Abstract
Background
Substance use is prevalent among emergency department (ED) patients, and sex has been implicated as an important factor in the etiology, pathophysiology, sequelae, and treatment of substance use disorders. However, additional information is needed about the epidemiology of substance use as it relates to sex among ED patients.
Objectives
This study examined sex differences in the prevalence and severity of self-reported tobacco, alcohol, and drug use among adult ED patients.
Methods
A random sample of English- or Spanish-speaking, non–critically ill or injured, 18- to 64-year-old patients was approached at two urban EDs and asked to self-report their lifetime and past 3-month tobacco, alcohol, and drug use. Participants completed the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) using an audio computer-assisted self-interview. Participants were categorized by their substance severity (ASSIST score) and need for a brief or more intensive intervention per World Health Organization recommendations. Substance misuse prevalence, frequency, severity, and need for interventions were compared between sexes by substance category. Multivariable logistic regression models were used to examine the association between sexes and the need for intervention after adjusting for sociodemographic characteristics.
Results
Of the 6,432 participants in the study, the median age was 37 years (interquartile range = 26 to 48 years), and 56.6% were female. Overall, lifetime, and past 3-month use was higher for men across all substances (tobacco, alcohol, and drugs). Among those reporting past 3-month use, the frequency of use was similar between sexes for tobacco and all drugs, but men reported more frequent alcohol use. Men had higher mean ASSIST scores compared to women, 30.3 (standard error [SE] ± 0.8) vs. 21.1 (SE ± 0.5); mean difference 9.2 (95% confidence interval [CI] = 7.4 to 10.9). The need for any intervention (brief or intensive) was similar between sexes for tobacco and drugs. After sociodemographic factors were adjusted for, women were less likely than men to need any intervention for alcohol (odds ratio [OR] = 0.6; 95% CI = 0.4 to 0.8), but not other substances: tobacco (OR = 0.9; 95% CI = 0.6 to 1.3), marijuana (OR = 0.8; 95% CI = 0.6 to 1.1), or other drugs (OR = 1.1; 95% CI = 0.7 to 1.7).
Conclusions
Although men have a higher overall prevalence of substance use, the frequency and severity of use were similar for men and women for most substances. After other characteristics were adjusted for, sex appears associated with the need for interventions for alcohol, but not tobacco, marijuana, or other drugs.
Emergency department (ED) patients are more likely than the general population to use and misuse tobacco, alcohol, and drugs.1,2 Among ED patients, the prevalence of tobacco use has been reported to be as high as 48%.2 In 2010, almost one out of every 10 ED visits was directly or indirectly a consequence of alcohol use, a figure that has nearly doubled since 1995.1 In 2011, the Drug Abuse Warning Network (DAWN) estimated that 2.5 million ED visits (approximately 2% to 3% of all visits) were directly due to misuse or abuse of illicit and prescription drugs,3 and approximately 13% of ED patients screened positive for problematic drug use.4
Sex differences have received growing attention as being an important component in the etiology and consequences of substance abuse and dependence.5–8 One large multistate ED study demonstrated that male sex was associated with greater severity of tobacco, alcohol, and drug use, which mirrors what is known about the general population.9 Apart from this study, little is known about sex-specific differences in the patterns of substance use and need for interventions among ED patients. This knowledge deficit about substance use related to sex was highlighted as a research priority at the 2014 Academic Emergency Medicine consensus conference “Gender-Specific Research in Emergency Care.”10
Understanding sex differences may be a pivotal factor in designing effective screening, brief interventions, and referral to treatment (SBIRT) approaches to address substance use among ED patients.11 In the ED, some SBIRT models have been shown to reduce alcohol use and its associated negative consequences, using the reason for the ED visit as a “teachable moment.”12,13 In settings other than EDs, primary care-based SBIRTs have shown differential effects of these approaches between men and women.14 In addition, women generally have been underrepresented in this line of research. As research and clinical implementation of SBIRT expands, there likely will be a role for sex-specific SBIRT trials, particularly if significant differences between sexes in the prevalence, patterns, or severity of substance use exist. Substance abuse may also manifest in variable behaviors between men and women (i.e., social or financial problems), and knowledge of these behaviors might supply important content for interventions and treatment. Additional work is needed to identify sex differences and examine factors that might account for these differences in substance use among ED patients.
The primary aim of this investigation was to determine if sex differences exist in the prevalence of lifetime and past 3-month use of tobacco, alcohol, and drugs among a large random sample of adult ED patients. In addition, we also examined sex differences in: 1) the frequency of tobacco, alcohol, and drug use among those who used these substances within the past 3 months; 2) the severity of substance use within each substance category; 3) the need for interventions (brief or intensive) per World Health Organization (WHO) guidelines to decrease or eliminate substance use; and 4) patterns of substance use associated with the need for intervention.
METHODS
Study Design
This was a retrospective subanalysis of data from two concurrent clinical trials: Brief Intervention for Drug Misuse in the Emergency Department (BIDMED) and Increasing Viral Testing in the Emergency Department (InVITED). This study involved assessing substance misuse prevalence, frequency, and severity among a random sample of adult ED patients conducted over a 30-month period from July 2010 to December 2012. Study recruitment ceased once targeted enrollment was achieved. Data from this current investigation were collected before participants were randomly assigned to treatment or control conditions in the two trials. The study methodology has been previously described in greater detail elsewhere.15,16 Both studies were approved by the participating hospitals’ institutional review boards.
Study Setting and Population
The study sites were two urban academic EDs. One of the sites is a Level I trauma center and the tertiary care referral center for the region; its annual ED census is >100,000 adult visits. The other site is a community hospital ED with an annual ED census of >55,000 adult visits.
A random sample of ED patients was approached and assessed for study eligibility during study enrollment shifts. Enrollment shifts were 8-hour periods from 8:00 AM to 4:00 PM, and 4:00 PM to midnight, 7 days a week when bilingual (English- and Spanish-speaking) research assistants (RAs) were available to conduct the study. We used a computer-based (Random.org) random sampling technique previously employed in our studies to select patients to approach and assess for study eligibility.17 In brief, during the selected enrollment shifts the RA reviewed the electronic medical records of patients randomly selected by their room numbers; those meeting initial eligibility requirements then underwent further in-person assessments to confirm study eligibility. Patients were potentially study eligible if they were 18 to 64 years old, English- or Spanish-speaking, not critically ill or injured, and able to provide informed consent. Patients were excluded if they were known to be pregnant; incarcerated, under arrest, or undergoing home confinement; presenting for acute psychiatric illness; in substance abuse treatment; or clinically intoxicated at the time of screening. Patients deemed clinically sober by their treating physicians were eligible. No financial incentives were provided to participants, and ED staff members were specifically instructed not to encourage, refer, or discourage patients from participating in the study.
Survey Content and Administration
Participants were first asked about their sociodemographic characteristics (age, race/ethnicity, partner status, insurance status, education level, homelessness, employment status, usual source of medical care, and family status) using instruments from previous studies.18 Participants next completed a confidential, audio computer-assisted self-administered interviewer (ACASI)-based assessment of their substance use and misuse using the Alcohol, Smoking and Substance Involvement Screening Test, Version 3 (ASSIST V.3.).19 The WHO has put forth guidelines regarding the need for interventions based on ASSIST scores: it recommends that those who score ≥ 4 points for tobacco or in any drug category, or ≥ 11 points for alcohol, receive a brief intervention and those who score ≥ 27 points in any category receive a more intensive intervention. WHO guidelines do not stratify their intervention recommendations based on sex.
Question 1 of the ASSIST asks about lifetime use of individual substances, and then substance misuse is quantified based on responses to the following six questions. Questions 2 through 7 of the ASSIST can each be mapped to a different subdomain: frequency of use; frequency of cravings; frequency of health, social, legal, or financial problems; frequency of failed obligations; concern expressed by others; and attempts to cut down or quit in the past 3 months. For prescription drugs, participants are told not to report drugs “that are used as prescribed by your doctor,” but to report “medications for reasons other than prescribed, or taken them more frequently or at higher doses than prescribed.” A potential limitation of the ASSIST is that it does not assess quantity of use.
We used a form of the ASSIST that we previously had adapted to an ACASI format and that included expanded drug categories (e.g., barbiturates, benzodiazepines, illicit opioids, gamma-hydroxybutyrate, methadone or buprenorphine, methamphetamines, prescription opioid analgesics).20 This adapted ASSIST underwent standardized cognitive-based assessments verifying participant comprehension of questions, responses, and instructions and was demonstrated to have good internal reliability (Cronbach’s alpha ranged from 0.86 to 0.95).15 Participants completed the study questionnaires in approximately 10 to 15 minutes.
Outcome Measures
We assessed both lifetime and 3-month prevalence of self-reported substance use among ED female and male study participants, which corresponds to questions 1 and 2 of the ASSIST. For participants who reported substance use within the past 3 months, frequency of use also was assessed. Responses to the ASSIST were scored per WHO guidelines to assess severity of substance misuse by substance misuse category (e.g., alcohol, tobacco, and individual drug categories).19 These ASSIST scores also were used to assess the level of intervention needed (none, brief, or intensive) based on WHO guidelines as outlined. Of note, using WHO criteria it is still possible to require a brief intervention with lifetime use only (i.e., no use in the past 3 months, but screen-positive due to self-report of craving). Lastly, we compared the subdomains of the ASSIST (questions 2 through 7) between sexes in attempt to understand differences in behaviors that might lead to needing an intervention.
Data Analysis
Study eligibility assessments and enrollment were summarized using the recommended Consolidated Standards of Reporting Trials (CONSORT) guidelines for reporting data in observational studies.21 Participant sociodemographic characteristics were summarized (proportions or median and interquartile ranges) by sex. The prevalence of lifetime and past 3-month use of alcohol, tobacco, and drugs were calculated. Among those who reported past 3-month use, frequency of use for each substance category (alcohol, tobacco, and individual drug categories) was calculated. ASSIST scores (mean, standard error [SE]) for each substance category, and for all drugs combined, were calculated. The proportions of participants needing brief interventions or more intensive interventions (per WHO recommendations based on ASSIST scores) for each substance category were stratified by those who reported lifetime use only or past 3-month use.
Sex differences in sociodemographic characteristics, prevalence, frequency, severity, and the need for intervention were compared using Wilcoxon’s test for continuous variables and chi-square or Fisher’s exact test for categorical variables, as appropriate. Student’s t-test was not used because many continuous variables (e.g., drug use frequencies) are highly skewed. Multivariable logistic regression was used to determine the association between sex and the need for an intervention for each substance category. Likelihood ratio testing was used to determine the final logistic model by comparing nested models (α = 0.05); age, ethnicity, education, employment status, homelessness, and the presence of child under 17 years old living in the home were included in the final model, as well as interaction terms between age and sex and the presence of child under 17 years old living in the home and sex. The Hosmer-Lemeshow test was used to examine the goodness of fit of the multivariable models.
Finally, to explore differences in patterns of substance use and need for intervention between sexes, an analysis of the ASSIST by subdomain was performed. For each substance, we calculated the mean score ASSIST score and associated 95% confidence intervals (CIs) by question for each sex to determine if sex differences existed within each subdomain.
RESULTS
Participant Recruitment, Enrollment, and Sociodemographic Characteristics
The results of participant recruitment and enrollment are depicted in Figure 1. Sociodemographic characteristics of both sexes are presented in Table 1; 57% of participants were women (n = 3,639). Overall, more men than women had lower levels of education, were homeless, and cited the ED as their source of usual medical care. A higher proportion of women were Hispanic and insured and reported living with a child ≤ 17 years old in the home.
Figure 1.
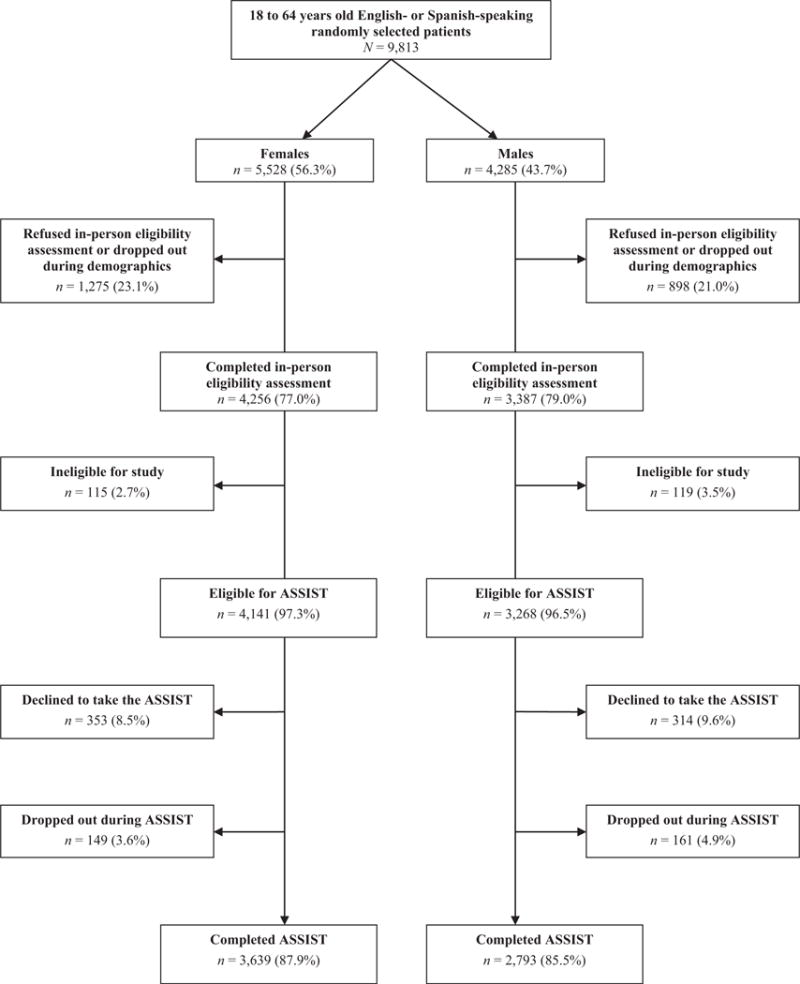
Eligibility assessment and enrollment flow diagram.
Table 1.
Demographic Characteristics of Participants by Sex
| Demographic Characteristics | Male (n = 2,793) | Female (n = 3,639) | Mean Difference (95% CI) |
|---|---|---|---|
| Age (yr), median (IQR) | 38 (27–49) | 36 (25–48) | 1.2 (0.6 to 1.9) |
| Ethnicity/race | |||
| White, non-Hispanic | 62.9 | 60.6 | 2.3 (−0.4 to 5) |
| White, Hispanic | 9.6 | 12.5 | −2.9 (−4.5 to −1.4) |
| Black/African American, non-Hispanic | 17.3 | 17.3 | 0.0 (−0.1 to 0.1) |
| Black/African American, Hispanic | 6.9 | 6.2 | −0.7 (−0.9 to 0.1) |
| Other | 3.1 | 3.5 | −0.4 (−0.9 to 0.1) |
| Education completed | |||
| Some high school | 27.9 | 23.8 | 4.1 (1.9 to 6.2) |
| High school | 32.4 | 27.9 | 4.5 (2.3 to 6.8) |
| Some college | 22.8 | 30.1 | −7.3 (−9.4 to −5.1) |
| College graduate | 16.9 | 18.2 | −1.3 (−3.2 to 0.6) |
| Health insurance | |||
| Private | 39.8 | 41.6 | −1.3 (−3.7 to 1.1) |
| Governmental | 27.5 | 38.9 | −11.5 (−13.8 to −9.2) |
| None | 32.6 | 19.4 | 13.1 (11 to 15.3) |
| Partner status | |||
| Married | 28.3 | 27.6 | 0.7 (−1.5 to 2.9) |
| Divorced/widowed/separated | 15.7 | 19.6 | −4 (−5.9 to −2.1) |
| Never married | 40.3 | 37.6 | 2.7 (0.3 to 5.1) |
| Unmarried couple | 15.7 | 15.1 | 0.6 (−1.2 to 2.4) |
| Homeless | |||
| Currently homeless | 7.3 | 4.2 | 3.1 (2 to 4.3) |
| Homeless in past 12 months | 3.0 | 3.1 | 0.0 (−0.8 to 0.9) |
| Never/not homeless past 12 months | 89.6 | 92.8 | −3.1 (−5 to −1.2) |
| Employment status | |||
| Employed | 51.0 | 47.1 | 3.7 (1.2 to 6.2) |
| Disabled | 17.5 | 18.4 | −0.9 (−2.8 to 1) |
| Student | 6.2 | 9.9 | −3.7 (−5.1 to −2.3) |
| Unemployed | 25.2 | 24.5 | 0.1 (−2 to 2.2) |
| Usual source of medical care | |||
| Private clinic/practice | 41.4 | 50.2 | −8.8 (−11.2 to −6.1) |
| Hospital or community health clinics | 20.8 | 30.3 | −9.6 (−11.7 to −7.5) |
| Emergency department | 34.9 | 17.1 | 17.8 (15.7 to 19.9) |
| Urgent care center | 2.6 | 2.3 | 0.3 (−0.5 to 1) |
| Lives with a minor child in the home | 58.4 | 68.4 | −9.7 (−12 to −7.3) |
Categorical data are presented as proportion (%). Mean difference: males – females.
IQR = interquartile range.
Substance Use/Misuse Differences by Sex
The prevalence of lifetime and past 3-month substance use among men and women is displayed in Table 2. Across all substances (tobacco, alcohol, and all drugs combined), men had a higher prevalence of lifetime and past 3-month substance use. When assessing the prevalence of use of specific drugs, men reported greater use than women of all drugs except for benzodiazepines within the past 3 months. For both sexes, the prevalence of past 3-month use was greatest for alcohol, followed by tobacco, marijuana, prescription opioids, and cocaine (in descending order of prevalence). Both sexes had a prevalence of less than 4% for use of all other drug categories.
Table 2.
Prevalence of Lifetime and Past 3-month Substance Use
| Specific Substances | Lifetime
|
Past 3 Months
|
||||
|---|---|---|---|---|---|---|
| Male | Female | Mean Difference (95% CI) | Male | Female | Mean Difference (95% CI) | |
| Tobacco (smoking) | 72.8 | 61.2 | 11.6 (9.3 to 13.8) | 50.0 | 39.1 | 10.8 (8.3 to 13.4) |
| Alcohol | 91.1 | 83.6 | 7.6 (6.0 to 9.1) | 57.3 | 47.7 | 10.3 (8.0 to 12.7) |
| Drugs | ||||||
| Marijuana | 69.9 | 52.7 | 17.1 (14.9 to 19.5) | 33.9 | 21.2 | 12.6 (10.4 to 14.9) |
| Cocaine or crack | 32.0 | 18.7 | 13.4 (11.2 to 15.5) | 7.9 | 4.2 | 3.6 (2.4 to 4.7) |
| Prescription opioids | 18.9 | 11.8 | 7.1 (5.3 to 8.9) | 8.1 | 5.1 | 2.9 (1.8 to 4.1) |
| Hallucinogens | 23.0 | 10.7 | 12.4 (10.6 to 14.3) | 1.9 | 0.8 | 1.2 (0.6 to 1.7) |
| Benzodiazepines | 11.6 | 8.3 | 3.3 (1.8 to 4.8) | 3.8 | 3.5 | 0.4 (−0.5 to 1.4) |
| Methamphetamines | 12.5 | 7.9 | 4.6 (3.1 to 6.1) | 2.2 | 1.1 | 1.1 (0.5 to 1.7) |
| Opioids | 12.0 | 5.6 | 6.4 (5.0 to 7.8) | 3.4 | 1.5 | 1.9 (1.1 to 2.7) |
| Amphetamines | 7.6 | 5.1 | 2.7 (1.3 to 3.9) | 1.9 | 1.6 | 0.3 (−0.4 to 1.0) |
| Inhalants | 8.0 | 3.7 | 4.3 (3.2 to 5.5) | 1.1 | 0.3 | 0.8 (0.4 to 1.2) |
| Methadone or buprenorphine | 4.6 | 2.1 | 2.5 (1.5 to 3.4) | 2.0 | 0.8 | 1.2 (0.7 to 1.8) |
| Gamma-hydroxybutyrate | 2.4 | 1.0 | 1.5 (0.8 to 2.1) | 0.3 | 0.1 | 0.2 (0.0 to 0.5) |
| Barbiturates | 2.1 | 1.0 | 1.7 (0.4 to 1 to 0) | 0.4 | 0.2 | 0.2 (0.0 to 0.4) |
| All drugs | 47.5 | 32.3 | 15.2 (12.8 to 17.5) | 42.4 | 28.3 | 14.0 (11.7 to 16.3) |
Data are presented as a proportion (%). Mean difference: males – females.
The frequency of use for participants who reported substance use within the past 3 months is shown in Table 3. Frequency of tobacco use was similar between sexes, although greater proportions of men compared to women reported daily to near-daily use of alcohol (5 to 7 days/week). Nearly one-third of men and women who used marijuana in the past 3 months reported daily to near-daily use, although this proportion was somewhat higher in men (39% vs. 32%). A greater proportion of women reported daily to near-daily use of cocaine, whereas men reported greater use of methamphetamines. Frequency of use of other specific drugs was similar between sexes.
Table 3.
Frequency of Use Among Participants Reporting Use in the Past 3 Months
| Specific Substances | Past 3-month Use |
5 to 7 Days per Week
|
1 to 4 Days per Week
|
Once or Twice in the Past Month
|
Once or Twice in the Past 3 Months
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Females (n) |
Males (n) |
Female (%) |
Male (%) |
Mean Difference (95% CI) |
Female (%) |
Male (%) |
Mean Difference (95% CI) |
Female (%) |
Male (%) |
Mean Difference (95% CI) |
Female (%) |
Male (%) |
Mean Difference (95% CI) |
|
| Tobacco (smoking) | 1,423 | 1,397 | 75 | 75 | −0.4 (−3.5 to 3) | 11.8 | 12.5 | 0.8 (1.8 to 3) | 5.3 | 6.2 | 0.9 (−0.8 to 2.7) | 7.7 | 6.5 | −1.2 (−3.1 to 0.6) |
| Alcohol | 2,085 | 1,332 | 7 | 14 | 6.8 (4.9 to 8.6) | 26.3 | 36.9 | 10.6 (7.8 to 13.3) | 32.6 | 27.3 | −5.4 (−8.1 to −2.7) | 33.8 | 21.7 | −12.2 (−15.2 to −9.4) |
| Drugs | ||||||||||||||
| Marijuana | 771 | 947 | 32 | 39 | 6.6 (2 to 10.9) | 26.3 | 25.4 | −0.9 (−4.9 to 3.3) | 17.2 | 17.0 | −0.1 (−4 to 3.2) | 24.4 | 18.9 | −5.5 (−9.6 to −1.4) |
| Cocaine or crack | 153 | 221 | 22 | 12 | −9.8 (−17.7 to −2.7) | 12.4 | 19.6 | 7.2 (−0.1 to 14.8) | 28.8 | 28.3 | −0.4 (−10 to 9.3) | 36.6 | 39.7 | 3.0 (−6.3 to 13.2) |
| Prescription opioids | 186 | 226 | 22 | 17 | −4.8 (−12.2 to 2.9) | 24.5 | 30.9 | 6.5 (−2.5 to 14.6) | 25.5 | 24.2 | −1.5 (−9.5 to 7.6) | 27.7 | 27.4 | −0.4 (−9.4 to 8) |
| Hallucinogens | 29 | 53 | 4 | 13 | 9.5 (−1.8 to 21.2) | 7.4 | 5.7 | −1.6 (−14.9 to 9) | 22.2 | 20.8 | −2.1 (−21.3 to 16.5) | 66.7 | 60.4 | −6.4 (−30.1 to 18.8) |
| Benzodiazepines | 127 | 106 | 23 | 16 | −7.5 (−17.6 to 2.9) | 21.6 | 29.0 | 7.1 (−3.5 to 19.2) | 20.0 | 23.4 | 3.6 (−7.7 to 14.4) | 35.2 | 31.8 | −3.6 (−16.1 to 8.8) |
| Methamphetamines | 40 | 61 | 5 | 13 | 8.2 (2.7 to 17.6) | 10.0 | 14.8 | 4.5 (−9.3 to 17.6) | 37.5 | 18.0 | −19.3 (−36.9, −2.4) | 47.5 | 54.1 | 7.0 (−14.7 to 27.4) |
| Opioids | 55 | 95 | 31 | 28 | 2.5 (−18.5 to 13.2) | 20.0 | 29.5 | 9.3 (−5.8 to 23.9) | 23.6 | 14.7 | −9 (−23.5 to 4.5) | 25.5 | 27.4 | 1.9 (−11.8 to 16.5) |
| Amphetamines | 58 | 53 | 5 | 13 | 8.2 (−2.9 to 19.7) | 29.8 | 21.2 | −9 (−25 to 7.8) | 26.3 | 25.0 | −1 (−18.2 to 15.3) | 38.6 | 40.4 | 1.9 (−15.4 to 20.6) |
| Inhalants | 11 | 31 | 36 | 13 | −23.1 (−58.5 to 7.9) | 0.0 | 20.0 | 20 (7.7 to 36) | 18.2 | 20.0 | 1.9 (−27.4 to 27.3) | 45.5 | 46.7 | 1.2 (−36.7 to 33.7) |
| Methadone/buprenorphine | 29 | 56 | 26 | 25 | −0.4 (−22.4 to 18.6) | 18.5 | 27.3 | 9 (−10.1 to 27.6) | 22.2 | 23.6 | 1.5 (−19.7 to 21.5) | 33.3 | 23.6 | −10.7 (−33.3 to 12.9) |
| Gamma-hydroxybutyrate | 4 | 8 | 50 | 25 | −25 (−75 to 50) | 0.0 | 12.5 | −12.5 (0 to 0) | 0.0 | 25.0 | 25 (0 to 0) | 50.0 | 37.5 | −4.6 (−85.7 to 0) |
| Barbiturates | 7 | 11 | 17 | 20 | 3.3 (−46.6 to 40) | 16.7 | 30.0 | 14.8 (−42.9 to 58.3) | 16.7 | 0.0 | −16.7 (0 to 0) | 50.0 | 50.0 | 0.0 (−54.2 to 51.9) |
Rows do not sum to 100% because of nonresponders. Mean difference to males – females.
Overall, men had higher average ASSIST scores for tobacco, alcohol, and all drugs combined. However, for individual drug components, men and women had similar severities of use as measured by ASSIST scores. Data Supplement S1 (available as supporting information in the online version of this paper) displays mean ASSIST scores, a marker of severity of substance use, for men and women by substance category.
Overall, the need for any intervention was similar between sexes (Data Supplement S2, available as supporting information in the online version of this paper), with a few exceptions. Men who ever smoked (lifetime prevalence) were more likely to need brief interventions than women, but the need for intervention was similar among those who smoked within in the past 3 months. More men than women with alcohol use in the past 3 months required both brief and intensive interventions. The need for intervention by drug category was largely the same between sexes; only women required fewer brief interventions for marijuana and fewer intensive interventions for gamma-hydroxybutyrate.
In the multivariable logistic model adjusting for sociodemographic characteristics (Data Supplement S3, available as supporting information in the online version of this paper), women were less likely than men to need any intervention for alcohol (odds ratio [OR] = 0.6; 95% CI = 0.4 to 0.8), but not other substances: tobacco (OR = 0.9; 95% CI = 0.6 to 1.3), marijuana (OR = 0.8; 95% CI = 0.6 to 1.1), or other drugs (OR = 1.1; 95% CI = 0.7 to 1.7).
Analysis of the subdomains of the ASSIST by substance between sexes demonstrated several areas of discrepancy between men and women (Data Supplement S4, available as supporting information in the online version of this paper). For alcohol and marijuana use, men had higher ASSIST scores across all subdomains. Men had higher ASSIST scores for frequency of use and reported more health, social, legal, or financial problems compared to women concerning tobacco use. Women reported more frequent urges to use benzodiazepines than men, whereas men reported more failed obligations and health, social, legal, or financial problems related to methamphetamine use. Subdomains for the remaining drug categories were similar between sexes.
DISCUSSION
In this large study of adult ED patients not seeking treatment for or undergoing evaluation for substance use, a substantial proportion of men and women reported tobacco, alcohol, and/or drug use. Alcohol, tobacco, and drug use was more prevalent overall among men compared with women. This observation was apparent for both lifetime and past 3-month use, with one exception that the past 3-month use of benzodiazepines was greater among women. This finding is in concert with a substantial body of outpatient and population-based studies that suggest substance use is more common among men.5 In addition, in agreement with previously published work, ED patients of both sexes also report more tobacco, alcohol, and drug use than previously published national averages.9,22
Among those in our sample who reported drug use within the past 3 months, the most commonly reported substances for both sexes (in descending order) were alcohol, tobacco, marijuana, prescription opioids, and cocaine. These findings are interesting because men and women are using the same types of substances. Since ED-based screening and interventions are often substance-specific, this provides insight into what specific substances should be targeted and suggests that men and women be screened for similar substances. It is important to note, however, that this may reflect local differences in patterns of use. Although this observation is similar to a recent multicenter study, patterns of substance use may vary geographically and our study findings may not be generalizable to other areas of the country.9
When marijuana is not included, the most common drug used in the past 3 months for either sex was prescription opioids. Prescription opioid use was still more common among men, despite the fact that women are more likely to use prescription opioids and receive opioids in higher doses.23,24 Equal numbers of men and women also have ED visits related to prescription opioids.25 A possible explanation for this discrepancy with our study findings is that women might not identify prescription opioids as drugs being misused based on the ASSIST screening instrument. This observation highlights a gap in knowledge; it is not yet known how current means of detecting substance use differs between sexes. It is possible that sex-specific screening for substance use is warranted, and this is a needed area of further study.
Although women in our ED-based sample had less prevalent substance use than men, the frequency and severity of use were similar to their male counterparts for tobacco and most individual drug categories. This finding supports recent work that found a similar pattern of substance use and suggests that substance-using women are as just as prone to problematic behavior as substance using men.9 In fact, it is plausible that women should have lower cutoffs for what constitutes problematic behavior or positive screens for misuse and need for treatment. It is well known that sex differences in body composition, physiology, and metabolism may make women more prone to the negative sequelae of substance use at lower levels of use than their male counterparts.8,10 Therefore, women who use substances at the same frequency and severity as men, may be placing themselves at higher risk for consequences.17 For example, at similar levels of alcohol consumption, women have a greater risk of developing liver cirrhosis than men.26
In the multivariable analyses, after adjusting for sociodemographic characteristics, women had a 44% lower likelihood of needing an intervention for alcohol. This estimate would almost certainly change if a lower sex-specific cutoff were employed. Future work should investigate the impact of sex-specific lower screening thresholds and its effect on patient-centered outcomes. Of interest, estimates for needing an intervention were similar between sexes for tobacco and drugs. Despite this similar need for intervention, previous work has demonstrated that women are less likely to be involved in treatment programs.27 That observation may mean that women are not adequately being identified as having a problem with substances or that they are not being referred to treatment.
Men had higher overall ASSIST scores for all drugs combined, but not for individual drug categories. A possible explanation for this finding is that men may have more polydrug problems than women, a behavior that may be important for the content of interventions. In addition, the analysis of the subdomains of the ASSIST may be useful in generating sex-specific SBIRT content. There were differences between sexes, but this also varied by substance. This suggests that SBIRT content may need to be not only sex-specific, but substance-specific as well. For example, women noted more cravings than men with regard to benzodiazepine use, but more men noted health, social, legal, or financial problems with methamphetamine use. These differences in why men and women needed an intervention on screening highlight that further work is needed to really understand sex-specific motivations to initiate and continue substance use.
This study is also of direct clinical relevance. It further highlights that ED patients of both sexes have prevalent substance use problems and that there is high burden of substance use needs among ED patients. Substance use should not be viewed as a male problem; clinicians should have a low threshold to screen for substance use disorders among both men and women in the ED, with referral to treatment when indicated. There is also an unmet need to examine ED-based substance use resources for both sexes from perspectives of research, clinical care, and policy.
LIMITATIONS
Although measures were taken to include a representative sample of adult ED patients at the two study sites, some patients were inevitably excluded (i.e., presented to the ED when data were not collected, spoke languages other than English or Spanish, or met exclusion criteria), and those excluded might have had different substance use/misuse profiles and need for interventions. In particular, study recruitment did not occur between midnight and 8 AM, a time when individuals with substance abuse related visits often present to the ED. In addition, the ASSIST might not identify all patients with substance use problems. For example, the ASSIST does not assess quantity of use and may miss individuals with problematic binge-type behavior who would not otherwise screen positive. The outcome measures were based on self-reported substance use and thus subject to recall or social desirability biases. However, use of the ACASI approach and other means to ensure privacy probably helped to ensure confidentiality, likely decreasing social desirability bias. Regardless, if such biases did exist, they would likely underestimate the magnitude of the problem. Last, the study did not explore risks factors or motivations for substance use between sexes, which might be an important component of interventions and treatment. Further work should be done in this area.
CONCLUSIONS
Although men have a higher overall prevalence of substance use, the frequency and severity of use were similar between sexes for most substances. After other characteristics are adjusted for, sex appears associated with the need for intervention for alcohol, but not tobacco, marijuana, or other drugs. There are also sex differences in why men and women needed intervention. Future work should seek to understand sex-specific risk factors for substance use and explore the utility of sex-specific screening and intervention.
Supplementary Material
Data Supplement S1. Assist scores by substance category for participants reporting any lifetime use.
Data Supplement S2. WHO recommendations for interventions by substance to men versus women.
Data Supplement S3. Odds of needing an intervention for women compared to men by level of intervention.
Data Supplement S4. Analysis of the subdomains of the ASSIST by substance between sexes demonstrating several areas of discrepancy between men and women. Error bars correspond to 95% confidence intervals; a p-value <0.05 is denoted by an asterisk (*).
Acknowledgments
Funding for this study was supported by R01 DA026066 (BIDMED) and R01 DA026066 (InVITED).
Dr. Merchant, an associate editor for this journal, had no role in the peer-review process or publication decision for this manuscript.
Footnotes
Presented at the Society for Academic Emergency Medicine Annual Meeting, San Diego, CA, May 2015.
The authors have no conflicts of interest to disclose.
Supervising Editor: Mark Mycyk, MD.
Supporting Information
The following supporting information is available in the online version of this paper.
References
- 1.Cherpitel CJ, Ye Y. Trends in alcohol- and drug-related emergency department and primary care visits: data from four U.S. national surveys (1995–2010) J Stud Alcohol Drugs. 2012;73:454–8. doi: 10.15288/jsad.2012.73.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lowenstein SR, Koziol-McLain J, Thompson M, et al. Behavioral risk factors in emergency department patients: a multisite survey. Acad Emerg Med. 1998;5:781–7. doi: 10.1111/j.1553-2712.1998.tb02504.x. [DOI] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 4.Konstantopoulos WL, Dreifuss JA, McDermott KA, et al. Identifying patients with problematic drug use in the emergency department: results of a multisite study. Ann Emerg Med. 2014;64:516–25. doi: 10.1016/j.annemergmed.2014.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zilberman M, Tavares H, el-Guebaly N. Gender similarities and differences: the prevalence and course of alcohol- and other substance-related disorders. J Addict Dis. 2003;22:61–74. doi: 10.1300/j069v22n04_06. [DOI] [PubMed] [Google Scholar]
- 6.Tetrault JM, Desai RA, Becker WC, Fiellin DA, Concato J, Sullivan LE. Gender and non-medical use of prescription opioids: results from a national US survey. Addiction. 2008;103:258–68. doi: 10.1111/j.1360-0443.2007.02056.x. [DOI] [PubMed] [Google Scholar]
- 7.Sugarman DE, Demartini KS, Carey KB. Are women at greater risk? An examination of alcohol-related consequences and gender. Am J Addict. 2009;18:194–7. doi: 10.1080/10550490902786991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clin Psychol Rev. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Sanjuan PM, Rice SL, Witkiewitz K, Mandler RN, Crandall C, Bogenschutz MP. Alcohol, tobacco, and drug use among emergency department patients. Drug Alcohol Depend. 2014;138:32–8. doi: 10.1016/j.drugalcdep.2014.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choo EK, Beauchamp G, Beaudoin FL, et al. A research agenda for gender and substance use disorders in the emergency department. Acad Emerg Med. 2014;21:1438–46. doi: 10.1111/acem.12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cunningham RM, Bernstein SL, Walton M, et al. Alcohol, tobacco, and other drugs: future directions for screening and intervention in the emergency department. Acad Emerg Med. 2009;16:1078–88. doi: 10.1111/j.1553-2712.2009.00552.x. [DOI] [PubMed] [Google Scholar]
- 12.Sommers MS, Lyons MS, Fargo JD, et al. Emergency department-based brief intervention to reduce risky driving and hazardous/harmful drinking in young adults: a randomized controlled trial. Alcohol Clin Exp Res. 2013;37:1753–62. doi: 10.1111/acer.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Academic ED SBIRT Research Collaborative. The impact of screening, brief intervention and referral for treatment in emergency department patients’ alcohol use: a 3-, 6- and 12-month follow-up. Alcohol Alcohol. 2010;45:514–9. doi: 10.1093/alcalc/agq058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007:CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Merchant RC, Baird JR, Liu T, Taylor LE, Montague BT, Nirenberg TD. Brief intervention to increase emergency department uptake of combined rapid human immunodeficiency virus and hepatitis C screening among a drug misusing population. Acad Emerg Med. 2014;21:752–67. doi: 10.1111/acem.12419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merchant RC, Baird JR, Liu T, Taylor LE. HCV among The Miriam Hospital and Rhode Island Hospital Adult ED Patients. RI Med J. 2014;97:35–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Trillo AD, Merchant RC, Baird JR, Liu T, Nirenberg TD. Sex differences in alcohol misuse and estimated blood alcohol concentrations among emergency department patients: implications for brief interventions. Acad Emerg Med. 2012;19:924–33. doi: 10.1111/j.1553-2712.2012.01408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merchant RC, Seage GR, Mayer KH, Clark MA, DeGruttola VG, Becker BM. Emergency department patient acceptance of opt-in, universal, rapid HIV screening. Pub Health Rep. 2008;123(Suppl 3):27–40. doi: 10.1177/00333549081230S305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Humeniuk R, Ali R. Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and pilot brief intervention: a technical report of phase II findings of the WHO ASSIST Project. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 20.Youmans Q, Merchant RC, Baird JR, Langan TJ, Nirenberg T. Prevalence of alcohol, tobacco and drug misuse among Rhode Island hospital emergency department patients. Med Health RI. 2010;93:44–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Schulz KE, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001;357:1191–4. [PubMed] [Google Scholar]
- 22.Grucza RA, Abbacchi AM, Przybeck TR, Gfroerer JC. Discrepancies in estimates of prevalence and correlates of substance use and disorders between two national surveys. Addiction. 2007;102:623–9. doi: 10.1111/j.1360-0443.2007.01745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frenk SM, Porter KS, Paulozzi LJ. Prescription opioid analgesic use among adults: United States, 1999–2012. NCHS Data Brief. 2015;189:1–8. [PubMed] [Google Scholar]
- 24.Campbell CI, Weisner C, Leresche L, et al. Age and gender trends in long-term opioid analgesic use for noncancer pain. Am J Pub Health. 2010;100:2541–7. doi: 10.2105/AJPH.2009.180646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choo EK, Douriez C, Green T. Gender and prescription opioid misuse in the emergency department. Acad Emerg Med. 2014;21:1493–8. doi: 10.1111/acem.12547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rehm J, Taylor B, Mohapatra S, et al. Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev. 2010;29:437–45. doi: 10.1111/j.1465-3362.2009.00153.x. [DOI] [PubMed] [Google Scholar]
- 27.Greenfield SF, Brooks AJ, Gordon SM, et al. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Assist scores by substance category for participants reporting any lifetime use.
Data Supplement S2. WHO recommendations for interventions by substance to men versus women.
Data Supplement S3. Odds of needing an intervention for women compared to men by level of intervention.
Data Supplement S4. Analysis of the subdomains of the ASSIST by substance between sexes demonstrating several areas of discrepancy between men and women. Error bars correspond to 95% confidence intervals; a p-value <0.05 is denoted by an asterisk (*).


