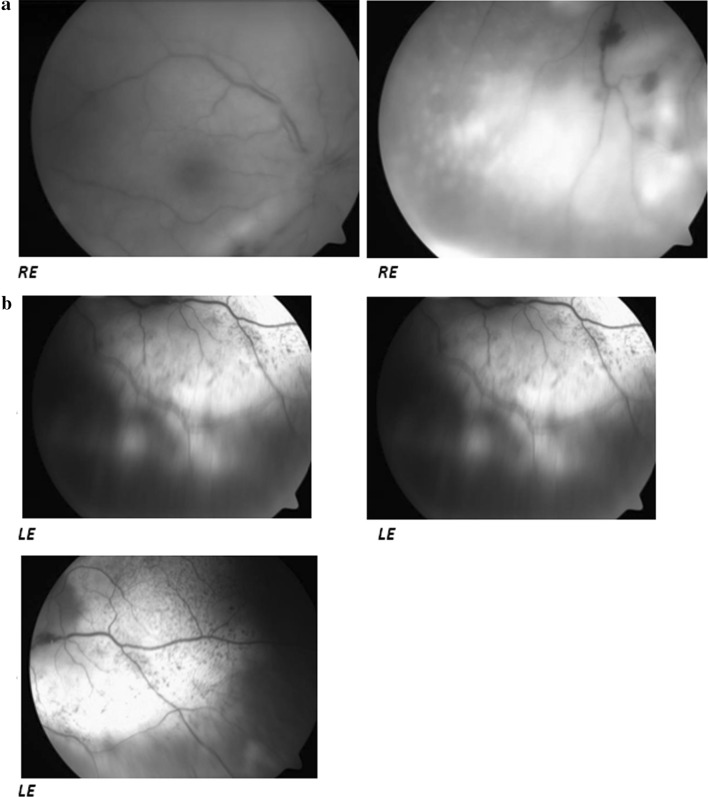
Fig. 2.
a March 2009. Fundus photography: right eye (RE): retinal infiltrations around lower temporal arcade, small retinal hemorrhages near vessels. b March 2009. Fundus photography: left eye (LE) after diagnostic vitrectomy with silicon oil tamponade, infiltration of the optic nerve head, with surrounding hemorrhages, typical white deep retinal changes with patchy pigmentation
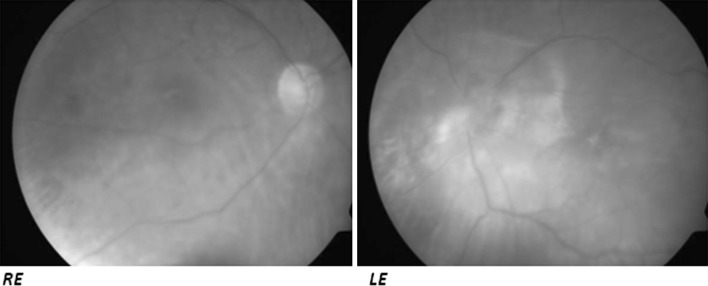
Fig. 3.
December 2009. Fundus photography after chemotherapy: normal posterior pole of the right eye (RE), in the left eye (LE) fibrotic changes around the optic nerve head
In January 2014 the patient’s mental status had changed. Neurologic examination revealed loss of orientation, memory, verbal abilities and a right side hemiparesis. MRI of the brain indicated a tumour in the frontal left lobe that measured 20.2 × 22.1 mm with oedema of the brain tissue (Fig. 4). Stereotactic biopsy of the tumour confirmed DLBCL. The patient underwent chemotherapy consisting of high doses of Ara-C (6.4 g i.v.), MTX (6.4 i.v.) and dexamethasone, with no clinical or radiological response. Radiation therapy of CNS (50 Gy/wl) brought a temporary improvement, but the patient died 2 months after the DLBCL’s relapse was diagnosed.
Fig. 4.
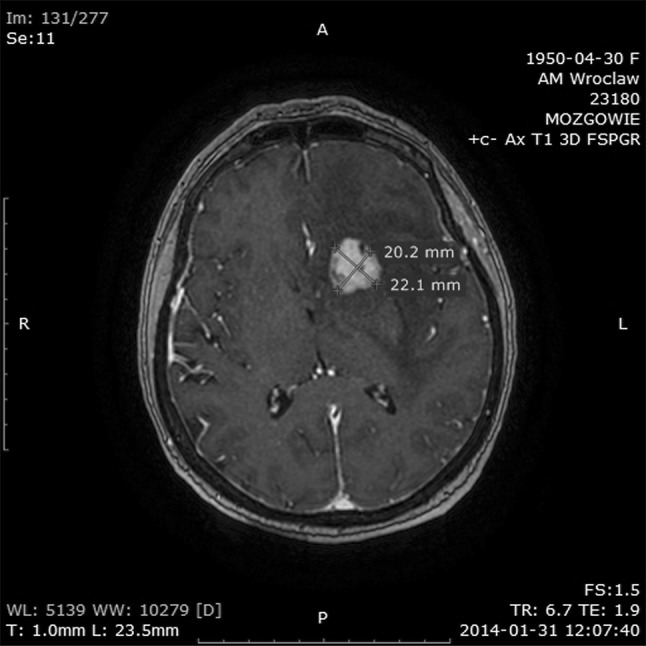
January 2014. Brain`s MRI: a tumour in the frontal left lobe with oedema of the brain tissue
Discussion
Diagnosis of PIOL can be challenging. It requires a high degree of clinical suspicion. Differential diagnosis should include infectious and non-infectious aetiologies, particularly the common masqueraders such as sarcoidosis, tuberculosis, viral retinitis and syphilis [2]. This rare disease should be suspected in all patients with uveitis resistant to corticosteroid therapy and in elderly patients with a recent onset of vitritis [3]. Patients typically complain of decreased vision, painless blurred vision and floaters, most likely secondary to the chronic vitritis and subretinal lesions. Some patients are asymptomatic and are diagnosed only when examined following diagnosis of PCNSL. PIOL is a subset of PCNSL and is usually an aggressive DLBCL. Central nervous system involvement will occur in 50–80 % of patients of PIOL after the onset of ocular symptoms. Conversely, 15–25 % of patients with PCNSL have ocular involvement. The most common ocular manifestations are posterior uveitis or vitritis. Characteristically, PIOL tends to be bilateral. The major risk factors for PIOL/PCNSL are immunodeficiency and immunosuppression [4]. Definitive diagnosis still requires harvesting of a sufficient amount of good quality tissue that is kept fresh for histopathological analysis [4]. The optimal treatment of PIOL includes high dose of systemic chemotherapy (MTX/Ara-C) with common complete remission, although relapse is frequent. Intravitreal MTX can be used successfully in some patients but disease relapse is common when therapy is discontinued. Orbital radiation can lead to remission, but there are many adverse events, such as dry eye, optic neuropathy and retinopathy, and it does not prolong survival. Rituximab given both systematically and intravitreally was used based on its efficacy, with a good initial response, but subsequent relapse required intravitreal MTX and radiation [5, 6]. PIOL is associated with a poor prognosis, with patients dying of CNS disease; therefore appropriate diagnosis is crucial for the treatment. In our patient the combination therapy—intravenous, intravitreal and intrathecal—led to long-term complete remission which continued for 49 months. Relapse was confirmed in CNS with no infiltration within the orbits, but resistance to chemotherapy and radiotherapy was observed. According to the other data, the relapse of PIOL is frequent in the brain, spinal cord and the meningeal localization, and despite high doses of chemotherapy the course is often fatal. Follow-up periods range from 12 to 35 months, with mortality rates up to 81 % [7]. The optimal approach includes either systemic or intraocular chemotherapy, which delays the relapse and may influence the overall survival.
Conclusion
The diagnosis of PIOL is highly difficult. Cooperation of pathologists, ophthalmologists and hematologists is required for a quick and accurate diagnosis. Local and systemic treatment is needed to achieve complete remission, but the relapse rate remains very high.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from the patient included in the study.
References
- 1.Faia LJ, Chan CC. Primary intraocular lymphoma. Arch Pathol Lab Med. 2009;133(8):1228–1232. doi: 10.5858/133.8.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jusufbegovic D, Kim V, Char DH. Primary uveal lymphoma with epibulbar extension masquerading as an intraocular inflammation. Can J Ophthalmol. 2015;50(1):e24–e26. doi: 10.1016/j.jcjo.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 3.Coupland SE, Bechrakis NE, Anastassiou G, Foerster AM, Heiligenhaus A, Pleyer U, Hummel M, Stein H. Evaluation of vitrectomy specimens and chorioretinal biopsies in the diagnosis of primary intraocular lymphoma in patients with masquerade syndrome. Graefes Arch Clin Exp Ophthalmol. 2003;241(10):860–870. doi: 10.1007/s00417-003-0749-y. [DOI] [PubMed] [Google Scholar]
- 4.Sagoo MS, Mehta H, Swampillai AJ, Cohen VM, Amin SZ, Plowman PN, Lightman S. Primary intraocular lymphoma. Surv Ophthalmol. 2014;59(5):503–516. doi: 10.1016/j.survophthal.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Itty S, Olson JH, O’Connell DJ, Pulido JS. Treatment of primary intraocular lymphoma (PIOL) has involved systemic, intravitreal or intrathecal chemotherapy and/or radiotherapy. Retina. 2009;29(3):415–416. doi: 10.1097/IAE.0b013e318196b1f6. [DOI] [PubMed] [Google Scholar]
- 6.Itty S, Pulido JS. Rituximab for intraocular lymphoma (2009). Retina 29(2):129-32. doi: 10.1097/IAE.0b013e318192f574. Review [DOI] [PubMed]
- 7.Chan CC, Rubenstein JL, Coupland SE, Davis JL, Harbour JW, Johnston PB, Cassoux N, Touitou V, Smith JR, Batchelor TT, Pulido JS. Primary vitreoretinal lymphoma: a report from an International Primary Central Nervous System Lymphoma Collaborative Group symposium. Oncologist. 2011;16(11):1589–1599. doi: 10.1634/theoncologist.2011-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]