Abstract
Populations are aging and the prevalence of diabetes mellitus is increasing tremendously. The number of older people with diabetes is increasing unexpectedly. Aging and diabetes are both risk factors for functional disability. Thus, increasing numbers of frail or disabled older patients with diabetes will increase both direct and indirect health-related costs. Diabetes has been reported as an important risk factor of developing physical disability in older adults. Older people with diabetes have lower muscle mass and weaker muscle strength. In addition, muscle quality is poorer in diabetic patients. Sarcopenia and frailty have a common soil and may share a similar pathway for multiple pathologic processes in older people. Sarcopenia is thought to be an intermediate step in the development of frailty in patients with diabetes. Thus, early detection of sarcopenia and frailty in older adults with diabetes should be routine clinical practice to prevent frailty or to intervene earlier in frail patients.
Keywords: Diabetes, Disability, Frailty, Sarcopenia
The Sulwon Award for Scientific Achievement is the Korean Diabetes Association's highest scientific award and honors an individual who has excellently contributed to the progress in the field of diabetes and metabolism. Sulwon Award is named after an emeritus professor Eung Jin Kim, who founded Korean Diabetes Association. Prof. Hak Chul Jang received the seventh Sulwon Award at 2015 International Conference on Diabetes and Metabolism, October 15-17, 2015 at Jejudo Island, Korea.
INTRODUCTION
Increased life expectancy and declining fertility has brought dramatic shifts in the age structure worldwide [1]. Large populations are aging and this has become a global social and health burden. A progressive decline in muscle mass and strength, termed sarcopenia, develops as a consequence of aging [2]. The prevalence of sarcopenia reported varies widely depending on the definition and methods of assessment; it ranges from 8% to 40% of people aged over 60 years [3,4]. Sarcopenia results in frailty, loss of independence, physical disability, and increased mortality in older adults [5,6].
Diabetes mellitus is a prevalent chronic disease, especially in older adults, that is associated with microvascular and cardiovascular complications [7]. More than 25% of Korean people over age 60 years have diabetes mellitus [8,9]. Diabetes has been associated with an increased risk of developing physical disability in older adults [10,11]. Chronic conditions such as visual disturbances, diabetic complications, comorbidities, and depression are associated with physical disability in patients with diabetes; however, these account for only some of the impairments [12]. It was also reported that men and women with diabetes diagnosed at age 60 have estimated reductions in life expectancy of 7.3 and 9.5 years and good quality of life of 11.1 and 13.8 years, respectively [13]
Physical and cognitive function becomes of great importance in the care of older people with diabetes. A key strategy is to prevent the functional decline instead of attempting to recover lost function. In this review, the relationship between sarcopenia, frailty, and physical disability in older adults with diabetes will be discussed.
SARCOPENIA AND DIABETES
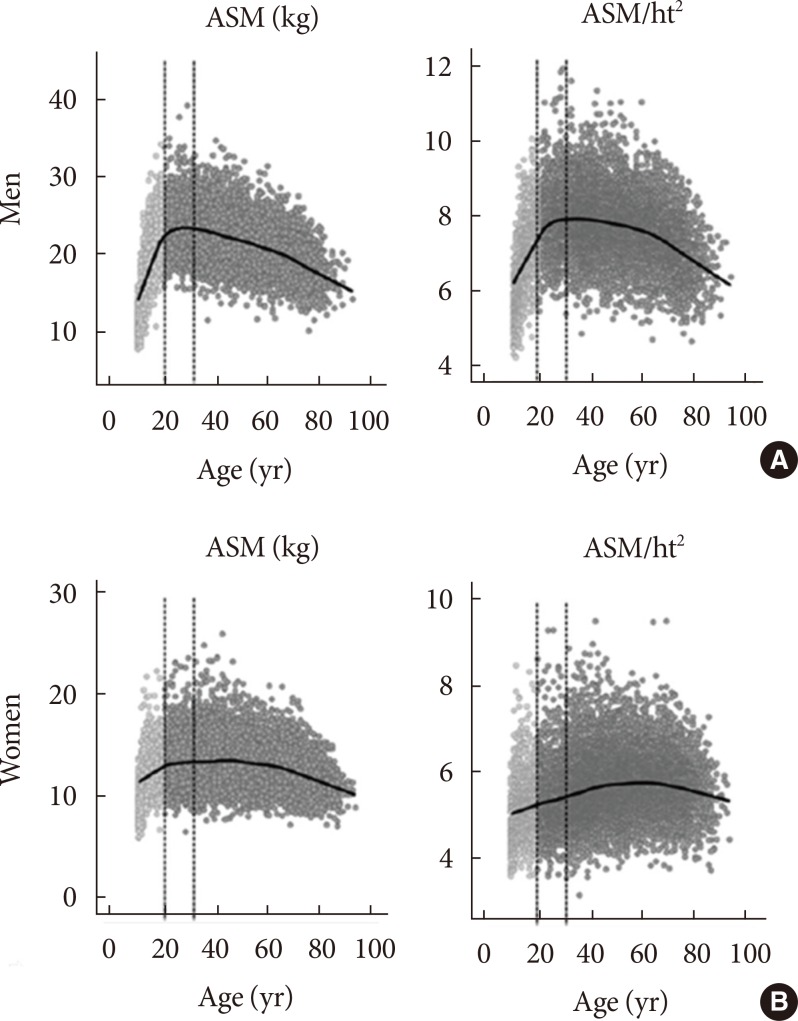
A progressive decrease in muscle mass, especially of the lower extremities and an increase in fat mass, especially of visceral and intermuscular fat are common body compositional changes associated with aging [14,15]. After 30 years of age, muscle mass is reported to decline at an annual rate of approximately 1% to 2%, and that accelerates to as much as 1.5% to 3% per year after age 60 years, becoming ever faster after age 75 years (Fig. 1) [4,15].
Fig. 1. Changes of appendicular skeletal muscle mass (ASM), and ASM indices according to age trends in Korean (A) men and (B) women using data from Korea National Health and Nutrition Examination Study 2008 to 2010. ht2, height squared (m). Modified from Kim et al. [4].
Baumgartner et al. [16] first proposed that the appendicular skeletal muscle mass (ASM) divided by height squared (ASM/ht2) was as a representative muscle index. Clinically, sarcopenia was defined as relative ASM index less than 2 standard deviations below the mean values of healthy young adults or the lowest quintile of study populations [16,17]. However, recent studies have indicated that decline in muscle strength may be more important in the health outcomes related to sarcopenia [18]. Based on this, the European Working Group for Sarcopenia in Older People proposed reduced muscle mass with either muscle weakness or poor physical performance as the criteria for sarcopenia [2]. These criteria demonstrated better associations with various outcomes compared with the definitions driven only by muscle mass [19,20].
Meanwhile, the Foundation for the National Institutes of Health (FNIH) Sarcopenia Project has suggested a new criteria for sarcopenia categorized by muscle mass, muscle strength, and physical performance [21]. They proposed a new muscle mass index of ASM divided by body mass index. However, data about the clinical implications of the new FNIH criteria remain sparse.
Muscles play various important roles in the human body; thus, loss of muscle mass and strength can cause a diverse range of functional disability and metabolic derangements in older adults. Sarcopenia has been closely related to many clinical consequences, including functional disability, metabolic impairment, increased cardiovascular risk, and mortality, in the older Korean adults [6,22,23,24,25].
However, studies of sarcopenia in older adults with diabetes are few. The Health, Aging, and Body Composition (Health ABC) Study showed that older adults with type 2 diabetes lost their knee extensor strength more rapidly than nondiabetic subjects did [26]. In that study, diabetic patients had greater declines in muscle mass and leg muscle strength, and muscle quality was poorer in diabetic patients over 3 years. In addition, thigh muscle cross-sectional area also declined twice as fast in older women with diabetes than in nondiabetic subjects over 6 years [27]. Further, the Hertfordshire study demonstrated that older men newly diagnosed with diabetes have significantly weaker muscle strength and higher odds of impaired physical function than those without diabetes do [28]. Leenders et al. [29] also showed that leg lean mass and appendicular skeletal mass were significantly lower in older men with diabetes. Further, leg-extension strength in patients with diabetes was weaker than in nondiabetic subjects, and functional performance was impaired in older diabetic men. Other studies also have demonstrated that leg muscle strength and gait speed is reduced in older peoples with diabetes [30,31]
Kim et al. [32] reported that in Korean men and women aged ≥65 years, ASM was lower in diabetic patients compared with nondiabetic subjects but relative muscle index (ASM/height2) was lower only in older men with diabetes. The Korean Sarcopenic Obesity Study showed that sarcopenia (skeletal muscle mass/weight×100 <2 SD below the mean of the young reference) was present in 15.7% in subjects with diabetes and 6.9% in the control subjects [33]. Yoon et al. [34] demonstrated that muscle mass and strength in older diabetic patients were not different compared with nondiabetic subjects, but muscle quality was poorer and physical performance was impaired in diabetic subjects with poor glycemic control.
PATHOPHYSIOLOGY OF SARCOPENIA IN DIABETES
Multiple factors are associated with decreased muscle mass and/or strength in older adults. [2,17] The major causes or mechanisms related to sarcopenia include inadequate nutrition, physical inactivity or disuse, age-related hormonal changes including sex hormone and growth hormone, loss of motor neurons, atherosclerosis, obesity, insulin resistance, and inflammatory cytokines (Table 1).
Table 1. Major causes or mechanisms of sarcopenia in older adults.
| Primary | Age related: sex hormones, muscle apoptosis, mitochondrial dysfunction |
|---|---|
| Secondary | Activity related: physical inactivity, disuse, decon ditioning, zero gravity |
| Nutrition related: inadequate dietary intake, malabsorption, gastrointestinal disorders or medications that cause anorexia | |
| Endocrine disorder related: obesity, insulin resistance, inflammatory cytokine, steroid treatment, abnormal thyroid function | |
| Neurodegenerative disorder related: stroke, parkinsonism, diabetic neuropathy | |
| Chronic disease related: malignancy, advanced organ failure |
Additionally, diabetes mellitus will accelerate the reduction of muscle mass and strength because hyperglycemia, diabetic complications, obesity, insulin resistance, inflammatory cytokines, and endocrine changes associated with diabetes have adverse effects on muscle [35].
The mechanism of hyperglycemia that is associated with accelerated reduction of muscle mass and strength is still unclear. Weight loss associated with hyperglycemia may result in the loss of muscle mass and strength [36]. It is also reported that amino acid metabolism decreases in type 2 diabetes [37]. Insulin resistance inhibits the mammalian target of the rapamycin pathway that leads to protein synthesis and decreases protein degradation [38]. Insulin resistance also increases activation of the ubiquitin-proteasome pathway, resulting in degradation of muscle protein [37].
Chronic hyperglycemia increases advanced glycation end products (AGEs). AGEs accumulate in skeletal muscle and cartilage and increase the stiffness in patients with diabetes. It was reported that elevated AGEs were associated with poor grip strength in older women with moderate to severe disability and slow walking speed in older community-dwelling adults [39,40]. Higher skin autofluorescence, a noninvasive measurement of tissue AGEs, has been associated with lower grip strength and leg-extension power in Japanese men [41].
Another major cause of sarcopenia in diabetes is a decrease in motor neurons [42]. Diabetic neuropathy is a common complication of diabetes, especially in older adults, and it leads to muscle wasting and weakness of distal skeletal muscles [31]. Electrophysiological studies have shown that muscle strength of the ankle and knee extensors in patients with diabetes are correlated with fiber density and the amplitude of the macro motor unit potential [43], suggesting the loss of muscle strength because of incomplete reinnervation after axonal loss. A longitudinal follow-up study for diabetic polyneuropathy has shown that 8.3% of the patients had electrophysiological abnormalities at baseline; 16.7% had such abnormalities at 5 years; and 41.9% at 10 years [44]. Interestingly, diabetic patients with peripheral neuropathy had higher calf intermuscular adipose tissue volume, and higher adipose tissue volume was associated with poor muscle strength and physical function [45].
Diabetes is associated with an increase in inflammatory cytokines. It has been reported that systemic inflammatory cytokines such as tumor necrosis factor and interleukin 6 have detrimental effects on muscle mass, strength, and physical performance in older adults [46,47].
Testosterone increases satellite cell numbers and protein synthesis in muscle [48]. Serum testosterone levels decline gradually and progressively with aging in men. The men with diabetes and/or obesity have lower serum testosterone levels. Therefore, testosterone deficiency is another cause of sarcopenia in patients with diabetes.
FRAILTY AND DIABETES
Frailty is a common geriatric syndrome in older adults that carries an increased risk for poor health outcomes including falls, incident disability, hospitalization, and mortality because of decreased physical reserves [49]. Although agreement between a theoretical concept and an operational definition is lacking [50], Fried et al. [49] defined a clinical phenotype of frailty, which was identified by the presence of three or more of the five components (Table 2). An individual with one or two of the five components was considered prefrail. Frailty seems to be a dynamic process and also potentially reversible. Therefore, early detection of frailty and prevention or early interventions should be key issues in the care of older adults.
Table 2. Clinical phenotype of frailty proposed by Fried et al.
| Weight loss | Unintentional loss of ≥4.5 kg in the past year |
| Weakness | Hand-grip strength in the lowest 20% quintile adjusted for sex and body mass index |
| Exhaustion | Poor endurance and energy, self-reported from the Center for Epidemiologic Studies Depression Scale |
| Slowness | Walking speed under the lowest quintile adjusted for sex and height |
| Low physical activity level | Lowest quintile of kilocalories of physical activity during the past week, measured by the Minnesota Leisure Activity Scale |
Modified from Fried et al., with permission from Oxford University Press [49].
Fried et al. [51] also proposed the cycle of frailty, in which sarcopenia was one of the main potential causes of frailty. Actually, sarcopenia and frailty have a commonality and may share the similar pathway for multiple pathologic processes in older people. Thus, sarcopenia may be an intermediate step in the development of frailty in patients with diabetes.
Several studies have shown that diabetic patients aged 65 years or older were more likely to be frail than nondiabetic older adults were [52,53,54]. These studies also reported that frail patients with diabetes had a higher mortality than nonfrail patients, and the presence of frailty was an independent risk factor for mortality. The German ESTHER (Epidemiologische Studie zu Chancen der Verhütung, Früherkennung und optimierten Therapie chronischer Erkrankungen in der älteren Bevölkerung) study and the Whitehall II Prospective Study demonstrated that the prevalence of frailty was 3- to 5-fold higher in patients with diabetes older than 65 years than that seen in the general population [55,56].
MANAGEMENT OF FRAILTY IN DIABETES
Morley et al. [35] suggested that the management of frailty in patients with diabetes initially should focus on the prevention of sarcopenia. Several consensus reports recommended the measurement of gait speed as a screening method on clinical practice [2,17]. Until now, no pharmacologic agent to prevent or treat sarcopenia has proven to be as efficacious as exercise (mainly resistance training) is in combination with nutritional intervention (adequate protein and energy intake) [57]. This approach is currently the key strategy for the management of sarcopenia and frailty.
Larger muscles in the body move in a rhythmic manner for a prolonged period during aerobic exercise, whereas resistance exercise involves muscles working hard against an applied force or weight such as in weight lifting. Both aerobic and resistance exercise training have been shown to prevent the decline in muscle mass and strength with age [58]. Although aerobic exercise is less likely to contribute to muscle hypertrophy, it has been linked to improvements in cardiovascular fitness and endurance capacity. Aerobic exercise can also reduce body fat including intra- and intermuscular fat, which in turn improves the functional role of muscle relative to body weight [59,60]. In contrast, resistance exercise training appears to have a larger effect on augmenting muscle mass and strength, and it attenuates the development of sarcopenia [61,62]. Improvements in muscle strength can be achieved with as little as one resistance exercise training session per week [63].
Many older people do not consume sufficient amounts of dietary intake and protein, which leads to a reduction in lean body mass and increased functional disability [64]. The current recommended dietary allowance (RDA) of dietary protein is 0.8 g/kg/day, but 40% of people aged over 70 years did not meet this RDA [65]. Older women taking a low protein diet below the RDA had a significant decline in muscle mass and strength [66]. Further, older people who took the protein of RDA had a negative nitrogen balance and might require a higher protein content than the RDA to maintain their skeletal muscle [67]. Although older adults who exercise may have additional protein requirements, studies investigating whether nutritional supplementation in combination with resistance exercise can augment muscle strength and mass have yielded inconsistent results [68]. Nutritional supplementation may result in an overall decrease in voluntary food intake and adherence to the supplements can be a problem [69].
Additionally, three treatable causes should be managed for the treatment of frailty [35]: (1) treatable causes of fatigue: vitamin B12 deficiency, adrenal inefficiency, hypothyroidism, anemia, sleep apnea, hypotension, syncope, and depression; (2) polypharmacy: anticholinergic medication, overtreatment of blood pressure, hypoglycemia; (3) and unintentional weight loss: depression, medications, dysphagia, dental problems, and nosocomial infections.
CONCLUSIONS
As larger populations are now aging, there is a tremendous increase of older adults with diabetes. Aging and diabetes are both risk factors for functional impairment. A recent systematic review article showed that diabetes is associated with a strong increase in the risk of physical disability in older adults [11]. This will increase both direct and indirect health-related costs. I believe that early detection of sarcopenia and frailty in older adults with diabetes should be routine clinical practice to facilitate early multimodal interventions.
ACKNOWLEDGMENTS
This work was supported by the National Research Foundation Grant (No. 2006-2005410) of the Ministry of Education, Science, and Technology and a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI15C3207). I thank Professors Hyung-Joon Yoo and Ki-Up Lee for the scientific leadership in the field of elderly diabetes.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.The Population Reference Bureau: 2014 World population data sheet. [cited 2016 Feb 27]. Available from: http://www.prb.org/pdf14/2014-world-population-data-sheet_eng.pdf.
- 2.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis. Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abellan van Kan G. Epidemiology and consequences of sarcopenia. J Nutr Health Aging. 2009;13:708–712. doi: 10.1007/s12603-009-0201-z. [DOI] [PubMed] [Google Scholar]
- 4.Kim KM, Lim S, Choi KM, Kim JH, Yu SH, Kim TN, Song W, Lim JY, Won CW, Yoo HJ, Jang HC Sarcopenia Study Group of Korean Geriatrics Society. Sarcopenia in Korea: prevalence and clinical aspects. J Korean Geriatr Soc. 2015;19:1–8. [Google Scholar]
- 5.Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim JH, Lim S, Choi SH, Kim KM, Yoon JW, Kim KW, Lim JY, Park KS, Jang HC. Sarcopenia: an independent predictor of mortality in community-dwelling older Korean men. J Gerontol A Biol Sci Med Sci. 2014;69:1244–1252. doi: 10.1093/gerona/glu050. [DOI] [PubMed] [Google Scholar]
- 7.Resnick HE, Harris MI, Brock DB, Harris TB. American Diabetes Association diabetes diagnostic criteria, advancing age, and cardiovascular disease risk profiles: results from the Third National Health and Nutrition Examination Survey. Diabetes Care. 2000;23:176–180. doi: 10.2337/diacare.23.2.176. [DOI] [PubMed] [Google Scholar]
- 8.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–308. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee YJ, Jang HC, Kim EH, Kim HJ, Lee SB, Choi SH, Lim S, Park KU, Park YJ, Kim KW. Association between apolipoprotein E polymorphism and type 2 diabetes in subjects aged 65 or over. Korean Diabetes J. 2008;32:30–37. [Google Scholar]
- 10.De Rekeneire N, Resnick HE, Schwartz AV, Shorr RI, Kuller LH, Simonsick EM, Vellas B, Harris TB Health, Aging, and Body Composition study. Diabetes is associated with subclinical functional limitation in nondisabled older individuals: the Health, Aging, and Body Composition study. Diabetes Care. 2003;26:3257–3263. doi: 10.2337/diacare.26.12.3257. [DOI] [PubMed] [Google Scholar]
- 11.Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, Peeters A. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1:106–114. doi: 10.1016/S2213-8587(13)70046-9. [DOI] [PubMed] [Google Scholar]
- 12.Caruso LB, Silliman RA, Demissie S, Greenfield S, Wagner EH. What can we do to improve physical function in older persons with type 2 diabetes? J Gerontol A Biol Sci Med Sci. 2000;55:M372–M377. doi: 10.1093/gerona/55.7.m372. [DOI] [PubMed] [Google Scholar]
- 13.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 14.Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Nevitt M, Harris TB. Weight change and the conservation of lean mass in old age: the Health, Aging and Body Composition Study. Am J Clin Nutr. 2005;82:872–878. doi: 10.1093/ajcn/82.4.872. [DOI] [PubMed] [Google Scholar]
- 15.Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MA. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am J Clin Nutr. 2002;76:473–481. doi: 10.1093/ajcn/76.2.473. [DOI] [PubMed] [Google Scholar]
- 16.Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–763. doi: 10.1093/oxfordjournals.aje.a009520. [DOI] [PubMed] [Google Scholar]
- 17.Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, Cederholm T, Chandler J, De Meynard C, Donini L, Harris T, Kannt A, Keime Guibert F, Onder G, Papanicolaou D, Rolland Y, Rooks D, Sieber C, Souhami E, Verlaan S, Zamboni M. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12:249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newman AB, Kupelian V, Visser M, Simonsick EM, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Rubin SM, Harris TB. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci. 2006;61:72–77. doi: 10.1093/gerona/61.1.72. [DOI] [PubMed] [Google Scholar]
- 19.Landi F, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, Bernabei R, Onder G. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012;31:652–658. doi: 10.1016/j.clnu.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Woo J, Leung J, Sham A, Kwok T. Defining sarcopenia in terms of risk of physical limitations: a 5-year follow-up study of 3,153 Chinese men and women. J Am Geriatr Soc. 2009;57:2224–2231. doi: 10.1111/j.1532-5415.2009.02566.x. [DOI] [PubMed] [Google Scholar]
- 21.Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L, Guralnik JM, Fragala MS, Kenny AM, Kiel DP, Kritchevsky SB, Shardell MD, Dam TT, Vassileva MT. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69:547–558. doi: 10.1093/gerona/glu010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim JH, Choi SH, Lim S, Yoon JW, Kang SM, Kim KW, Lim JY, Cho NH, Jang HC. Sarcopenia and obesity: gender-different relationship with functional limitation in older persons. J Korean Med Sci. 2013;28:1041–1047. doi: 10.3346/jkms.2013.28.7.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim KE, Jang SN, Lim S, Park YJ, Paik NJ, Kim KW, Jang HC, Lim JY. Relationship between muscle mass and physical performance: is it the same in older adults with weak muscle strength? Age Ageing. 2012;41:799–803. doi: 10.1093/ageing/afs115. [DOI] [PubMed] [Google Scholar]
- 24.Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, Kim KW, Lim JY, Park KS, Jang HC. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA) Diabetes Care. 2010;33:1652–1654. doi: 10.2337/dc10-0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim KM, Lim S, Choi SH, Kim JH, Shin CS, Park KS, Jang HC. Cardiometabolic implication of sarcopenia: the Korea National Health and Nutrition Examination Study (KNHANES) 2008-2010. IJC Metab Endocr. 2014;4:63–69. [Google Scholar]
- 26.Park SW, Goodpaster BH, Strotmeyer ES, Kuller LH, Broudeau R, Kammerer C, de Rekeneire N, Harris TB, Schwartz AV, Tylavsky FA, Cho YW, Newman AB Health, Aging, and Body Composition Study. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes Care. 2007;30:1507–1512. doi: 10.2337/dc06-2537. [DOI] [PubMed] [Google Scholar]
- 27.Park SW, Goodpaster BH, Lee JS, Kuller LH, Boudreau R, de Rekeneire N, Harris TB, Kritchevsky S, Tylavsky FA, Nevitt M, Cho YW, Newman AB Health, Aging, and Body Composition Study. Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care. 2009;32:1993–1997. doi: 10.2337/dc09-0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sayer AA, Dennison EM, Syddall HE, Gilbody HJ, Phillips DI, Cooper C. Type 2 diabetes, muscle strength, and impaired physical function: the tip of the iceberg? Diabetes Care. 2005;28:2541–2542. doi: 10.2337/diacare.28.10.2541. [DOI] [PubMed] [Google Scholar]
- 29.Leenders M, Verdijk LB, van der Hoeven L, Adam JJ, van Kranenburg J, Nilwik R, van Loon LJ. Patients with type 2 diabetes show a greater decline in muscle mass, muscle strength, and functional capacity with aging. J Am Med Dir Assoc. 2013;14:585–592. doi: 10.1016/j.jamda.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 30.Volpato S, Bianchi L, Lauretani F, Lauretani F, Bandinelli S, Guralnik JM, Zuliani G, Ferrucci L. Role of muscle mass and muscle quality in the association between diabetes and gait speed. Diabetes Care. 2012;35:1672–1679. doi: 10.2337/dc11-2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalyani RR, Tra Y, Yeh HC, Egan JM, Ferrucci L, Brancati FL. Quadriceps strength, quadriceps power, and gait speed in older U.S. adults with diabetes mellitus: results from the National Health and Nutrition Examination Survey, 1999-2002. J Am Geriatr Soc. 2013;61:769–775. doi: 10.1111/jgs.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim KS, Park KS, Kim MJ, Kim SK, Cho YW, Park SW. Type 2 diabetes is associated with low muscle mass in older adults. Geriatr Gerontol Int. 2014;14(Suppl 1):115–121. doi: 10.1111/ggi.12189. [DOI] [PubMed] [Google Scholar]
- 33.Kim TN, Park MS, Yang SJ, Yoo HJ, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Prevalence and determinant factors of sarcopenia in patients with type 2 diabetes: the Korean Sarcopenic Obesity Study (KSOS) Diabetes Care. 2010;33:1497–1499. doi: 10.2337/dc09-2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoon JW, Ha YC, Kim KM, Moon JH, Choi SH, Lim S, Park YJ, Lim JY, Kim KW, Park KS, Jang HC. Hyperglycemia is associated with impaired muscle quality in older men with diabetes: the Korean Longitudinal Study on Health and Aging. Diabetes Metab J. 2016;40:140–146. doi: 10.4093/dmj.2016.40.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morley JE, Malmstrom TK, Rodriguez-Manas L, Sinclair AJ. Frailty, sarcopenia and diabetes. J Am Med Dir Assoc. 2014;15:853–859. doi: 10.1016/j.jamda.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 36.von Haehling S, Morley JE, Anker SD. From muscle wasting to sarcopenia and myopenia: update 2012. J Cachexia Sarcopenia Muscle. 2012;3:213–217. doi: 10.1007/s13539-012-0089-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang X, Hu Z, Hu J, Du J, Mitch WE. Insulin resistance accelerates muscle protein degradation: activation of the ubiquitin-proteasome pathway by defects in muscle cell signaling. Endocrinology. 2006;147:4160–4168. doi: 10.1210/en.2006-0251. [DOI] [PubMed] [Google Scholar]
- 38.Lawrence JC., Jr mTOR-dependent control of skeletal muscle protein synthesis. Int J Sport Nutr Exerc Metab. 2001;11:S177–S185. doi: 10.1123/ijsnem.11.s1.s177. [DOI] [PubMed] [Google Scholar]
- 39.Dalal M, Ferrucci L, Sun K, Beck J, Fried LP, Semba RD. Elevated serum advanced glycation end products and poor grip strength in older community-dwelling women. J Gerontol A Biol Sci Med Sci. 2009;64:132–137. doi: 10.1093/gerona/gln018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Semba RD, Bandinelli S, Sun K, Guralnik JM, Ferrucci L. Relationship of an advanced glycation end product, plasma carboxymethyl-lysine, with slow walking speed in older adults: the InCHIANTI study. Eur J Appl Physiol. 2010;108:191–195. doi: 10.1007/s00421-009-1192-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Momma H, Niu K, Kobayashi Y, Guan L, Sato M, Guo H, Chujo M, Otomo A, Yufei C, Tadaura H, Saito T, Mori T, Miyata T, Nagatomi R. Skin advanced glycation end product accumulation and muscle strength among adult men. Eur J Appl Physiol. 2011;111:1545–1552. doi: 10.1007/s00421-010-1779-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andreassen CS, Jakobsen J, Andersen H. Muscle weakness: a progressive late complication in diabetic distal symmetric polyneuropathy. Diabetes. 2006;55:806–812. doi: 10.2337/diabetes.55.03.06.db05-1237. [DOI] [PubMed] [Google Scholar]
- 43.Andersen H, Stalberg E, Gjerstad MD, Jakobsen J. Association of muscle strength and electrophysiological measures of reinnervation in diabetic neuropathy. Muscle Nerve. 1998;21:1647–1654. doi: 10.1002/(sici)1097-4598(199812)21:12<1647::aid-mus4>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 44.Partanen J, Niskanen L, Lehtinen J, Mervaala E, Siitonen O, Uusitupa M. Natural history of peripheral neuropathy in patients with non-insulin-dependent diabetes mellitus. N Engl J Med. 1995;333:89–94. doi: 10.1056/NEJM199507133330203. [DOI] [PubMed] [Google Scholar]
- 45.Tuttle LJ, Sinacore DR, Cade WT, Mueller MJ. Lower physical activity is associated with higher intermuscular adipose tissue in people with type 2 diabetes and peripheral neuropathy. Phys Ther. 2011;91:923–930. doi: 10.2522/ptj.20100329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci. 2002;57:M326–M332. doi: 10.1093/gerona/57.5.m326. [DOI] [PubMed] [Google Scholar]
- 47.Cesari M, Penninx BW, Pahor M, Lauretani F, Corsi AM, Rhys Williams G, Guralnik JM, Ferrucci L. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2004;59:242–248. doi: 10.1093/gerona/59.3.m242. [DOI] [PubMed] [Google Scholar]
- 48.Sinha-Hikim I, Cornford M, Gaytan H, Lee ML, Bhasin S. Effects of testosterone supplementation on skeletal muscle fiber hypertrophy and satellite cells in community-dwelling older men. J Clin Endocrinol Metab. 2006;91:3024–3033. doi: 10.1210/jc.2006-0357. [DOI] [PubMed] [Google Scholar]
- 49.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 50.Rodriguez-Manas L, Feart C, Mann G, Vina J, Chatterji S, Chodzko-Zajko W, Gonzalez-Colaco Harmand M, Bergman H, Carcaillon L, Nicholson C, Scuteri A, Sinclair A, Pelaez M, Van der Cammen T, Beland F, Bickenbach J, Delamarche P, Ferrucci L, Fried LP, Gutierrez-Robledo LM, Rockwood K, Rodriguez Artalejo F, Serviddio G, Vega E FOD-CC group (Appendix 1). Searching for an operational definition of frailty: a Delphi method based consensus statement: the frailty operative definition-consensus conference project. J Gerontol A Biol Sci Med Sci. 2013;68:62–67. doi: 10.1093/gerona/gls119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fried LP, Walston J. Principles of geriatric medicine and gerontology. 5th ed. New York: McGraw Hill; 2003. Chapter 116, Frailty and failure to thrive; pp. 1487–1502. [Google Scholar]
- 52.Ottenbacher KJ, Graham JE, Al Snih S, Raji M, Samper-Ternent R, Ostir GV, Markides KS. Mexican Americans and frailty: findings from the Hispanic established populations epidemiologic studies of the elderly. Am J Public Health. 2009;99:673–679. doi: 10.2105/AJPH.2008.143958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hubbard RE, Andrew MK, Fallah N, Rockwood K. Comparison of the prognostic importance of diagnosed diabetes, co-morbidity and frailty in older people. Diabet Med. 2010;27:603–606. doi: 10.1111/j.1464-5491.2010.02977.x. [DOI] [PubMed] [Google Scholar]
- 54.Cacciatore F, Testa G, Galizia G, Della-Morte D, Mazzella F, Langellotto A, Pirozzi G, Ferro G, Gargiulo G, Ferrara N, Rengo F, Abete P. Clinical frailty and long-term mortality in elderly subjects with diabetes. Acta Diabetol. 2013;50:251–260. doi: 10.1007/s00592-012-0413-2. [DOI] [PubMed] [Google Scholar]
- 55.Saum KU, Dieffenbach AK, Muller H, Holleczek B, Hauer K, Brenner H. Frailty prevalence and 10-year survival in community-dwelling older adults: results from the ESTHER cohort study. Eur J Epidemiol. 2014;29:171–179. doi: 10.1007/s10654-014-9891-6. [DOI] [PubMed] [Google Scholar]
- 56.Bouillon K, Kivimaki M, Hamer M, Shipley MJ, Akbaraly TN, Tabak A, Singh-Manoux A, Batty GD. Diabetes risk factors, diabetes risk algorithms, and the prediction of future frailty: the Whitehall II prospective cohort study. J Am Med Dir Assoc. 2013;14:851.e1–851.e6. doi: 10.1016/j.jamda.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rolland Y, Onder G, Morley JE, Gillette-Guyonet S, Abellan van Kan G, Vellas B. Current and future pharmacologic treatment of sarcopenia. Clin Geriatr Med. 2011;27:423–447. doi: 10.1016/j.cger.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 58.Frankel JE, Bean JF, Frontera WR. Exercise in the elderly: research and clinical practice. Clin Geriatr Med. 2006;22:239–256. vii. doi: 10.1016/j.cger.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 59.Short KR, Vittone JL, Bigelow ML, Proctor DN, Nair KS. Age and aerobic exercise training effects on whole body and muscle protein metabolism. Am J Physiol Endocrinol Metab. 2004;286:E92–E101. doi: 10.1152/ajpendo.00366.2003. [DOI] [PubMed] [Google Scholar]
- 60.Misic MM, Rosengren KS, Woods JA, Evans EM. Muscle quality, aerobic fitness and fat mass predict lower-extremity physical function in community-dwelling older adults. Gerontology. 2007;53:260–266. doi: 10.1159/000101826. [DOI] [PubMed] [Google Scholar]
- 61.Sipila S, Suominen H. Effects of strength and endurance training on thigh and leg muscle mass and composition in elderly women. J Appl Physiol (1985) 1995;78:334–340. doi: 10.1152/jappl.1995.78.1.334. [DOI] [PubMed] [Google Scholar]
- 62.Frontera WR, Meredith CN, O'Reilly KP, Knuttgen HG, Evans WJ. Strength conditioning in older men: skeletal muscle hypertrophy and improved function. J Appl Physiol (1985) 1988;64:1038–1044. doi: 10.1152/jappl.1988.64.3.1038. [DOI] [PubMed] [Google Scholar]
- 63.Taaffe DR, Duret C, Wheeler S, Marcus R. Once-weekly resistance exercise improves muscle strength and neuromuscular performance in older adults. J Am Geriatr Soc. 1999;47:1208–1214. doi: 10.1111/j.1532-5415.1999.tb05201.x. [DOI] [PubMed] [Google Scholar]
- 64.Bartali B, Frongillo EA, Bandinelli S, Lauretani F, Semba RD, Fried LP, Ferrucci L. Low nutrient intake is an essential component of frailty in older persons. J Gerontol A Biol Sci Med Sci. 2006;61:589–593. doi: 10.1093/gerona/61.6.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, Lee JS, Sahyoun NR, Visser M, Kritchevsky SB Health ABC Study. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2008;87:150–155. doi: 10.1093/ajcn/87.1.150. [DOI] [PubMed] [Google Scholar]
- 66.Castaneda C, Charnley JM, Evans WJ, Crim MC. Elderly women accommodate to a low-protein diet with losses of body cell mass, muscle function, and immune response. Am J Clin Nutr. 1995;62:30–39. doi: 10.1093/ajcn/62.1.30. [DOI] [PubMed] [Google Scholar]
- 67.Campbell WW, Trappe TA, Wolfe RR, Evans WJ. The recommended dietary allowance for protein may not be adequate for older people to maintain skeletal muscle. J Gerontol A Biol Sci Med Sci. 2001;56:M373–M380. doi: 10.1093/gerona/56.6.m373. [DOI] [PubMed] [Google Scholar]
- 68.Bonnefoy M, Cornu C, Normand S, Boutitie F, Bugnard F, Rahmani A, Lacour JR, Laville M. The effects of exercise and protein-energy supplements on body composition and muscle function in frail elderly individuals: a long-term controlled randomised study. Br J Nutr. 2003;89:731–739. doi: 10.1079/BJN2003836. [DOI] [PubMed] [Google Scholar]
- 69.Milne AC, Potter J, Vivanti A, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev. 2009;(2):CD003288. doi: 10.1002/14651858.CD003288.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]