Abstract
Introduction
Extramammary Paget's disease (EMPD) occurs commonly in perineum, vulva and perineal region and is considered as a complex disorder due to different clinical and histological features.
Presentation of case
A 61 years old woman had a dermatologic evaluation for anal itch and underwent a skin biopsy with diagnostic of Paget disease in perianal region. Pelvic magnetic resonance showed a huge tumor which involved skin, derma and gluteus and she firstly refused any surgical treatment. One year later, because of increasing of the tumor and bleeding, she underwent the surgical procedure with a complete excision, resection of the skin of the anus, inguinal lymphadenectomy and left colostomy. Because of lymph nodes metastasis, a VLS Miles was sequentially performed. She started oncological follow up that showed liver, lung and pelvic metastasis. She survived for 24 months after surgery.
Discussion
In literature, less than 200 cases of perineal Paget's disease have been reported. EMPD in some cases has an associated adenocarcinoma, which has been associated with a worse prognosis and high mortality. Wrong diagnosis and a superficial consideration of a benign evolution should be considered as the first mistake in clinical practice.
Conclusion
Our surgical approach is considered in literature as the best one for those cases, followed by the oncological treatment. Those patients need to be better studied and more attention should be paid to the clinical presentation.
Keywords: Perineal Paget's disease, Extramammary Paget's disease
Highlights
-
•
A case of Extramammary Paget's disease (EMPD) is proposed.
-
•
Clinical presentation needs to be well studied and considered for the diagnostic.
-
•
A wide surgical excision and oncological treatment are mandatory to face this kind of tumor.
1. Introduction
Perianal Paget's disease (PPD) is a rare malignancy and less than 200 cases have been reported in literature. Extramammary Paget's disease (EMPD) is an uncommon entity. It frequently affects most women and Caucasian people in general, with a peak of incidence between 50 and 80 years old [1]. EMPD occurs in an apocrine gland distribution. The most commonly affected sites are the vulva, perineum, perianal region, scrotum, penis, or pubic area [2]. There is also a familiar EMPD (seven cases), although, genetic bases are still unknown [3]. Paget's disease, because of its associations with different synchronous or metachronous malignancies, is considered as a complex disorder due to pathological processes different in clinical and histological features. The prognosis of simple PPD is relatively favorable, both overall and disease-free survival are approximately 60% at 5-year [4]. However, one subtype of this malignancy, PPD with synchronous or metachronous carcinoma of the anorectum, has a poor prognosis, based on limited reports on this entity [4], [5]. The natural course of the disease and its optional management is still unknown.
2. Clinical case
After a dermatologic evaluation for anal itch, a 61 years old woman underwent a skin biopsy whose subsequent histological exam deposed for Paget disease in perianal region Fig 1. After that biopsy, the patient has been controlled for several months by the plastic surgeons without any improvement, and one year later, she performed a colonoscopy with evidence of left colonic diverticulitis and a perianal mass. Primarily she refused any surgical treatment proposed. During the same time she underwent a pelvic Magnetic Resonance which described inhomogeneous tissue with high enhancement and a depth of 3.8 cm and a length of 8 cm on the right side of the anus which involved skin, derma and gluteus. During the following year, because of the bleeding and the increase of the mass, she decided to be submitted to surgery. A complete excision of the tumor was performed associated to the resection of the skin of the anus, inguinal lymphadenectomy and left colostomy. The subsequent specimen was positive for lymph node metastasis, with infiltration of the internal sphincter and the histological pattern was a mildly differentiated adenocarcinoma with focal aspect of Paget. The resection margins were positive for tumor. She performed a TB CT scan that didn't show any evidence of metastasis. After this histological result she was readmitted to the operating room to perform a VLS Miles resection end excision of the big lip of the vagina (Fig. 2) with a terminal left colostomy. The definitive histological exam was positive for metastasis in 3 perirectal lymph nodes and massive infiltration of the right big lip of the vagina. The patient was dismissed after 20 days. She started oncologic follow up with laboratory data and total body CT scan that showed liver and abdominal metastasis. A PET-CT scan showed different pathological backlog of the radiopharmaceutical at the liver (SUV max 6,4), and at the inguinal region (SUV max 3,4), ascribable to adenopathy. During the following 12 months, she was submitted to 6 cycles of Chemotherapy (CHT) according to the XELOX protocol and also she underwent an UltraSound scan of the right inferior leg that highlighted a total thrombosis of the right external iliac vein and of the femoral vein and for this reason she started therapy with low molecular weight heparin. After the first CHT step she started other 3 cycles with FOLFOX4-Bevacizumab. Unfortunately laboratory data showed a constant increase of CA 19,9, TPA and liver function tests. Last follow up was made at 24months after the surgery and the CT scan showed an increase of liver, lung and perianal metastasis. After one month the patient died because of hepatic failure.
Fig. 1.
At the perianal region presence of dystrophic skin of about 8 cm long reddish, hard, painful, sometimes bloody, itchy.
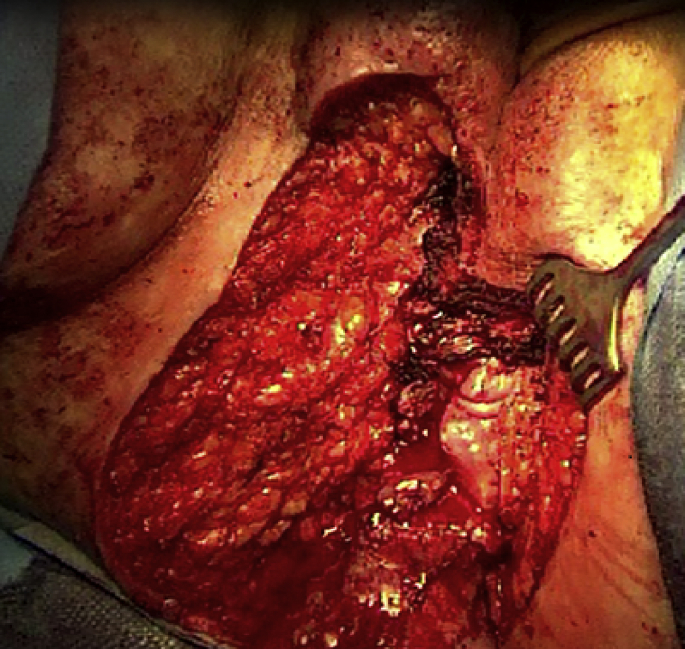
Fig. 2.
Intra-operative image.
3. Discussion
Extramammary Paget disease (EMPD) is a rare cutaneous intraepithelial adenocarcinoma that originates from apocrine glands of the genital and perianal regions and may involve different areas such as vulva, penis and axilla. The most important prognostic factor is depth of invasion; in fact tumors with depth of >1 mm are associated with poorer prognosis while spreading outside the skin into lymph nodes or other tissues are higher risk [6]. When EMPD originates in the perianal region, is called perianal Paget disease (PPD). Usually all forms of EMPD are treated by surgical excision. Frequently PPD occurs later in life in high surgical risk patients. The true incidence of the disease is difficult to estimate due to its rarity, but it is known to represent less than 1% of all anal diseases and 6.5% of all cases of Paget's disease [7]. Pathogenesis of PPD is controversial. Helwig and Graham [8] consider perianal and vulvar Paget's disease as a manifestation of a multicentric effect of an un-known carcinogenic stimulus on apocrine structures, epidermis and glandular elements of the rectum and urethra. The first historical report of this clinical situation was first described by Sir James Paget in 1874 [9], who referred about an intraepithelial carcinoma of the breast and suggested that this clinical pattern might also be found in other district. The first case of EMPD was described by Crocker in 1888, and perianal EMPD was first reported in 1893 by Darier and Coulillaud [10]. Fewer than 200 cases of PPD have been reported in literature and the true incidence is difficult to estimate. PPD commonly occurs in women of the 5th decade [11]. PPD and its incidence is higher in persons between 50 and 70 years of age, [12]. Patients with EMPD in 24% have an associated adenocarcinoma, which has been associated with a worse prognosis, with mortality rates up to 46% [13]. Usually patients with PPD came to our attention with non-specific symptoms such as bleeding, pruritus, eczema, pain at defecation. Clinical presentation of PPD is an erythematous plate with squamous areas which may sweet fluid. The size of the plate may rise from 1 cm to the entire perineal region. The margins of the lesion are usually erythematous with dermatitis. Always patients refer unsuccessful therapy with topical steroids. When local therapy is not useful for a certain time, PPD should be suspected and a biopsy of the lesion should be performed. Histologically, PPD is characterized by large vacuolated cells with mucin content, called Paget cells. They may also contain cytokeratin and carcinoembryonic antigen, which may be identified with immunofluorescence. CK7, CK19, and C-erb B2 are immunohistochemical markers for the diagnosis of EMPD [14]. Most dermatology textbooks recommend surgical excision as the “gold standard.” The recommended approaches are, for noninvasive lesions, extended surgical excision and for invasive disease or lesions associated with carcinoma, abdominoperineal excision or excision of rectum [15]. Primary treatment with radiation therapy is seldom used but most consider wide surgical excision to be the treatment of choice. Elderly patients, who are often undesirable surgical candidates, may benefit from primary radiotherapy as an alternative. Typically, the side effects from perianal radiotherapy include acute dermatitis, moist desquamation, and mild-to-late skin atrophy, all of which are manageable with moisturizing creams. Perianal Paget disease is a rare condition and remains a therapeutic challenge for clinicians. No randomized trials have yet been performed comparing surgical excision and radiation therapy. The previous reports that included radiotherapy poorly described the technical details and outcome of treatment. Radiotherapy can be considered in selected cases an effective treatment modality and a suitable alternative to wide surgical excision [16], but our patient refused any radiation treatment. Many authors described nonsurgical treatment first Kobayashi reported the effect of intralesional interferon [17]. Cohen reported the results of the topical imiquimod in 9 cases of EMPD, that have shown promising results in 8–16 weeks of therapy with lifelong follow-up [18], [19]. However, many authors recommended surgical treatment, including a wide local excision through abdominoperineal excision because it has a good prognosis [16].
4. Conclusions
Less than 200 cases of PPD have been reported in literature. EMPD occurs in an apocrine gland distribution. Wrong diagnosis and a superficial consideration of a benign evolution should be considered as the first mistake in clinical practice. According to the literature, in our case the best approach considered was a wide surgical excision with resection of the skin of the anus, inguinal lymphadenectomy and left colostomy as first step, then, because of positive lymph nodes and invasion of internal anal sphincter VLS Miles was performed and oncological treatment. In perineal region PPD is quite often associated to anorectal carcinoma, therefore it needs to be better studied and more attention should be paid to its presentation.
Ethical approval
We haven't involved ethics committee because It's a case report.
Sources of funding
It's a case report without sponsor.
Author contribution
Giuseppe Carbotta: study concept.
Antonio Prestera: write the paper.
Pierluca Sallustio: write the paper.
Rita Laforgia: English translate.
Pierluigi Lobascio: rewied of literature.
Prof Nicola Palasciano: supervisor.
Conflicts of interest
We declare all authors haven't conflicts of interest.
Guarantor
Giuseppe Carbotta md, corresponding author and guarantor.
Consent section
“Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
References
- 1.Shepherd V., Davidson E.J., Davies-Humphreys J. Extramammary Paget's disease. BJOG. 2005;112(3):273–279. doi: 10.1111/j.1471-0528.2004.00438.x. [DOI] [PubMed] [Google Scholar]
- 2.Kanitakis J. Mammary and extramammary Paget's disease. J. Eur. Acad. Dermatol. Venereol. 2007 May;21(5):581–590. doi: 10.1111/j.1468-3083.2007.02154.x. http://www.ncbi.nlm.nih.gov/pubmed/17447970. [DOI] [PubMed] [Google Scholar]
- 3.McCarter M.D., Quan S.H., Busam K., Paty P.P., Wong D., Guillem J.G. Long-term outcome of perianal Paget's disease. Dis. Colon Rectum. 2003 May;46(5):612–616. doi: 10.1007/s10350-004-6618-x. [DOI] [PubMed] [Google Scholar]
- 4.Marchesa P., Fazio V.W., Oliart S., Goldblum J.R., Lavery I.C., Milsom J.W. Long-term outcome of patients with Perianal Paget's disease. Ann. Surg. Oncol. 1997;4:475–480. doi: 10.1007/BF02303671. [DOI] [PubMed] [Google Scholar]
- 5.Williams S.L., Rogers L.W., Quan S.H. Perianal Paget's disease: report of seven cases. Dis. Colon Rectum. 1976;19:30–40. doi: 10.1007/BF02590848. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J.M., Granter S.R., Werchniak A.E. Risk stratification in extramammary Paget disease. Clin. Exp. Dermatol. 2015;40(5):473–478. doi: 10.1111/ced.12690. [DOI] [PubMed] [Google Scholar]
- 7.Kyriazanos ID, Stamos NP, Miliadis L, Noussis G, Stoidis CN. Extra-mammary Paget's disease of the perianal region: a review of the literature emphasizing the operative management technique. [DOI] [PubMed]
- 8.Helwig E.B., Graham J.H. Anogenital (extramammary) Paget's disease. A clinicopathological study. Cancer. 1963;16:387–403. doi: 10.1002/1097-0142(196303)16:3<387::aid-cncr2820160314>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 9.Paget J. Vol. 10. 1874. pp. 87–89. (On disease of the mammary areola preceding cancer of the mammary gland). St Bartholomew’s Hospital Report. [Google Scholar]
- 10.Darier J., Coulillaud P. Concerning a case of Paget disease of the perineal and scrotal area. Ann. Dermatol. Syphiligr. Paris. 1893;4:25–33. [Google Scholar]
- 11.Amin R. Perianal Paget's disease. Br. J. Radiol. 1999;72:610–612. doi: 10.1259/bjr.72.858.10560346. [DOI] [PubMed] [Google Scholar]
- 12.Shepherd N.A. Anal intraepithelial neoplasia and other neoplastic precursor lesions of the anal canal and perianal region. Gastroenterol. Clin. North Am. 2007;36:969–987. doi: 10.1016/j.gtc.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Chanda J.J. Extramammary Paget's disease: prognosis and relationship to internal malignancy. J. Am. Acad. Dermatol. 1985;13:1009–1014. doi: 10.1016/s0190-9622(85)70254-x. [DOI] [PubMed] [Google Scholar]
- 14.Banerjee S., Chatterjee M., Chand K. Extramammary Paget's disease. Indian J. Dermatol. Venereol. Leprol. 2005;71:417–420. doi: 10.4103/0378-6323.18948. [DOI] [PubMed] [Google Scholar]
- 15.Coldiron B.M., Goldsmith B.A., Robinson J.K. Surgical treatment of extramammary Paget's disease. A report of six cases and a reexamination of Mohs micrographic surgery compared with conventional surgical excision. Cancer. 1991;67:933–938. doi: 10.1002/1097-0142(19910215)67:4<933::aid-cncr2820670413>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 16.Liu C., Wang Q., Kong Y., Tu X., Wang J., Zhu X. A clinicopathological study of perianal Paget's disease associated with internal rectal adenocarcinoma. Zhonghua Bing Li Xue Za Zhi. 2004;33:11–15. [PubMed] [Google Scholar]
- 17.Kobayashi H., Someda Y., Furukawa M., Chanoki M., Hamada T. Intralesional interferon in the treatment of extramammary Paget's disease. Nihon Hifuka Gakkai Zasshi. 1987;97:1–7. [PubMed] [Google Scholar]
- 18.Cohen P.R., Schulze K.E., Tschen J.A., Hetherington G.W., Nelson B.R. Treatment of extramammary Paget disease with topical imiquimod cream: case report and literature review. South Med. J. 2006;99:396–402. doi: 10.1097/01.smj.0000209223.68763.b1. [DOI] [PubMed] [Google Scholar]
- 19.Ximena E., del Puerto C., Mario P., Sergio G. Ectopic extramammary Paget's disease on the face. Indian J. Dermatol. Venereol. Leprol. 2012;78:760–762. doi: 10.4103/0378-6323.102385. [DOI] [PubMed] [Google Scholar]