Abstract
Objective
CDC routinely conducts contact investigations involving travelers on commercial conveyances, such as aircrafts, cargo vessels, and cruise ships.
Methods
The agency used established systems of communication and partnerships with other federal agencies to quickly provide accurate traveler contact information to states and jurisdictions to alert contacts of potential exposure to two travelers with Middle East Respiratory Syndrome Coronavirus (MERS-CoV) who had entered the United States on commercial flights in April and May 2014.
Results
Applying the same process used to trace and notify travelers during routine investigations, such as those for tuberculosis or measles, CDC was able to notify most travelers of their potential exposure to MERS-CoV during the first few days of each investigation.
Conclusion
To prevent the introduction and spread of newly emerging infectious diseases, travelers need to be located and contacted quickly.
The risk of a pandemic caused by Middle East Respiratory Syndrome Coronavirus (MERS-CoV), a virus that causes predominantly respiratory symptoms and has a substantial case fatality rate in humans, is considered to be low,1 with limited human-to-human transmission documented in health-care and household settings.2,3 Although the virus has a low rate of infectivity, an affected air traveler has the potential to spread infection, and mathematical modeling suggests that the number of new cases depends on the length of the flight and the cabin location of the infected passenger.4 Several diseases with low infectivity rates (R0 <1) have been transmitted from person to person on long flights.5
The Centers for Disease Control and Prevention (CDC) has legal authority in the United States to conduct contact investigations involving travelers exposed to communicable diseases; contact investigations for diseases such as tuberculosis (TB),6 measles,7 rubella,8 pertussis, and meningococcal disease9 are performed routinely after exposure on commercial aircraft. In these routine investigations, travelers contacted for follow-up are limited to those in the seats or rows in close proximity to the index patients and sometimes to crew members. Decisions on whom to contact after exposure to a given disease are based on the aircraft airflow and traveler movement dynamics, population susceptibility, potential risks to contacts and others, the availability of public health resources, and the existence of effective prophylaxis or treatment.7,10–13 In addition to routine investigations, large-scale contact investigations, which include all passengers and crew members on a flight, have been performed for certain pathogens when the potential risk of illness or death was high or when little was known about transmissibility. Examples of pathogens that have prompted large-scale contact investigations among air travelers are influenza A(H1N1)pdm09,14 severe acute respiratory syndrome-associated coronavirus (SARS-CoV),15,16 and Ebola.17
Initial clinical reports of MERS-CoV infection described substantial illness and death among infected individuals,18,19 and, as of March 23, 2016, the World Health Organization reported 1,698 confirmed cases and a case fatality rate of approximately 36%.20 Evidence at the time suggested that the spread of MERS-CoV to other countries by commercial air travel was likely.21 Recent models suggest the continued risk of a small number of travelers with symptomatic MERS-CoV infection traveling to the United States each year.22 The introduction of MERS-CoV to other countries, including France,23 Italy,24 Germany,25 the Netherlands,26 and South Korea,27 has been described, but person-to-person transmission during air travel was not documented. However, given the severity of MERS-CoV infection and the evidence of transmission of SARS-CoV on flights,16 concern for the risk of MERS-CoV exposure to air travelers was heightened at the time of these investigations.
Because of the lack of information about transmission of MERS-CoV during air travel, CDC undertook large-scale airline contact investigations in May 2014, when two ill passengers who traveled from Saudi Arabia to the United States became the first confirmed cases of MERS-CoV infection in the United States.
METHODS OF TRACING AIR TRAVELERS
CDC receives more than 2,000 reports annually from private and public sources of travelers who are ill or who have died during travel (CDC unpublished data). Contact investigations involving air travelers are conducted for certain cases of communicable diseases for which transmission might occur simply by being a passenger on an aircraft with an infectious person, and public health intervention is warranted. The decision to conduct a contact investigation takes into account factors such as the clinical presentation of the index case, flight duration, and time elapsed since travel.
The process CDC uses to perform a large-scale airline contact investigation is the same used to perform a routine airline contact investigation. The three major steps are (1) confirming the flight information of the index patient, (2) obtaining the passenger manifest and contact information, and (3) providing traveler contact information to state and foreign public health authorities (Figure 1).
Figure 1.
Centers for Disease Control and Prevention timeline for tracing air travelers on domestic and international flights when travelers are exposed to communicable diseases, 2014
aDepending on the urgency of the contact investigation
bNTC is a division of Customs and Border Protection that provides advance antiterrorism targeting, research, and coordination.
DGMQ = Division of Global Migration and Quarantine
NTC = National Targeting Center-Passenger
Flight information confirmation
Flight itinerary information is typically obtained from the index patient during an initial interview with the local health department. CDC personnel then confirm this information with either the airline or Customs and Border Protection (CBP).
Obtaining passenger manifest and contact information
CDC uses a multistep process to obtain passenger contact information; this process is different according to whether the flight is domestic or international. First, CDC issues a manifest order to the airline. This manifest order cites the federal regulation (42 Code of Federal Regulations Part 71.32(b) as authorized by 42 U.S. Code § 264)28 that requires airlines to provide CDC with information on the index patient and the index patient's potential contacts, including full name, seat number, primary and secondary -telephone -numbers, permanent home address (or state of residence), passport number, and issuing country, as available. The time it takes for CDC to obtain the manifest varies, but information is typically received within two business days of the request for information on nonurgent cases, such as TB, in which contacts are not likely to become rapidly infectious or benefit from prophylaxis. Urgent orders are issued when the investigation involves highly infectious pathogens (such as measles) and when prophylaxis can be provided (e.g., for meningitis exposure).
Data obtained from manifests are often incomplete. Analysis of data received by CDC for 16 domestic-flight manifests ordered in 2013 showed that for 45 of 234 (19%) travelers, only the first and last name were provided (unpublished data, CDC, 2013); it was not possible to contact most of these 45 travelers because of missing contact information.
Contact information is frequently missing on international-flight manifests as well. For example, among 76 international flights arriving in the United States for which manifests were ordered in 2013, the airlines did not provide contact information for 1,335 of 2,500 (53%) travelers (unpublished data, CDC, 2013). However, for these international flights, CDC uses other information sources.
The primary sources used to supplement manifest data are federal databases accessed by CBP's National Targeting Center-Passenger (NTC).29 NTC's mission is to provide advance antiterrorism targeting, research, and coordination within CBP and among numerous law enforcement and intelligence agencies. To accomplish this mission, NTC uses advanced technology, including automated targeting and data processing systems and intelligence information. A CDC liaison stationed at NTC facilitates the collection of passenger contact information for CDC during a contact investigation. Rapid, secure communication between CDC and the U.S. Department of Homeland Security, of which CBP is a component, is accomplished using the Homeland Security Information Network, an Internet-based, information-sharing platform that connects all Department of Homeland Security mission partners.
NTC can access various passenger data sources to support public health contact investigations. One supplemental data system used is the Advance Passenger Information System, which provides CBP with pre-arrival and departure manifest data for all international travelers and crew members on aircraft or ships.30 After these supplemental methods were used for the 76 international-flight manifests ordered in 2013, at least one piece of contact information (e.g., e-mail address, residential address, telephone number) was available for more than 99% of travelers.
Customs declaration forms, completed by travelers flying into the United States, are another potential source of information. Only one form per family unit is required.31 The forms require travelers to provide a destination address in the United States, which could be a hotel or other temporary location. However, these forms are handwritten, might be incomplete or illegible, and must be manually sorted and reviewed by CDC personnel. Because they often do not include a permanent address, the forms might not be helpful if the passenger has left the temporary location. In addition, electronic applications, such as Mobile Passport Control, are used in lieu of the customs declaration form,32 and information collected by this system is not available to CDC. In general, because of these limitations, customs declaration forms are used only in urgent investigations when other information sources are not available.
The Transportation Security Administration's Secure Flight Program33 also collects information on all U.S.-bound air travelers. When making a reservation, all domestic and international travelers must provide their name, date of birth, and sex to the airline, which in turn provides this information to the Secure Flight Program for vetting against government security watch lists. Currently, no formal protocol is in place to provide Secure Flight Program data to CDC during public health investigations.
Providing passenger contact information to state and foreign public health authorities
All available passenger contact information is entered into a secure CDC database that automatically sorts the travelers by state of current home address. If a home address is not available, a telephone number area code is used, although this area code does not always indicate the traveler's current residence. The traveler list is then imported into CDC's Epidemic Information Exchange, where CDC can rapidly and securely notify state public health officials electronically about the index patients and contacts who are assigned to their state.34
Travelers initially assigned to one state often need to be reassigned to another state as the investigation progresses because they have continued their travel. Also, assignments are made based on the best information available, which might include a passport home address or a mobile telephone number that is no longer current.
For travelers with location information outside the United States, CDC notifies the foreign ministry of health of the appropriate jurisdiction or the national focal point for that country as designated under the International Health Regulations (2005),35 and provides flight information, clinical information about the index patient, and available contact information for exposed travelers. If CDC is aware that the index patient's itinerary includes multiple countries, notifications are also sent to those countries.
Travelers who cannot be assigned to a U.S. or foreign jurisdiction are often not contacted. However, some of these travelers will be identified by interviewing their travel companions or family members (Figure 1).
Evaluation of crew members
Contact investigation protocols include evaluation of crew members when it is likely they were exposed. For example, in TB investigations, where prolonged exposure is often needed for transmission to occur, a passenger seated beside someone with TB for eight hours or more would be considered a contact, whereas flight crew members with brief interaction would not. However, in measles investigations, where brief interaction is a risk for transmission, the crew members who served the ill passenger would be considered contacts. Crew evaluations are typically conducted by the airline's occupational health service with guidance from CDC or a state health department.
METHODS AND OUTCOMES OF MERS-CoV CONTACT TRACING
MERS-CoV infection index-patient notifications
CDC requires immediate reporting of patients who are suspected of having MERS-CoV infection.36 Both cases that prompted the first two contact investigations were reported to CDC by state health departments after travel when MERS-CoV infection was suspected.37
Flight confirmation of MERS-CoV infection index patients
For both MERS-CoV contact investigations, flight information was obtained by health departments through interviews with the index patients and was confirmed by CBP. The first index patient flew on April 24, 2014, from Riyadh, Saudi Arabia, to London, England, and then from London to Chicago, Illinois. The second index patient flew on May 1, 2014, from Riyadh to London, from London to Boston, Massachusetts; from Boston to Atlanta, Georgia; and then from Atlanta to Orlando, Florida.
Obtaining passenger manifests and contact information for MERS-CoV investigations
Index patient 1.
For the Riyadh-to-London flight, CDC requested information for U.S. citizens seated anywhere on the aircraft. The names, passport numbers, and limited contact information of nine U.S. citizens onboard were provided to CDC by Public Health England. Additional contact information was obtained by a CDC NTC liaison for all nine contacts. For the London-to-Chicago flight, the manifest was ordered from the airline and received later the same day. The 80-passenger manifest included contact information for all but seven travelers on the flight. NTC provided contact information for all 80 travelers within hours of the request.
Index patient 2.
This passenger traveled on four flights: two international and two U.S. domestic flights. CDC was not notified of any passengers on the Riyadh-to-London flight who needed to be contacted in the United States at the time of the investigation. The manifest for the London-to-Boston flight was provided on the same day it was requested with contact information for 86 of 188 (46%) travelers on the flight. NTC provided contact information for all but three travelers within approximately four hours.
Of the 333 travelers on two domestic flights, no contact information was provided by the airline for 71 (21%) travelers on the manifest. Because these were domestic flights, passport information was not available for most travelers and the manifests were not visible in the NTC. The airline later provided additional information, including dates of birth, which improved success in searching for these travelers. Data collection was complete for the domestic flights within 72 hours of receipt of the first manifest, and contact information for all but 18 travelers from these two flights was available after NTC assistance.
Customs declaration forms were not used during either investigation because it was determined that they were not likely to add any useful information.
Providing passenger contact information to state and foreign public health authorities for MERS-CoV investigations
For both MERS-CoV investigations, notifications to health departments were dispatched through usual procedures. Seventeen states were involved, with a median of two contacts per state (range: 1–12). One country was notified of 24 contacts. By the fourth day of the first MERS-CoV investigation, all 80 travelers on the London-to-Chicago flight had been notified. Additionally, the nine travelers identified on the Riyadh-to-London flight were notified within four days. One contact was determined to be outside of CDC jurisdiction but could not be located or contacted. Twelve crew members were contacted by the airline employer (Figure 2). Travelers were notified by telephone, e-mail, letter, or in person.
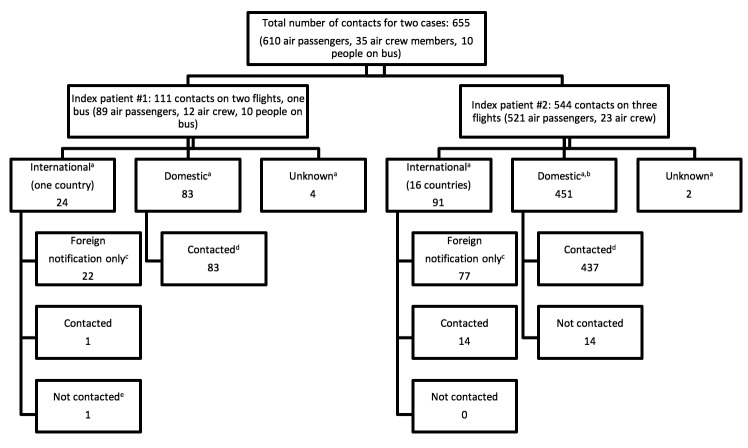
Figure 2.
Summary of how air travelers were traced during a contact investigation of the first two confirmed cases of Middle East Respiratory Syndrome Coronavirus infection in the United States, 2014
aLocation of passenger at initial contact
bOne person was determined to be outside of the Centers for Disease Control and Prevention's jurisdiction.
cForeign notification: notification sent to public health authorities in other countries, not directly to passengers
dContacted: passengers who were contacted by U.S. public health officials
eLocation of air crew was unknown, but they were contacted by their domestic airline of employment.
For the second investigation, 35 states or territories were involved, with a median of five contacts per state (range: 1–94). Sixteen countries were notified of 91 contacts. All 23 flight crew members were contacted by the airline. In total, 528 of 544 (97%) contacts were notified within five days of case confirmation (Figure 2). After initial contact, 91 of 528 (17%) travelers were reassigned to a different jurisdiction.
CDC offered to help states notify and interview exposed travelers, and provided such assistance to six states (32 travelers) for the first investigation and 12 states and a U.S. territory (118 travelers) for the second investigation. International notifications were conducted with the assistance of the Pan American Health Organization. In some cases, the International Health Regulations' national focal point was contacted; for others, the traveler was contacted by CDC directly (Figure 2).
Bus investigation
The first index patient traveled by airport shuttle bus from Chicago's O'Hare International Airport to northern Indiana, a one-hour trip. CDC worked with the shuttle company to identify the driver and nine travelers on the bus. Because manifests are not prepared for bus travel, credit card records were used to obtain passenger contact information for three passengers; in addition, the bus driver was contacted, and two passengers on the bus were airline staff members who were identified through their employer. The remaining four passengers had paid with cash and could not be identified. Of the 10 people traveling on the bus, six were contacted. The Indiana State Department of Health issued a press release with information about the bus itinerary, but no additional travelers were identified.
DISCUSSION
In conducting contact investigations of travelers, CDC uses established relationships with other federal agencies and existing notification systems to obtain contact information for travelers and provide rapid notifications to public health officials. The use of secondary data sources has greatly improved the accuracy and completeness of traveler contact information. Placement of a CDC staff member within CBP's NTC and the use of Department of Homeland Security information systems for secure data transmission have also contributed to the effectiveness and timeliness of this process.
Although the effectiveness of routine contact investigations of diseases with known transmission patterns, such as measles and TB, can be measured by the number of contacts who are provided prophylaxis or by the number of active secondary cases prevented,7,11 measuring the effectiveness of large-scale investigations of emerging infectious diseases such as MERS-CoV infection is more complicated. At the time of these investigations, little evidence existed on the patterns of MERS-CoV transmission during air travel, and the potential for illness and death caused by the disease was considered substantial. In investigations of an emerging infectious disease such as MERS-CoV infection, CDC contacts all passengers and crew members on the aircraft.14,17 These investigations provide an immediate public health response and inform decisions about future investigations. Effectiveness can more easily be measured in the number of travelers contacted and the speed with which this contact occurred. Although a few people were not contacted (e.g., bus passengers) during investigation of the first index patient, the potential for these passengers to contract MERS-CoV infection was considered low given their reported length of exposure. In addition, these investigations were not the only method used to trace travelers; numerous methods to alert health-care providers and the public about MERS-CoV were implemented, and patients under investigation were reportable to CDC.36
Although some questions about transmission of MERS-CoV remain,38 at the time of these investigations, the risk of transmission from someone who was asymptomatic was thought to be low, and quarantine of contacts was not implemented. Quarantine involves the restriction of movement of people who do not have symptoms of disease and is more likely to be used when transmission can occur during an asymptomatic state. Decisions to implement quarantine involve balancing individual rights with the importance of preventing the introduction and spread of communicable diseases in the United States.39
The primary limitation of tracing travelers during a contact investigation is the incomplete contact information on passenger manifests. Travelers may choose not to provide contact information to the airline, and many airlines do not require it. Also, some travelers may book a flight through a third party, such as a travel agency or an online booking agent, and provide information to the company that is not provided to the airline. Although contact information for most travelers on international flights entering the United States can usually be obtained from the Department of Homeland Security, missing information on domestic-flight manifests is a challenge. In response to this problem during the MERS-CoV investigations, CDC began requesting additional information in the manifest order, including date of birth and e-mail address. These additional pieces of information, when available, improve the success rate for finding individuals in databases. If contact information cannot be found for a given individual using these resources, CDC is unable to contact the individual. A study of CDC airline contact investigations on TB conducted January 2007–June 2008 reported that 74% of passengers had enough information to be assigned to a public health jurisdiction for follow-up, but CDC received follow-up evaluation results on only 26% of contacts.6 Because health departments are not required to return evaluations to CDC during routine investigations, returned evaluations do not represent all passengers contacted. The lack of initial contact information for many passengers, however, is the greatest challenge. Efforts to improve the information provided on manifests are ongoing and will require work with industry partners and, potentially, a change in government policy.
Another limitation is the large number of jurisdictional reassignments. When no address information for a traveler is provided, jurisdictional assignment is made based on the telephone area code. In the United States, where a mobile telephone number is often kept after moving, a telephone number may not reflect a person's current location. Requiring travelers to provide current address information at the time of booking would help to eliminate this limitation. Furthermore, many people take several flights within a short time, changing location several times during an investigation. Jurisdictional reassignments because of continued travel are unavoidable in most investigations. CDC aids state and local jurisdictions in rapidly reassigning these moving contacts.
Large-scale tracing of air travelers, based principally on CDC's routine protocols, was effective in rapidly notifying jurisdictions of potentially exposed contacts. Although CDC offered to help notify these travelers, most jurisdictions notified travelers themselves and reported their results to CDC. The public health infrastructure had the capacity to conduct the contact investigations, which involved rapidly contacting hundreds of travelers.
Alternatives to large-scale contact investigations have been proposed, such as using media announcements to notify travelers of possible exposure and encouraging them to monitor themselves and seek medical attention if symptoms develop. This option has the advantage of requiring fewer federal resources to implement but may cause unnecessary concern to individuals who were not exposed, and those who were exposed might not receive the notification. CDC recently leveraged both approaches for an Ebola contact investigation involving two commercial flights, sending a message out immediately through the media about affected flights while obtaining contact information from the airline to contact passengers directly.17
CONCLUSION
A large-scale expansion of routine processes for conducting contact investigations allowed for rapidly identifying and notifying hundreds of air travelers of potential MERS-CoV exposure after the first two travelers with confirmed MERS-CoV infection entered the United States on commercial flights in April and May 2014. CDC continues to refine and improve these processes. Initial contact of potentially exposed travelers was followed by interviews and serologic testing, the results of which will be published in a separate article.
Footnotes
The authors thank Laura Vonnahme, MPH, for her thoughtful insights and support during this investigation. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East Respiratory Syndrome Coronavirus: estimation of pandemic risk. Lancet. 2013;382:694–9. doi: 10.1016/S0140-6736(13)61492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DAT, et al. Hospital outbreak of Middle East Respiratory Syndrome Coronavirus. N Engl J Med. 2013;369:407–16. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Memish ZA, Zumla AI, Al-Hakeem RF, Al-Rabeeah AA, Stephens GM. Family cluster of Middle East Respiratory Syndrome Coronavirus infections. N Engl J Med. 2013;368:2487–94. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 4.Coburn BJ, Blower S. Predicting the potential for within-flight transmission and global dissemination of MERS. Lancet Infect Dis. 2014;14:99. doi: 10.1016/S1473-3099(13)70358-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mangili A, Gendreau MA. Transmission of infectious diseases during commercial air travel. Lancet. 2005;365:989–96. doi: 10.1016/S0140-6736(05)71089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marienau KJ, Burgess GW, Cramer E, Averhoff FM, Buff AM, Russell M, et al. Tuberculosis investigations associated with air travel: U.S. Centers for Disease Control and Prevention, January 2007–June 2008. Travel Med Infect Dis. 2010;8:104–12. doi: 10.1016/j.tmaid.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Nelson K, Marienau K, Schembri C, Redd S. Measles transmission during air travel, United States, December 1, 2008–December 31, 2011. Travel Med Infect Dis. 2013;11:81–9. doi: 10.1016/j.tmaid.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Kim C, Chavez P, Pierce A, Murray A, Sander M, Kenyon C, et al. Rubella contact tracing associated with air travel. Travel Med Infect Dis. 2012;10:48–51. doi: 10.1016/j.tmaid.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Stone SC, Kassinove AS. Exposure to patients with meningococcal disease on aircraft—United States, 1999–2001. Ann Emerg Med. 2001;38:598–9. doi: 10.1067/mem.2001.119344. [DOI] [PubMed] [Google Scholar]
- 10.Leitmeyer K. European risk assessment guidance for infectious diseases transmitted on aircraft—the RAGIDA project. Euro Surveill. 2011;16:19845. pii. [PubMed] [Google Scholar]
- 11.Marienau KJ, Cramer EH, Coleman MS, Marano N, Cetron MS. Flight related tuberculosis contact investigations in the United States: comparative risk and economic analysis of alternate protocols. Travel Med Infect Dis. 2014;12:54–62. doi: 10.1016/j.tmaid.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Johansson MA, Arana-Vizcarrondo N, Biggerstaff BJ, Staples JE, Gallagher N, Marano N. On the treatment of airline travelers in mathematical models. PloS One. 2011;6:e22151. doi: 10.1371/journal.pone.0022151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mangili A, Vindenes T, Gendreau M. Infectious risks of air travel. Microbiol Spectr. 2015;3(5) doi: 10.1128/microbiolspec.IOL5-0009-2015. [DOI] [PubMed] [Google Scholar]
- 14.Neatherlin J, Cramer EH, Dubray C, Marienau KJ, Russell M, Sun H, et al. Influenza A(H1N1)pdm09 during air travel. Travel Med Infect Dis. 2013;11:110–8. doi: 10.1016/j.tmaid.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vogt TM, Guerra MA, Flagg EW, Ksiazek TG, Lowther SA, Arguin PM. Risk of severe acute respiratory syndrome-associated coronavirus transmission aboard commercial aircraft. J Travel Med. 2006;13:268–72. doi: 10.1111/j.1708-8305.2006.00048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olsen SJ, Chang HL, Cheung TY, Tang AF, Fisk TL, Ooi SP, et al. Transmission of the severe acute respiratory syndrome on aircraft. N Engl J Med. 2003;349:2416–22. doi: 10.1056/NEJMoa031349. [DOI] [PubMed] [Google Scholar]
- 17.Regan JJ, Jungerman R, Montiel SH, Newsome K, Objio T, Washburn F, et al. Public health response to commercial airline travel of a person with Ebola virus infection—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(3):63–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East Respiratory Syndrome Coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13:752–61. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watson JT, Hall AJ, Erdman DD, Swerdlow DL, Gerber SI. Unraveling the mysteries of Middle East Respiratory Syndrome Coronavirus. Emerg Infect Dis. 2014;20:1054–6. doi: 10.3201/eid2006.140322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV)—Saudi Arabia [cited 2016 Apr 11] Available from: http://www.who.int/csr/don/23-march-2016-mers-saudi-arabia/en.
- 21.Khan K, Sears J, Hu VW, Brownstein JS, Hay S, Kossowsky D, et al. Potential for the international spread of Middle East Respiratory Syndrome in association with mass gatherings in Saudi Arabia. PLoS Curr. 2013:5. doi: 10.1371/currents.outbreaks.a7b70897ac2fa4f79b59f90d24c860b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carias C, O'Hagan JJ, Jewett A, Gambhir M, Cohen NJ, Haber Y, et al. Exportations of symptomatic cases of MERS-CoV infection to countries outside the Middle East. Emerg Infect Dis. 2016;22:723–5. doi: 10.3201/eid2204.150976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mailles A, Blanckaert K, Chaud P, van der Werf S, Lina B, Caro V, et al. First cases of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infections in France: investigations and implications for the prevention of human-to-human transmission, France, May 2013. Euro Surveill. 2013;18:20502. pii. [PubMed] [Google Scholar]
- 24.Puzelli S, Azzi A, Santini MG, Di Martino A, Facchini M, Castrucci MR, et al. Investigation of an imported case of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection in Florence, Italy, May to June 2013. Euro Surveill. 2013;18:20564. doi: 10.2807/1560-7917.es2013.18.34.20564. pii. [DOI] [PubMed] [Google Scholar]
- 25.Reuss A, Litterst A, Drosten C, Seilmaier M, Bohmer M, Graf P, et al. Contact investigation for imported case of Middle East Respiratory Syndrome, Germany. Emerg Infect Dis. 2014;20:620–5. doi: 10.3201/eid2004.131375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kraaij-Dirkzwager M, Timen A, Dirksen K, Gelinck L, Leyten E, Groeneveld P, et al. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infections in two returning travellers in the Netherlands, May 2014. Euro Surveill. 2014;19:20817. doi: 10.2807/1560-7917.es2014.19.21.20817. pii. [DOI] [PubMed] [Google Scholar]
- 27.Hui DS, Perlman S, Zumla A. Spread of MERS to South Korea and China. Lancet Respir Med. 2015;3:509–10. doi: 10.1016/S2213-2600(15)00238-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. 42 U.S.C., Ch. 6A, Pt. G, §264 (2011)
- 29.Mayfield J. “You did us proud.” U.S. Customs and Border Protection 2011 Aug 2 [cited 2016 May 20] Available from: http://www.cbp.gov/newsroom/spotlights/2011-08-02-040000/you-did-us-proud.
- 30.Customs and Border Protection (US) APIS: Advance Passenger Information System [cited 2016 May 20] Available from: http://www.cbp.gov/travel/travel-industry-personnel/apis2.
- 31.Customs and Border Protection (US) Sample customs declaration form [cited 2014 Jun 6] Available from: http://www.cbp.gov/travel/us-citizens/sample-declaration-form.
- 32.Customs and Border Protection (US) Mobile passport control [cited 2016 May 20] Available from: http://www.cbp.gov/travel/us-citizens/mobile-passport-control.
- 33.Transportation Security Administration (US) Secure Flight Program [cited 2016 May 20] Available from: http://www.tsa.gov/stakeholders/secure-flight-program.
- 34.Centers for Disease Control and Prevention (US) Epi-X: The Epidemic Information Exchange [cited 2016 May 20] Available from: http://www.cdc.gov/epix.
- 35.World Health Organization. International Health Regulations 2005 [cited 2016 May 20] Available from: http://www.who.int/ihr/publications/9789241596664/en.
- 36.Centers for Disease Control and Prevention (US) Middle East Respiratory Syndrome (MERS): interim guidance for healthcare professionals [cited 2016 Apr 11] Available from: http://www.cdc.gov/coronavirus/mers/interim-guidance.html.
- 37.Bialek SR, Allen D, Alvarado-Ramy F, Arthur R, Balajee A, Bell D, et al. First confirmed cases of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection in the United States, updated information on the epidemiology of MERS-CoV infection, and guidance for the public, clinicians, and public health authorities—May 2014. MMWR Morb Mortal Wkly Rep. 2014;63(19):431–6. [PMC free article] [PubMed] [Google Scholar]
- 38.Hunter JC, Nguyen D, Aden B, Al Bandar Z, Al Dhaheri W, Abu Elkheir K, et al. Transmission of Middle East Respiratory Syndrome Coronavirus infections in healthcare settings, Abu Dhabi. Emerg Infect Dis. 2016;22:647–56. doi: 10.3201/eid2204.151615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention (US) Specific laws and regulations governing the control of communicable diseases [cited 2016 Apr 12] Available from: http://www.cdc.gov/quarantine/specificlawsregulations.html.