Abstract
Purpose
To perform an epilepsy surgery on a patient with drug resistant epilepsy secondary to bilateral brain malformation. The patient was a 2-year 9-month-old boy who had congenital bilateral multiple abnormalities. He developed a complex partial seizure at 9 months old. Based on the presurgical evaluations, he underwent a right hemispherotomy.
Results
Brain MRI revealed congenital bilateral polymicrogyria, right schizencephaly, and corpus callosum agenesis. The abnormality was noted to be more severe in the right hemisphere. Diffusion tensor image tractography clearly detected a left pyramidal tract. On the contrary, the right hemisphere did not show a clear pyramidal tract. An interictal EEG showed epileptiform discharges over both hemispheres with right frontotemporal area dominancy. The long-term video-EEG recorded his habitual seizures arising from the right frontal area. Right hemispherotomy led to freedom from seizures and a reduced need for anti-epilepsy drugs.
Conclusions
We report a patient with bilateral MRI and EEG abnormalities with clear DTI laterality who achieved seizure freedom with epilepsy surgery.
Keywords: Bilateral congenital brain malformation, Hemispherotomy, Brain magnetic resonance imaging (MRI), Diffusion tensor image (DTI) tractography, Epilepsy surgery
1. Background
Patients with multiple epileptiform discharges on interictal scalp electroencephalogram (EEG) can present a puzzling issue when making decisions about potential epilepsy surgery because the EEG does not always correctly locate the epilepsy foci. As magnetic resonance imaging (MRI) or positron emission tomography (PET) can also identify epileptic foci for patients with generalized or multiple foci, we sometimes see discordance between presurgical studies. In this case study, we present a patient with medically intractable epilepsy whose brain MRI showed bilateral abnormalities and whose interictal scalp EEG showed multiple independent spike foci (MISF). However, diffusion tensor image (DTI) tractography showed a clear pyramidal tract in the left hemisphere and none in the right hemisphere. We performed right hemispherotomy based mostly on the DTI and ictal EEG findings.
2. Patient and methods
The patient was a 2-year 9-month-old boy. He started to walk at 1 year of age, even though he had slight weakness on the left side of his body. He had developed a twitch of the left arm, leg, and face at 9 months old. At the age of 1 year old, he developed status epilepticus. Carbamazepine (CBZ) was initiated. He developed complex partial seizures, and zonisamide (ZNS) was added to the CBZ. His seizure prodrome included grimacing suddenly as if he felt fears, trying to hug someone near him, and then development of tachypnea. He also exhibited loss of awareness and stiffness of his extremities. Postictally, he either resumed normal responsiveness or fell asleep. These seizures lasted from approximately 10 s to 2 min. Seizure frequency was approximately 50 times per day. Carbamazepine and ZNS did not control his seizures.
3. Magnetic resonance imaging (MRI)
The MRI was performed according to our epilepsy protocol on a 1.5-T scanner. Sequences were angulated perpendicularly or parallel to the longitudinal axis of the hippocampal body on axial and coronal FLAIR. The DTI tractography acquisition parameters were: b-value = 700 s/mm2, 5 b0 volumes, 30 gradient directions, voxel size 2 × 2 × 2 mm3, 64 axial slices, and zero slice gap with saving the 5 b0 volumes separately.
4. Video electroencephalogram (VEEG)
The VEEG was performed until a habitual seizure was captured using the 10–20 international system of electrode placement with reference electrodes using Pz′ (1 cm behind Pz) with simultaneous video recording of the clinical manifestations.
5. Surgery and histopathology
Of significance, the patient had bilateral brain malformations, but the abnormality was more severe on the right hemisphere. Based on his presurgical evaluation, he underwent transsylvian hemispherotomy over the right hemisphere. Right temporal area and parietal area tissues were submitted for histopathological study.
6. Results
6.1. Magnetic resonance imaging (MRI)
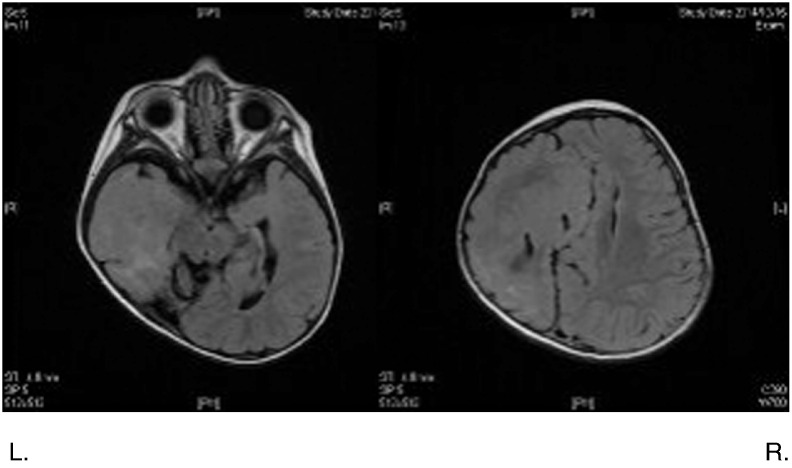
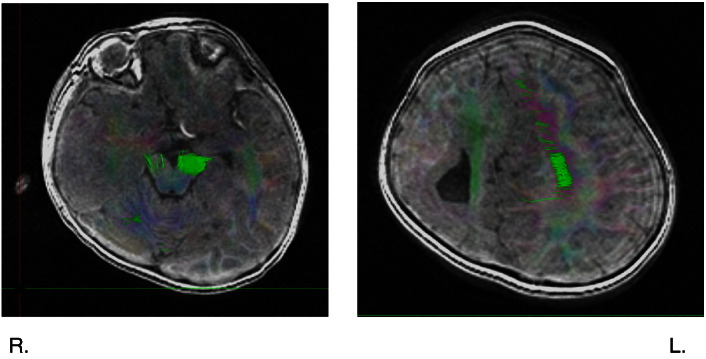
The MRI revealed congenital bilateral polymicrogyria, right schizencephaly, and corpus callosum agenesis. The abnormality was more severe in the right hemisphere (Fig. 1). However, there was clear laterality on DTI tractography. The DTI tractography revealed a clear pyramidal tract in the left hemisphere. On the contrary, it was felt that there were possibly blurred pyramidal tract fibers present in the right hemisphere as well (Fig. 2).
Fig. 1.
Magnetic resonance imaging (MRI).
Brain MRI showing complete absence of sulcation and gyration of the right temporal lobe. The right hemisphere has a more disorganized appearance with a thickened frontal lobe area and a nearly agyric cortex. Abnormally formed bilateral lateral ventricles are seen.
Fig. 2.
Diffusion tensor image (DTI) tractography.
DTI tractography showing a clear bundle of pyramidal tract tissue within the left hemisphere. The right hemisphere did not show a clear pyramidal tract.
6.2. Video electroencephalogram (VEEG)
There were 16 habitual seizures captured over 20 h. All of the events were identical. They started with grimacing suddenly, as if he felt afraid, trying to hug someone near him. He then exhibited left arm tonic posturing with left hand dystonic posturing, quickly followed by right-sided whole-body tonic posturing with his eyes deviated to the left. He also developed tachypnea during the seizures.
Interictally, the EEG showed almost continuous medium-to-high amplitude sharp slow waves over the right frontal area at F4 maximum negativity with a field at F8, Fp2, and T4. There were intermittent medium-amplitude spike-waves over the right frontal, right temporal, left frontal, and left temporal areas, more in the right hemisphere, consistent with multiple independent spike foci (MISF).
Ictally, first there were sharp-slow waves over the right frontal area at F4 followed by a 4- to 5-Hz rhythmicity for several seconds and then spread to Fp2 and F8 followed by diffuse 3- to 4-Hz delta and theta activity over the right hemisphere. These seizures lasted approximately 30–40 s.
6.3. Postoperative course and histopathology
After surgery, the patient obtained freedom from epileptic seizures for more than a year. Currently, he is taking CBZ only. He could sing and smile, which he was not capable of presurgically. Histological examination confirmed the complete lack of sulci and gyri and the lack of operculization of the Sylvian fissure. In particular, the neocortex was reduced in depth, there was no lamination, and the neurons were immature, with few differentiated pyramidal cells.
7. Discussion
Hemispherotomy can be considered for those with seizures arising from one hemisphere where there is a preexisting structural abnormality of that hemisphere. It is particularly suitable for those with a preexisting hemiplegia and/or visual field deficit.
When a child presents with catastrophic hemispheric epilepsy and developmental delay, the detection of contralateral MRI abnormalities is not an absolute contraindication for hemispherotomy. An appropriate selection of surgical candidates and prediction of postoperative outcome are crucial.
The DTI is a powerful tool, which has the ability to characterize abnormalities in epileptic foci and to demonstrate the white matter fibers and tracts participating in the epileptic network by the functional and microstructural alterations associated with seizures [1].
Some authors say that contralateral interictal epileptic discharges were seen in 24 children (56%), which is consistent with previous studies that have reported this kind of abnormality in 36% to 61% of hemispherotomy candidates [2]. Even bilateral epileptic encephalopathy, or epileptic discharges predominating in the unaffected hemisphere, does not necessarily preempt a surgical approach, because 72% to 80% of these patients achieve freedom from seizures. According to Boshuisen [3], unambiguous contralateral MRI abnormalities are associated with seizure recurrence, even though contralateral EEG abnormalities do not negatively influence postsurgical outcome. This unambiguous abnormality on MRIs by visual inspection could be said to be subjective. The definition of the unambiguous MRI findings itself is ambiguous. This unambiguous finding might be explained by DTI tractography, as showed in the paper. The ambiguous case, which means severe hemispherical lesions represented by hemimegalencephaly, and the unambiguous case, which means subtle or minor lesions represented by focal cortical dysplasia, are the same malformation, and the difference lies in timing of mitotic cycles [4]. Although we need more cases to explain the utility of the DTI to distinguish between ambiguous findings and unambiguous findings, DTIs might have great potential to provide additional information about the timing difference of migration disorder and might contribute to selecting epilepsy surgery candidates.
Conflict of interest statement
The authors declare no conflicts of interest.
References
- 1.Luat A.F., Chugani H.T. Molecular and diffusion tensor imaging of epileptic networks. Epilepsia. 2008;49(Suppl. 3):15–22. doi: 10.1111/j.1528-1167.2008.01506.x. [DOI] [PubMed] [Google Scholar]
- 2.Kossoff E.H., Vining E.P., Pillas D.J., Pyzik P.L., Avellino A.M., Carson BS. Hemispherectomy for intractable unihemispheric epilepsy etiology vs outcome. Neurology. 2003;61(7):887–890. doi: 10.1212/01.wnl.0000090107.04681.5b. [DOI] [PubMed] [Google Scholar]
- 3.Boshuisen K., van Schooneveld M.M., Leijten F.S., de Kort G.A., van Rijen P.C., Gosselaar P.H. Contralateral MRI abnormalities affect seizure and cognitive outcome after hemispherectomy. Neurology. 2010;75(18):1623–1630. doi: 10.1212/WNL.0b013e3181fb4400. [DOI] [PubMed] [Google Scholar]
- 4.Sarnat H.B., Philippart M., Flores-Sarnat L., Wei X.C. Timing in neural maturation: arrest, delay, precociousness, and temporal determination of malformations. Pediatr Neurol. 2015;52(5):473–486. doi: 10.1016/j.pediatrneurol.2015.01.020. [DOI] [PubMed] [Google Scholar]