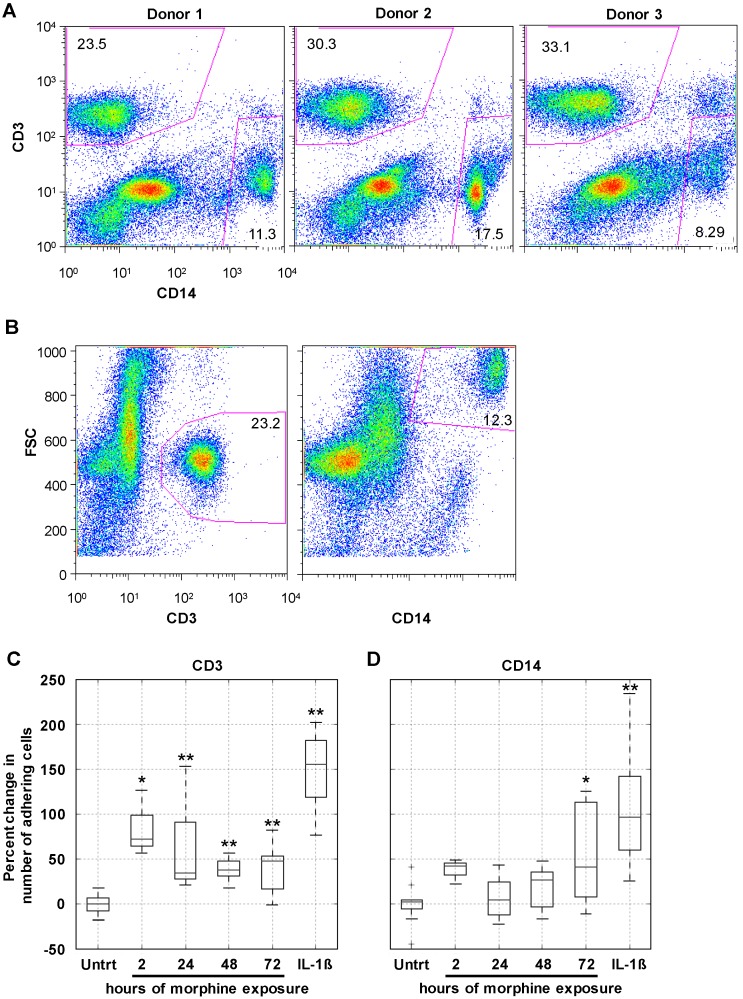
Figure 4.
Prolonged morphine exposure increased peripheral blood mononuclear cell (PBMC) firm adhesion. hCMEC/D3 cells were grown to confluence as described earlier. At confluence, cells were exposed continuously to morphine (0.1 µM) for 2, 24, 48, or 72 h with re-administration at 24 h intervals. The final morphine administration preceded the adhesion assay by 2 h. As a positive control of enhanced adhesion, confluent hCMEC/D3 cells were exposed to IL-1β (20 ng/mL) for 24 h. Following treatment, a suspension of 1 million PBMCs in co-culture media was added to the hCMEC/D3 monolayer and the co-cultures were incubated at 37 °C in 5% CO2 for 30 min to allow adhesion to occur. (A) At the start of each adhesion assay, the start population of PBMCs was stained for CD3 and CD14 and analyzed by flow cytometry. Each donor had comparable CD3+ and CD14+ viable cell populations, indicating that the representation of these cell types in the initial population was not the driving force behind any observed differences in selective cell adhesion; (B) population gates were established on forward scatter (FSC) and either CD3 or CD14, and the number of events within each of these gates was used in the analysis as the number of CD3+ and CD14+ PBMCs that adhered to the hCMEC/D3 monolayer. Representative scatter plots from Donor 1 are shown here; (C) morphine treatment for 2, 24, 48, and 72 h, as well as IL-1β treatment of the monolayer, increased the number of CD3+ cells firmly adhering to the hCMEC/D3 monolayer, as quantitated by CD3 staining and flow cytometric analysis; (D) morphine treatment of the monolayer significantly induce firm adhesion of CD14+ cells but only at the 72 h time point. Treatment of the monolayer with IL-1β is shown as a positive control for increased adhesion. All bars represent three independent experiments performed in triplicate, each with individual PBMC donor samples. * p ≤ 0.02; ** p ≤0.002 as determined by Student’s t-test.