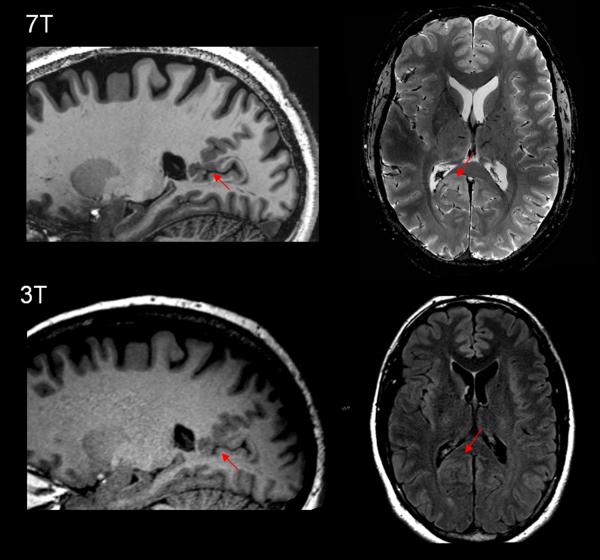
Figure 2.
Example of a subtle polymicrogyria/FCD lesion missed by 3T MRI but detected by 7T MRI. Upper row: 7T (MAGNETOM 7T, Siemens) T1w MP2RAGE sequence (left and middle) and T2*w GRE (right). Bottom row: T1w MPRAGE sequence (left and middle) and 3T (SKYRA 3T, Siemens) axial T2w FLAIR (right) from standard epilepsy protocol. The patient is a 37 year-old right-handed male being evaluated for epilepsy surgery, with seizure onset when he was 16. His seizures starts with an aura of feeling hot and dizzy and deja vu, then seizures were complex motor characterized by holding his head, chewing automatism, lip movements, weird hand motions and deep gasping breaths. Postictally he was amnesic and confused. Frequency was cluster of up to 10/day. His 3T MRI did not show any epileptic abnormalities. On 7T MRI T1w MP2RAGE sequence, it was shown that there was likely MCD and possibly PMG at the depth of the parietal occipital fissure, superior to isthmus (first column, arrow). The lesion showed asymmetric signal hyperintensity particularly on axial T2w GRE (second column, arrow). Guided by the 7T finding, we were able to find correlates on the 3T images, but with less conspicuity and only on the exact same slice. This patient is currently undergoing pre-surgical evaluation which will include invasive evaluation to investigate the epileptogenicity of the lesion.