Abstract
Haematopoietic cell transplants are done by more than 1500 transplant centres in 75 countries, mostly for life-threatening haematological disorders. However, transplant technology and access are not uniformly-distributed worldwide. Most transplants are done in predominately Europe, North America and some Asian countries. We review transplants activity in Latin America, a geographic region with a population of more than 600 million persons living in countries with diverse economic and social development levels. The data indicate a 20-40-fold lower frequency of transplants in Latin America compared with Europe and North America. We show that although economics, infrastructure and expertise are important limitations, other variables also operate. Changes in several of these variables may substantially increase transplant activity in Latin America.
Introduction
Haematopoietic Cell Transplants
Haematopoietic cell transplants are increasingly done to treat diverse severe haematological diseases, mostly leukaemias, lymphomas and plasma cell myeloma. Other transplant indications include bone marrow failure, autoimmune diseases and rare genetic and/or hereditary disorders. More than one million transplants have been done worldwide since 1956, predominately in Europe, North America a and some Asian countries1. The basic strategy is to give high-dose anti-cancer drugs and/or radiation to eradicate the neoplasm or abnormal cells. This is followed by an infusion of haematopoietic cells (termed a graft) to restore normal bone marrow function. There are several important transplant-related variables. For example, the donor can be an HLA-identical sibling or a partially- or completely-HLA-matched relative or unrelated person. These transplants are termed allotransplants. When the recipient's own bone marrow or blood cells are used the procedure is termed an autotransplant. There are also different graft sources such as bone marrow cells, blood cells and umbilical cord blood cells. Recently lower doses of drugs and/or radiation are being given before an allotransplant. This strategy is referred to as a reduced-intensity transplant. As we will discuss, several of these variables enormously impact the rate of diffusion of transplant technology into Latin America.
Economic and Social Aspects of Latin America
Latin America is a large area of 26 sovereign countries covering 19,197,000 km × E+2 or about 15 percent of the Earth's land surface area. The 2015 estimated population is about 610 million, 10 percent of the world population. Several countries such as Brazil and Mexico are enormous with populations exceeding 100-200 million persons. Other countries such as Panama and Uruguay are small with populations less than 4 million.
Added to this geographic and population diversity is tremendous economic heterogeneity including developed and developing countries. b For example, according to the International Monetary Fund (IMF) although the nominal gross domestic product (GDP) c of Latin America is about $6,000,000 million USD it ranges from Brazil at about $2,400,000 million USD to Dominica at $500 million USD, a more than 5000-fold difference. Per capita nominal GDP is equally heterogeneous ranging from $11,000-$14,000 USD (Argentina, Brazil, Chile and Mexico) to $800 USD (Haiti). For comparison, per capita nominal GDP in Norway is almost $100,000 USD and in the US about $55,000 USD. Adjusted per capita GDPs range from $14,000-$19,000 USD for Argentina, Brazil, Chile and Mexico to about $4,500 USD for Nicaragua and Haiti. Comparable figures for the US and UK are $53,000 USD and $36,000 USD. Finally per capita GDP at purchasing power parity (PPP) adjusted for cost of living ranges from about $32,000 USD in some Caribbean countries to $16,000-$23,000 USD for the larger Latin American countries (Argentina, Brazil, Chile and Mexico) to $7,700 USD (Guyana). Comparable figures for Norway and the US are $67,000 USD and $55,000 USD. Put otherwise, even the wealthiest Latin American countries have only about 30 percent of the purchasing power parity per capita for health care outside the national health care system than some European countries with somewhat similar health care systems. Comparison with US figures is more complex because of the private component of much of the US health care system. However, Latin American residents seeking health care outside a governmental health care system have on average only 30 percent of the purchasing power of US residents.
The Human Development Index (HDI) of the United Nations Human Development Program is another measure of social and economic progress. HDI scores for Latin America range from 0.82 for Argentina (very high human development; world rank 49) to 0.46 for Haiti (medium human development; world rank 168).
Another variable to consider is the equality or inequality of income distribution. This is usually measured by Gini coefficient where a value of 0 indicates perfect equality (everyone has the same income) versus a value of 100 indicating maximum inequality (one person has all the countrie's income and everyone else has no income). d Gini coefficients for most European and North American countries are 20-35 whereas Gini coefficients for Latin American countries are typically greater than 40-50. However, it is important to distinguish the income Gini coefficient from the wealth Gini coefficient. The latter describes how wealth, not income, is distributed. Most Latin American countries fall somewhere between the UK (60) and the US (80). Percent GDP invested in healthcare in Latin America ranges from 5-9 percent but with very different proportions of public versus private expenditures in different countries. (Comparable proportions for the US and UK are 19 and 10 percent). As we shall see these disparities substantially impact diffusion of transplant technology in Latin America.
The Social Progress Index is another multiple dimension measure of social progress which included basic medical needs. And although access to transplant cannot be considered a basic medical need, diffusion of high technology medicine often parallels social progress in other spheres. At baseline the Latin American region ranks 2nd globally after Europe/North America/Oceania in providing nutrition and basic medical needs. However, in the 2015 ranking adjusted for per capital GDP, 5 of the 15 countries with the greatest social progress are in Latin America: Costa Rica, Uruguay, Nicaragua, Jamaica, and Chile. This is encouraging.
Finally, period life expectancy at birth is another composite measure of health. Again, the range for Latin American countries is huge: 50-55 years (Trinidad and Tobago) to more than 80 years (Costa Rica). For the most populous countries it ranges between 70-73 years (Brazil), 70-78 years (Argentina) and 76-79 years (Mexico). As a group, Latin America ranks 2nd after the most developed countries in period life expectancy at birth according to the UN World Population Prospects 2008.
Transplants in Latin America
The first bone marrow transplants in Latin America were done in the 1970s. Since then many countries started or expanded transplant programs and today some are large and well-developed. A precise estimate of transplant activity (sometimes referred to as volume or intensity) is difficult for several reasons including: (1) heterogeneity of countries, health authorities and payors; (2) inconsistent reporting to national, regional and international agencies; (3) diversity of programme types and leaders and other variables. We used data from the Center for International Blood and Marrow Transplant Research (CIBMTR), an international voluntary reporting organization covering 462 transplant centres in 50 countries with participation of 49 transplant centres in 9 Latin American countries (Argentina, Brazil, Chile, Colombia, Mexico, Panama, Peru, Uruguay and Venezuela) with detailed and audited reporting to estimate transplant activity. Reports of transplants to the CIBMTR are mandatory in the US but not in Latin American countries such that under-reporting from Latin America is probable.
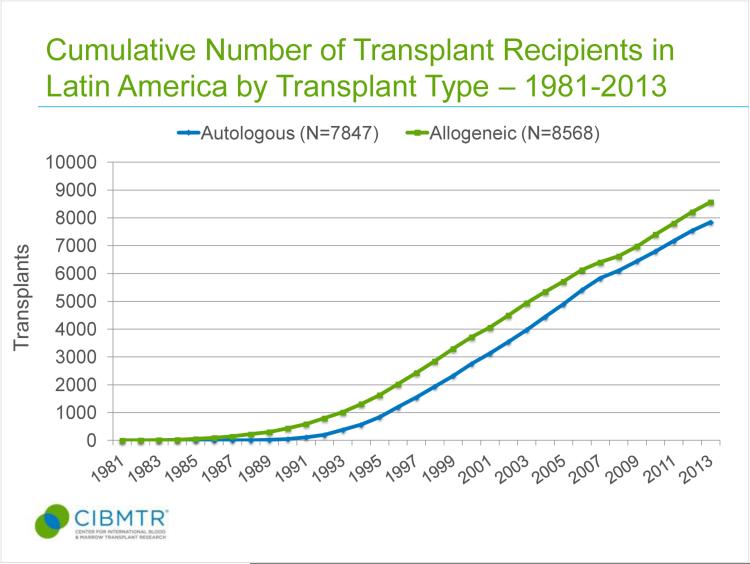
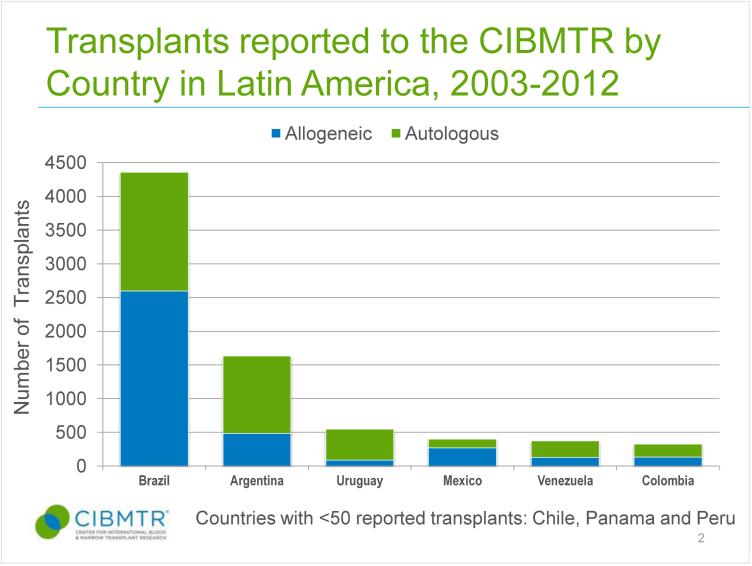
Figure 1 shows cumulative numbers of transplants reported to CIBMTR 1981-2013 from Latin America which exceed 16,000 including roughly equal numbers of autotransplants (N=7847) and allotransplants (N=8568). e In 2003-2013 there were reports of 7783 transplants (Figure 2). Although the ratio of auto- to allotransplants was about 0.8 overall this was not so when we studied different countries. For example, autotransplants predominated in Argentina, Columbia, Uruguay and Venezuela whereas allotransplants predominated in Brazil and Mexico. In 2012 there were about 400 autotransplants and about 500 allotransplants. This ratio of autotransplants to allotransplants is substantially lower than the 1.3 ratio of autotransplants to allotransplants in North America. This skewing reflects a relatively greater deficiency of allotransplants rather than an excess of autotransplants. The 900 autotransplants reported for an estimated 2012 population of about 590 million persons in Latin America (1.5 per million) should be compared with the about 10,000 autotransplants performed in North America with an estimated 2012 population of 360 million (28 per million) indicating an almost 20-fold reported lower autotransplant rate in Latin America. Comparable rates for allotransplants per 1 million population are 0.6 versus 25, a 40-fold lower rate in Latin America. Even more striking are numbers of transplants from HLA-matched unrelated donors which were less than 100 in Latin America versus about 4000 in North America, again a 40-fold difference.
Figure 1.
Figure 2.
Less than 50 umbilical cord blood cell transplants were done in Latin America in 2012 versus about 1000 in North America, a 40-fold population-adjusted difference. Reasons for the deficiency in transplants in general and especially in allotransplants in Latin America are discussed in detail below. We also received data from Cuba not included in the CIBMTR dataset indicating about 25-30 transplant per year most of which were autotransplants.2
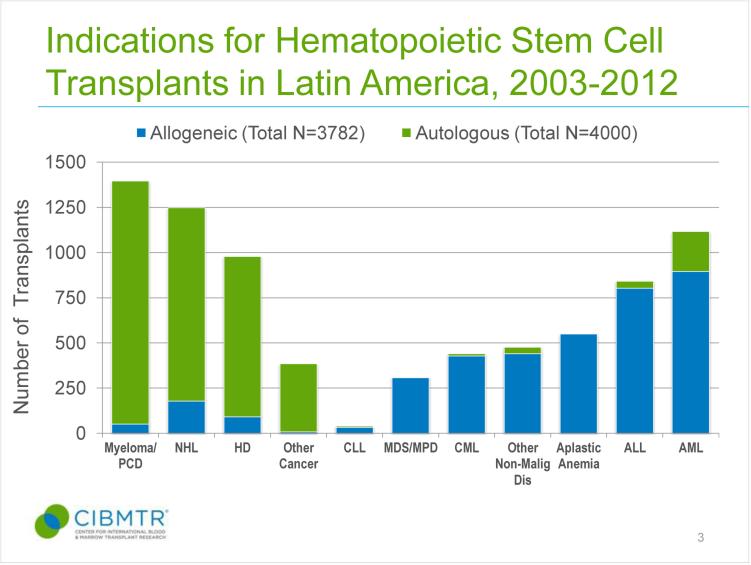
In our dataset about one-half of autotransplants in Latin America 2003-2012 were in persons with plasma cell myeloma and about 40 percent in persons with lymphomas (Figure 3). These proportions are similar to those reported in North America. About 75 percent of allotransplants in Latin America were done for leukaemias, a proportion also similar to North America. These data indicate Latin and North American transplant experts see generally similar indications for transplants in treating haematologic neoplasms but the frequency with which transplants are done in Latin America is substantially less as indicated above. Interestingly, about one-quarter of allotransplants reported to the CIBMTR from Latin America were in persons with bone marrow failure syndromes compared with only about 3 percent of allotransplants in Europe and North America likely reflecting a higher incidence of Fanconi anaemia in some Latin American countries and possibly participation of selected centres in the CIBMTR.
Figure 3.
Median age of persons receiving allotransplants in Latin America, 25 years, is substantially younger than median of persons receiving allotransplants in Europe and North America, 46 years. A similar shift to younger age recipients was found for autotransplant recipients, medians of 45 versus 56 years.
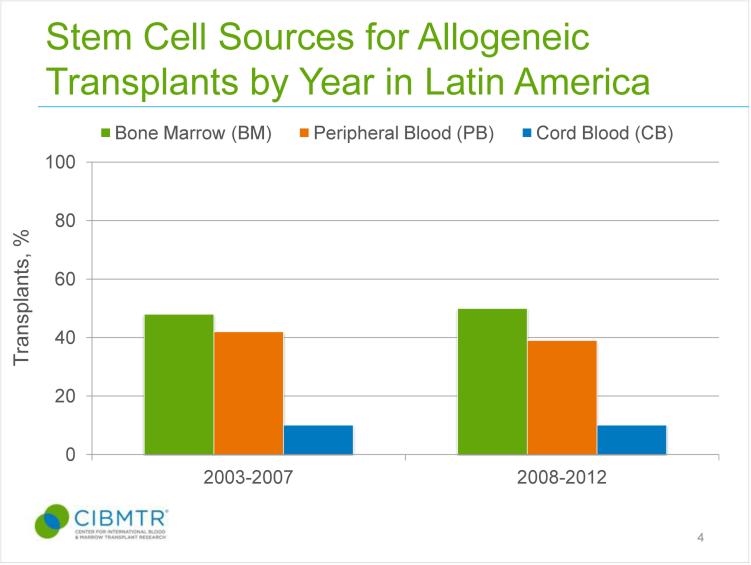
Another difference is graft type. In Europe and North America in 2008-2012 there were twice as many blood cell allografts as bone marrow allografts whereas there were equal proportions in Latin America. However, the proportion of allografts using umbilical cord blood cells, about 10 percent, was similar in Europe, North America and Latin America. Another difference in the CIBMTR dataset of US versus Latin American allotransplants is in the proportion of allotransplant from HLA-matched unrelated donors about 50 percent in the US versus about 25 percent in Latin America. Interestingly, only 10 percent of HLA-matched unrelated donor transplants in the US were done in persons classified as Hispanic, Latino or of Spanish origin compared with their 17 percent proportion of the US population. Figure 4 shows the distribution of graft types in Latin America in two intervals, 2003-2007 and 2008-2012. Roughly equal numbers of blood cell and bone marrow grafts were done in both intervals with a slight increase in the proportion of umbilical cord blood cell grafts. This situation differs from Europe and North America where a much higher proportion of blood cell grafts were done in the 2008-2012 interval. Causes for this difference may be unavailability of continuous flow blood cell separators at some centres and expensive software.
Figure 4.
Readers should also consider several other variables when evaluating these data. For example, population age is left-shifted in most Latin American countries compared with Europe and North America. This means cancers such as plasma cell myeloma, acute myeloid leukaemia and most lymphoma, diseases predominately of older persons, have lower incidences and prevalence in some Latin American countries. As such, there are proportionally fewer potential transplant recipients. Further, large areas of some countries such as South Argentina, North and Northeast Brazil and South Mexico have large populations with limited access to health care. Consequently, many cases of these diseases are not diagnosed and, if diagnosed, not referred for a transplant. Despite these and other limitations it is clear there is a huge deficiency in transplant activity in Latin America.
It is important to acknowledge potential effects of un-quantified, un-quantifiable and possibly un-identified variables associated with transplant activity reporting patterns such as a country's wealth and the proportion of public, private and academic transplant centres. These variables may imposed different limits to transplant activity in the vastly different countries comprising Latin America.
Special Considerations
Heath care infrastructure and economics
Health care infrastructure, access and economics are highly-confounded. Although percent GDP invested in health care in Latin American countries is not too dis-similar to European countries and Canada (and much less than the US), the absolute monies available differ strikingly. For example, according to Organization for Economic Cooperation and Development (OECD) Health Data 2012 the 8 percent of GDP invested in health care in Haiti translates to about $400 USD per capita versus $3,400 USD per capita in the UK and $ 8,200 USD per capita in the US and $3,300 for all OCED countries. The Table shows per capita health care investment of selected Latin American countries as percent of GDP according to the World Health Organization Global Health Expenditure 2012 database. The range is 3.4 percent (Venezuela) to 9.9 (Costa Rica) with a median value of 6.5 percent. Also shown in the Table are comparable data from Europe and North America ranging from 8.9 percent (Spain) to 17.1 percent (US) with a median of 10.1 percent. No Latin American country was above 10 percent whereas only 4 of 11 European and North American countries were below 10 percent.
Table.
Health Care Expenditures as Percent of GDP
| Argentina | 7.3 | Canada | 10.9 |
| Bahamas | 7.3 | Denmark | 10.6 |
| Belize | 5.4 | France | 11.7 |
| Bolivia | 6.1 | Germany | 11.3 |
| Brazil | 9.7 | Italy | 9.1 |
| Chile | 7.7 | Netherlands | 12.9 |
| Colombia | 6.8 | Norway | 9.6 |
| Costa Rica | 9.9 | Spain | 8.9 |
| Cuba | 8.8 | Switzerland | 11.5 |
| El Salvador | 6.9 | United Kingdom | 9.1 |
| Granada | 6.3 | United States | 17.1 |
| Guatemala | 6.5 | ||
| Guyana | 6.5 | ||
| Haiti | 9.4 | ||
| Honduras | 8.6 | ||
| Mexico | 6.2 | ||
| Panama | 7.2 | ||
| Peru | 5.3 | ||
| Trinidad/Tobago | 5.3 | ||
| Venezuela | 3.4 |
Haematopoietic cell transplants are expensive, especially allotransplants and more so allotransplants from donors other than HLA-identical siblings (see below). An accurate average cost is difficult to estimate because of different accounting practices in different countries and in different health care systems. However, $350,000-$800,000 USD is a reasonable approximation for an allotransplant in the US. 3 In most instances this is covered by private or public health insurance. Comparable cost in Latin America ranges from $25,000-$75,000 USD. Consequently, it is clear many Latin American health care systems cannot pay for transplants.
Availability of hospital beds for transplant recipients is another important issue. Numbers of inpatient beds allocated for transplants in a hospital is typically fixed. Autotransplants require, on average 20 hospital days whereas allotransplants from an HLA-identical sibling require on average 30 days. When an alternative donor is used such as an HLA-matched unrelated donor, HLA-partially-matched umbilical cord blood cells or an HLA- mismatched related donor average hospital days is 40-50 days. Re-admissions for transplant-related complication and/or disease recurrence are typically to the same hospital and unless a 2nd transplant is done are often not reimbursed by health authorities. In light of this, it is easy to see why Latin American transplant experts favour autotransplants and HLA-identical sibling transplants over alternative donor transplants. However, even the 20 day hospitalization for an autotransplant is longer than in the US and likely reflects several factors such as less developed outpatient facilities, poorer housing conditions, greater distances between homes and transplant centres, less access to transportation, lower social development and education level of recipients and potential caregivers. For example, in Europe and North America most ill persons prefer, if possible, to be at home, an attitude not as common or feasible in Latin America.
Expertise and personnel
Transplants, especially allotransplants, requires a well-developed health care infrastructure. Although transplants are typically done by haematologists and oncologists, sophisticated expertise is needed in diverse disciplines including histocompatibility testing, blood banking, infectious diseases, pathology, pharmacy and others. Often only tertiary care centres can assemble sufficient expert personnel to effect a successful transplant program. However, as we discuss below, a shift towards reduced-intensity transplants may improve this limitation by requiring less transplant-specific expertise.
Reimbursement
Government health care authorities are the most common payors of transplants in most Latin American countries. Typically these authorities have a policy of fixed reimbursement for a transplant. Because transplants from alternative donors are much more expensive than autotransplants or transplants from an HLA-identical sibling, most hospitals in Latin America have a net loss of revenues when an alternative donor transplant is done. This results in substantial pressure (economic, social, etc.) on transplant physicians to favour autotransplants and transplants from HLA-identical sibling donors over other types of transplants. This situation contrasts with the US whereas transplants are reimbursed mostly by private payors and where costs are itemized. (There are exceptions when a payor contracts with a hospital for a fixed cost but this is uncommon.) Consequently, transplants at US hospitals constitute an important revenue source and transplant experts are encouraged to do more transplants and even more complex transplants in some instances. Hospitals will often expand numbers of beds available for transplants because of the favourable economics.
Drug availability
Many drugs commonly-used in transplant recipients have limited use in other medical settings. Examples are thiotepa and intravenous busulfan and several anti-virus drugs such as cidofovir, ribavirin, foscarnet and vidarabine. There are 2 issues here. One is the high cost of these drugs. Because transplants are reimbursed at a fixed rate by most Latin American health authorities, more complex allotransplants such as those from alternative donors which typically require greater use of these drugs are less likely to be done. A second is many of these drugs are unavailable or very expensive in some or many Latin American countries. The limited market for some drugs is a dis-incentive for drug companies to seek regulatory approval. This is further complicated by the lack of a supra-national Health Authority such as the European Medicines Agency (EMA) therefore requiring approval in each country. Although approval in some countries such as Brazil and Mexico covers large populations, most Latin American countries are small. Compare this with an approval from the US Food and Drug Administration (FDA) which covers about 320 million persons. These considerations limit drug availability and consequently limit performing transplants from alternative donors.
Another interesting issue is the unavailability and/or high cost of drugs which might be used as an alternative to transplants, especially in plasma cell myeloma. For example, bortezomib, lenalidomide and pomalidomide are not widely-available in Latin America and quite expensive when imported. 4 In contrast, melphalan used for autotransplants is widely-available and cheap. This should result in a bias to refer persons with plasma cell myeloma for an autotransplant in Latin America compared with Europe and North America where these drugs are widely available (albeit expensive), However, this bias does not operate in acute leukaemias or lymphomas where conventional drugs are widely-available and cheaper.
Infectious diseases
Transplants in Latin America pose some unique challenges from an infectious diseases perspective. For example, frequencies of prior infection of recipients and donors with herpesviruses, Epstein-Barr virus (EBV), cytomegalovirus (CMV), hepatitis viruses-A, -B and -C and toxoplasmosis are substantially higher than in Europe and North America.5 This likely reflects social and economic conditions in many countries. Several of these agents, especially CMV, are frequently re-activated in transplant recipients. This means Latin American transplant centres need considerably greater resources for diagnosing, preventing and/or treating CMV-activation and –infection. These resources, especially drugs used to prevent CMV- and hepatitis-B-virus infection and/or reactivation, are expensive and several newer drugs are unavailable in many or most Latin American countries. Additional virus infections in transplant recipients requiring unavailable and/or expensive drugs in Latin America include adenovirus and BK virus. Fungal infections are also more frequent in immune compromised persons in Latin American countries 6. For example, Fusarium spp. infection in Brazil is more common than in other countries requiring therapy with azole anti-fungals or liposomal amphotericin-B. 6 Also, there is a recent epidemic of Dengue in Brazil which has affected several transplant recipients.
There is also the issue of overlooked tropical disease including tuberculosis, leprosy, Chagas disease, malaria, leishmaniasis, dengue, yellow fever and also measles in Latin America. 7 These disease are uncommon in Europe and North America but need to be addressed. Therapy of some of these diseases is typically inexpensive and effective drugs are widely-available. However, there is no therapy for some of these diseases.
Genetic diversity and unrelated donor registries
Another issue is genetic diversity. Allotransplants require some degree of genetic compatibility between donor and recipient. Initially, transplants were restricted to HLA-identical siblings or genetically-identical twins. Consequently, likelihood of finding an appropriate related donors correlates with family size. Average f family size in Latin America is larger than in Europe or North America favouring the likelihood of finding an appropriate donor. However, recently an increasing proportion of allotransplants are from HLA-matched unrelated persons. Probability of identifying such a donor depends on several variables including the degree of genetic heterogeneity in a country and on composition and size of unrelated donor registries. Some Latin American countries such as Bolivia, Costa Rica and Uruguay are relatively genetically homogeneous whereas others such as Brazil, Mexico, Haiti and Bolivia are far more diverse. Most countries with large populations have much greater genetic diversity than European and North American populations. Additionally, unrelated donor registries in Latin America are proportionally smaller than similar registries in Europe and North America. This combination makes it far less likely a donor will be found for a potential Latin American transplant recipient. Furthermore, many ethnic groups constituting large proportions of the populations of many Latin American countries such as Americo-Indians are under-represented in unrelated donor registries. The net effect of these factors is to decrease the likelihood of finding an appropriate unrelated donor in Latin America. Argentina, Brazil, Chile, Mexico and Panama have volunteer donor registries. Somewhat remarkably, Brazil (2015 population estimate 202 million) has an unrelated donor registry (REDOME) with 3.5 million volunteers. (www.inca.gov.br) However, on a proportional basis this is low compared to the US National Bone Marrow Donor Program (NMDP; 7 million donors with a 2015 population estimate of 320 million) and Germany (5 million donors with a 2015 population estimate of 83 million). Despite this potential resource in Brazil only about 270 unrelated donor transplants are done annually compared with more than 4,000 in the US 8 and more than 2100 in Germany. About 200 of the unrelated donors for transplant recipients in Brazil were from the Brazilian registry; the remainder were from donors in Europe and North America. The under-utilization of the large Brazilian unrelated donor registry compared with the US and Germany underscores other diffusion barriers discussed such as infrastructure and economics. The high proportion of unrelated European donor grafts likely reflects the disproportionately high numbers of persons of European genetic background receiving allotransplants in Brazil.
Umbilical cord blood cell transplants
A recent alternative donor source is HLA-partially-matched umbilical cord blood cells from unrelated donors. Typically these units are collected and stored frozen. Some data suggest results of transplant from umbilical cord blood cell donors are comparable to outcomes of transplants from HLA-matched unrelated blood cell or bone marrow donors, especially in young persons. The advantage of this type of transplant is it can be done relatively quickly compared with the considerable time required to identify and confirm an HLA-matched unrelated donor. With the proportionally large numbers of births in Latin America it should be easier to develop umbilical cord blood cell banks than elsewhere. However, this approach requires considerable infrastructure and is costly for several reasons including maintaining such a bank and because hospitalizations after this type of transplant are typically longer than after conventional transplants (discussed above). There are public umbilical cord blood banks in Argentina, Brazil, Chile, Mexico and Panama. However, only about 50 transplants are done annually in Latin America from umbilical cord blood cell donors versus about 500 in North America, a 20-fold population-adjusted difference. For several reasons including high demand for infrastructure and expertise, relatively small donor bank sizes and high cost we think volume of HLA-partially-matched umbilical cord blood cell transplant is unlikely to increase substantially, except perhaps in children. Transplants from HLA-matched unrelated donors and especially from HLA- mismatched related donors (who can be quickly-identified) are much more likely to fill the gap in persons without an HLA-identical sibling donor. Data from the CIBMTR from Latin Ameican contributing centres, indicate no substantial increase using umbilical cord blood donors 2003-2007 versus 2008-2012.
HLA-mismatched related transplants
Another development not unique to Latin America but with the potential to increase diffusion of transplant technology is using HLA-mismatched related donors for persons without an HLA-identical sibling donor or a HLA-matched unrelated donor. An HLA-mismatched related donor is rapidly identified for almost every potential transplant candidate. Use of such donors increases availability, decreases costs, avoids the need for large registries of HLA-typed unrelated volunteers and for banks of frozen HLA-typed umbilical cord blood cells. In the past these transplants were complex requiring in vitro manipulation of the graft. However, the recent use of unmodified grafts combined with posttransplant cyclophosphamide has greatly simplified this approach and reduced costs. Short-term outcomes of such transplants are roughly similar or only slightly worse than transplants from HLA-identical siblings or HLA-matched unrelated donors. Results of randomized clinical trials and comparisons of long-term outcomes are not reported. This approach could greatly expand transplant activity in Latin America. However, as discussed with regard to HLA-typed unrelated donor registries, other factors including infrastructure and increased need for more expensive and/or unavailable drug and economics are likely more important rate limiters of transplant diffusion than donor availability. Predicting how using HLA-mismatched-related donors will alter the landscape of allotransplants worldwide and specifically in Latin America is challenging. Obviously this approach could greatly expand numbers of potential transplant recipients with an appropriate donor. However, these types of transplants require more infrastructure and transplant expertise and are typically much more expensive than other types of allotransplants. How these opposing forces will balance in the future in Latin America is unclear but we anticipate increasing numbers of transplants from HLA-mismatched related donors.
Reduced-intensity transplants
Another recent trend is giving lower doses of drugs and/or radiation pretransplant referred to as reduced-intensity or mini-allotransplants. There is controversy whether results of reduced-intensity transplants are comparable to those of conventional transplants. Most data suggest similar survival outcomes despite differences in non-relapse mortality and cumulative incidence of relapse. This approach seems attractive in Latin America because early transplant-related complications should be less. However, 3 observations urge caution with this hypothesis. First, drugs typically used for reduced-intensity transplants, such as fludarabine and anti-thymocyte globulin (ATG), are more expensive than drugs used in conventional transplants. Whether using these drugs is necessary is unknown. Second, although 100 day transplant-related complications are less, one year rates are similar to conventional transplants in most studies. These later events may be unknown or remote to the transplant centre and/or health authorities. Consequently, although the transplant cost may appear lower, total cost to the health care system is probably not substantially reduced. Third, reduced-intensity transplants are typically associated with higher rates of disease recurrence. Sometimes a second transplant is done in which case the cost needs to be considered as part of a complete programme for treating the disease. However, if recurrent disease is treated otherwise, such as by chemotherapy, this cost is often unknown to or not considered by the transplant centre. However, the total cost to the health care system may be the same or higher than one conventional transplant. There are no randomized trials comparing total costs of conventional versus reduced-intensity transplants to know if these predictions are correct. In many instances disease recurrence is not treated and recipients die. This is, of course, a monetary savings but a social loss and humanitarian tragedy if preventable. In young persons it may also represent an important economic loss to the society.
Latin American transplant centres are increasingly switching to reduced-intensity transplants because immediate complications are less than with conventional transplants and some of the problems we discuss above such as infrastructure, few hospital beds, short-term costs and drug availability are temporarily improved. For example, in 2002 the proportion of reduced-intensity allotransplants in Latin America in the CIBMTR dataset was 11 percent whereas in 2013 it was 29 percent, a more than 2 fold increase. However, if we consider total health care expenditure for reduced-intensity allotransplants this shift may be inappropriate from a fiscal perspective.
Cultural attitudes towards transplants
One issue we considered was whether the lower transplant activity in Latin America compared with North America, especially allotransplants, might reflect culture-based differences such as willingness to receive tissue from another person including a relative and/or reluctance to donate blood or bone marrow cells. There is no perfect answer to this question but we addressed it in three ways. First, we considered whether rates at which people donate conventional blood units to not-for-profit organizations such as the Red Cross or equivalent national organizations differ between Latin America and North America. We found that in the larger, better-developed countries rates of blood donation were similar to North America. This was also so of smaller, less-developed countries. Whether this reflects different culturally-determined attitudes to blood donation, infrastructure-based limitations or a combination is unclear.
Second, we compared the size of the Brazilian unrelated donor registry with that of registries in Germany and North America. As we discussed the population-adjusted size of the Brazilian registry is at least 20-fold less than might be expected. However, in an absolute sense it is large with 3.5 million volunteers. Given the recent start of the Brazilian registry compared with other registries and economic constraints we take these data to indicate a willingness of Brazilians to donate haematopoietic cells for a transplant. There are too few data to judge the rate of loss of volunteers. Also, rates of volunteerism in other Latin American countries are less well-studied.
Third, we compared rates of allotransplants from HLA-identical siblings between Latin and North America restricting the North American analysis to approximately 52 million people classified by the US Census Bureau as Hispanic, Latino or Spanish. In CIBMTR analysis restricted to the US we found the population-adjusted frequency of HLA-identical sibling transplants in persons classified as Hispanic, Latino or of Spanish origin (termed Hispanics) to be lower than the frequency in persons of predominately European descent.g Because average family size of Hispanics is larger than that of persons of predominately European descent this decreased transplant frequency cannot result fewer potential donors. Whether it reflects different culture-based attitudes to transplants, socio-economic differences, other variables or combinations of these is unknown and likely unknowable. We did not compare rates of unrelated donor transplants because of under-representation of persons classified as Hispanic in the US National Marrow Donor Program (NMDP). 9 Again, it is impossible to know whether this reflects cultural attitudes or other variables such as the adoption of heath care attitudes of the resident country, access to health care and economics. The sum of these data, although inconclusive, suggest a modest culture-based bias against transplants compared with persons in the US of predominately European descent.
Transplant strategies for Latin America
The diverse constraints to the diffusion of transplant technology to Latin America we discuss have led to several interesting solutions some relatively unique to Latin America, others global. One strategy had been to do autotransplants with stored rather than frozen blood cells. This eliminates the need for expensive, technically-demanding equipment and storage and reduces cost. Results of this approach seem comparable to using frozen cells. However, because the unfrozen blood or bone marrow cells must be obtained temporally proximal to the autotransplant numbers of persons with lymphoma or plasma cell myeloma amenable to this approach is somewhat reduced. Some North American transplant centres have considerable experience performing autotransplants and even allotransplants in a mostly outpatient setting. This reduces costs and requires less infrastructure. 10-13 Costs of autotransplants in Latin America range from $10,000-50,000 USD and allotransplants from $20,000-$100,000 USD.h Median costs are about one-half or less than similar transplants in Europe and North America. Some of this seemingly lower cost is artificial reflecting different accounting procedures and concepts of health care provision. However, some of the lower costs may reflect Latin American interventions discussed including using outpatient facilities and less expensive drugs. However, these savings may not be realized in the setting of allotransplants from alternative donors such as HLA-mismatched relatives (see above). Another strategy is to use less expensive drugs such as melphalan, cyclophosphamide and cyclosporine pre- and posttransplant. This is sensible as most data indicate only marginal improvement in outcomes when newer, more expensive drugs are used.
These innovative adaptive strategies are, however, counterbalanced by an important force not unique to Latin America: physicians want to replicate what their colleagues elsewhere are doing. And they also want to use the newest (and invariably most expensive) drugs and procedures even if improvements in outcomes are only marginal or sometimes nil. This unfortunate tendency is strong, pervasive, fundamental to human nature and not easily overcome. These issues are discussed elsewhere. 14
Compromise and Cooperation
Progress in transplants requires comparing alternative interventions in large randomized clinical trials. Much of the recent improved transplant outcomes in Europe and North America resulted from national, regional and international trials of new therapies. Success of this approach requires a specific mind set: willingness to compromise personal opinions, beliefs, etc. towards a common goal. Such compromise is not easy. And it is not by any means inexpensive. For example, although there are organizations such as the Organization of American Countries (OAS) and the Pan American Health Organization (PAHO) these are less common and less active than equivalent European and North American entities such the European Union, North Atlantic Treaty Organization (NATO) and Organization of Economic Cooperation and Development (OECD). Some scholars suggest notions of scientific and medical cooperation are less well-developed in Latin America than elsewhere. Whether this situation relates to the colonization and exploitation of Latin American countries by Europeans and North Americans is controversial. 15 This may be changing and there is evidence of success in some related spheres such as the Latin American Society for Immunodeficiencies (LASID) which has coordinated diagnosis and therapy of immune disorders in 12 countries for more than 20 years. 16
Publications
One indirect measure of volume and quality of transplant activities in Latin America is publications in peer-reviewed scientific journals. Between 1990 and 2014 369 transplant-related studies originating in Latin America were published in peer-reviewed journals. About one-half were published in journals with an impact factor >3. Although the largest number of publications were from Brazil and Mexico, the highest per capita publication rate was from Uruguay. Increasing frequency of scientific reports from Latin American centres is encouraging and suggestive of substantial progress.
Haematopioetic Cell versus Solid Organ Transplants
In analyzing the aetiology(ies) of the deficiency of haematopoietic cell transplant in Latin America it is potentially interesting to compare the magnitude of this deficiency compared with other types of transplants such as kidney, heart and liver. Unfortunately few data are available to address this issue. A more detailed analysis will be forthcoming.
Summary and the future
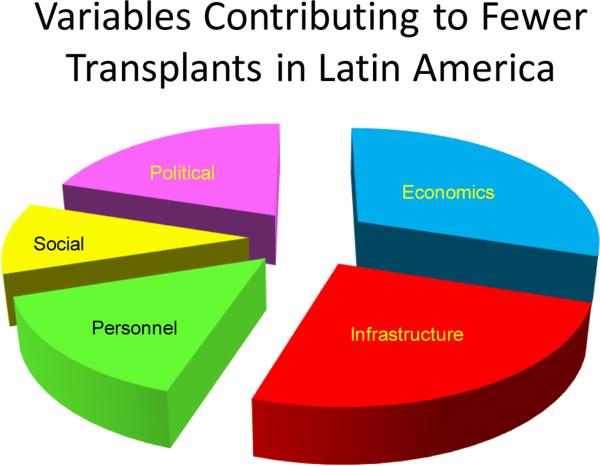
Our impression of the major variables currently limiting the diffusion of transplant activity in Latin America is indicated in Figure 5. These categories are clearly inter-related and somewhat arbitrary. For example, although we see economics and infrastructural limitations as the largest contributors to a deficiency of transplant activity, lack of monies also impacts personnel. Also, political decisions are, ultimately, the determinant of economic policies and subsequently a country's wealth in many instances.
Figure 5.
10 transplant experts including the authours were queried were asked to partition 100 percent into contribution to decreased haematopoietic cell transplant volume in Latin America. Proportions indicate mean values.
Recently, a Latin American Bone Marrow Transplant Group (LABMT) i was formed under encouragement of the Worldwide Network for Blood and Marrow Transplantation (WBMT). The WBMT/LABMT includes 153 transplant centres in 12 countries including Argentina, Brazil, Chile, Columbia, Costa Rica, Ecuador, Mexico, Panama, Paraguay, Peru, Uruguay and Venezuela. This is substantially more than the 49 centres in nine countries reporting to the CIBMTR. However, the CIBMTR dataset has subject-level data and is audited. LABMT is participating in the WBMT global transplant survey of annual transplant activity, indications and transplant types. This exercise is needed for a more complete view of regional transplant activity and will hopefully stimulate collaboration of transplant centres in Latin America.
Despite the substantial challenges to diffusion of transplants in Latin America we are convinced the volume of transplants will increase for several reasons we cited. But the reality is transplants are a high-technology, expensive undertaking for physicians and health authorities in developing countries. Progress requires advances outside the direct medical sphere including political and social involvement arenas. Increased use of reduced-intensity transplants and of HLA-haplotype-mismatched donors may ultimately decrease costs and eliminate the need for large and expensive HLA-typed unrelated donor registries and umbilical cord blood cell banks and expand transplants to more people needing them. In contrast, the wider availability of donors may stress resources of transplant centres and countries’ health care systems. Immediate problems to solve include wider access to expensive drugs. We also believe there is a need to improve communication between transplant centres in Latin America and encourage reporting to the LABMT regionally and the CIBMTR globally. High-quality data reporting can help identify and advance regional issues. Latin America transplant experts face an important challenge. We are optimistic they will succeed making transplants simpler, cheaper and more widely-available to the millions of persons living in Latin America.
Acknowledgements
The following colleagues provided helpful comments: Luis Fernando Bouzas (Instituto Nacional de Cancer–INCA, Brazil), Sebastian Galeano, Hospital Británico, Uruguay, Guillermo J. Ruiz-Arguelles Centro de Hematologia Puebla, Mexico.
Support. RPG acknowledges support from the NIHR Biomedical Research Centre funding scheme.
Footnotes
Defined as the US and Canada. Although Mexico and Central America are formally part of North America they are more reasonably considered part of the Latin American region for analyzing diffusion of high technology health care issues.
Classification of a developed versus a developing country is controversial and differs between organizations such as the International Monetary Fund (IMF), World Bank and United Nations Development Program (UNDP). We consider the 26 Latin American countries developing using UNDP terminology. However, Chile and Mexico are members of the Organization for Economic Cooperation and Development (OECD) and are considered developed countries by some organizations.
Un-adjusted for inflation and currency devaluations.
Gini index measures the extent to which the distribution of income or consumption expenditure among individuals or households within an economy deviates from a perfectly equal distribution. A Lorenz curve plots the cumulative percent of total income received against cumulative numbers of recipients, starting with the poorest individuals or households. The Gini index measures the area between the Lorenz curve and a hypothetical line of absolute quality, expressed as a percent of the maximum area under the line. A Gini index of 0 represents perfect equality whereas an index of 100 implies perfect inequality.
Although several surveys indicate more active transplant centres than we analyzed, data from these centres is unaudited. Consequently we chose a subset of centres with validated data. Several publications on global transplant activity do not specify transplant volume by geographic region and/or country.
Probability of a person having an HLA-identical sibling is 1-(0.75) × E+N where N=number of siblings.
The US Census Bureau distinguishes race from ethnicity. Hispanic or Latino is designated as an ethnicity. The 2010 questionnaire asks whether a person is of Hispanic, Latino or Spanish origin. If the reply is yes, it then asks is the person from Mexico, Puerto Rico, Cuba or another Hispanic, Latino or Spanish origin. If yes to Spanish origin, the country should be specified i.e. Argentina.
Costs were estimated based on a random sample of 14 transplant centres
Conflict of Interest. No relevant conflict of interest.
References
- 1.Gratwohl A, Pasquini MC, Aljurf M, Atsuta Y, Baldomero H, Foeken L. One million haemopoietic stem-cell transplants: a retrospective observational study for the Worldwide Network for Blood and Marrow Transplantation (WBMT). The Lancet Haematology. 2015;2:e91–e100. doi: 10.1016/S2352-3026(15)00028-9. [DOI] [PubMed] [Google Scholar]
- 2.Carnot-Uria J. Achievements and perspectives of stem cell transplantation in Cuba. Revista Cubana Hematologia, Immunologia y Hemoterapia. 2012;28:108–110. [Google Scholar]
- 3. http:/www.publications.milliman.com/research/health-rr/pdfs/2011-us-organ-tissue.pdf.
- 4.Ruiz-Arguelles GJ, Tarin-Arzaga LC, Gonzalez-Carillo ML, Gutierrez-Riveroll KI, Rangel-Malo R, Gutierrez-Aguirre CH, et al. Therapeutic choices in patients with Ph-positive CML living in Mexico in the tyrosine kinase inhibitor era: SCT or TKIs? Bone Marrow Transplantation. 2008;42:23–8. doi: 10.1038/bmt.2008.90. [DOI] [PubMed] [Google Scholar]
- 5. http://www.who.int/bulletin/volumes/86/10/07-046128/en/
- 6.Nucci M, Garnica M, Gloria AB, et al. Invasive fungal diseases in haematopoietic cell transplant recipients and in patients with acute myeloid leukaemia or myelodysplasia in Brazil. Clin Microbiol Infect. 2013;19:745–51. doi: 10.1111/1469-0691.12002. [DOI] [PubMed] [Google Scholar]
- 7.Machado CM, Martins TC, Colturato I, Souza M, Anderson JS, Souza MP. Epidemiology of neglected tropical diseases in transplant recipients. Review of the literature and experience of a Brazilian HSCT center. Rev Inst Med trop S. Paulo. 2009;51:309–24. doi: 10.1590/s0036-46652009000600002. [DOI] [PubMed] [Google Scholar]
- 8.Pasquini MC, Zhu X. Current use and outcome of hematopoietic stem cell transplantation: CIBMTR Summary Slides. 2014 Available at: http://www.cibmtr.org.
- 9.Gragert L, Eapen M, Williams E, Freeman J, Spellman S, Baitty R, et al. HLA Match Likelihoods for Hematopoietic Stem-Cell Grafts in the U.S. Registry. N Engl J Med. 2014;371:339–48. doi: 10.1056/NEJMsa1311707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruiz A, Ruiz-Argüelles GJ. A Mexican way to cope with stem cell grafting. Hematology. 2012;17(Suppl 1):S195–7. doi: 10.1179/102453312X13336169157130. [DOI] [PubMed] [Google Scholar]
- 11.Gutiérrez-Aguirre CH, Gómez-De-León A, Alatorre-Ricardo J, Cantú-Rodríguez OG, González-Llano O, Jaime-Pérez JC, et al. Allogeneic peripheral blood stem cell transplantation using reduced-intensity conditioning in an outpatient setting in ABO-incompatible patients: are survival and graft-versus-host disease different? Transfusion. 2014;54:1269–77. doi: 10.1111/trf.12466. [DOI] [PubMed] [Google Scholar]
- 12.González-Llano O, Rodríguez-Romo LN, Mancías-Guerra Mdel C, Tarín-Arzaga L, Jaime-Pérez JC, et al. Feasibility of an outpatient HLA haploidentical stem cell transplantation program in children using a reduced-intensity conditioning regimen and CD3-CD19 depletion. Hematology. 2014;19:10–17. doi: 10.1179/1607845413Y.0000000088. [DOI] [PubMed] [Google Scholar]
- 13.Jaime-Pérez JC, Heredia-Salazar AC, Cantú-Rodríguez OG, Gutiérrez-Aguirre H, Villarreal-Villarreal CD, Mancías-Guerra C, et al. Cost structure and clinical outcome of a stem cell transplantation program in a developing country: The experience in Northeast Mexico. Oncologist. 2015;20:386–92. doi: 10.1634/theoncologist.2014-0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woolhandler S, Himmelstein DU, Labar B, Lang S. Transplanted technology: Third World options and First World science. The New England Journal of Medicine. 1987;317:504–6. doi: 10.1056/NEJM198708203170810. [DOI] [PubMed] [Google Scholar]
- 15.Galeano E. Open Veins of Latin America. Monthly Review Press; New York, NY: 1997. [Google Scholar]
- 16.Condino-Neto C, Sorensen RU, Gomez-Raccio AC, King A, Espinosa-Rosales FJ, Franco JL. Current state and future perspectives of the Latin American Society for Immunodeficiencies (LASID) doi: 10.1016/j.aller.2014.05.007. http://dx.doi.org/10.1016/j.aller.2014.05.007. [DOI] [PubMed]