Figure 1.
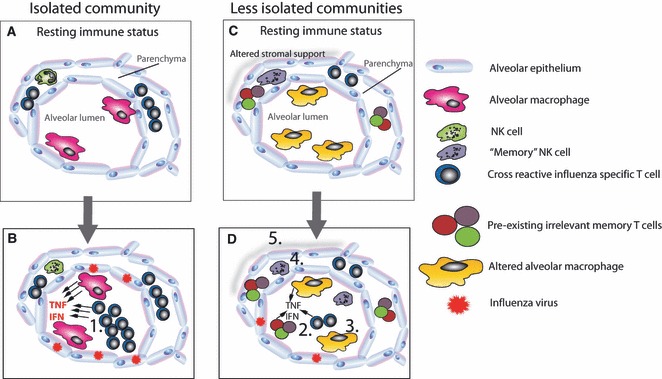
The impact of infection exposure on the development of pathology during the 1918 influenza pandemic. An isolated community will have a less infection‐experienced lung microenvironment. If cross‐reactive T cells are present, they may be over‐represented (A). In the absence of cross‐reactive antibody, influenza will replicate unchecked causing prolonged innate immunity (B). Should specific T cells be present, they expand exponentially because other infections have not adjusted their memory clone size. These too contribute to the inflammatory microenvironment. In an infection‐experienced host (C), the lung at rest is very different. No one T‐cell population is over‐represented, innate “memory” NK cells are present, and airway macrophages are blunted in their responsiveness. During a subsequent influenza infection (D), the whittled down cross‐reactive and bystander T cells enter the lung (2) but are exposed to a reduced inflammatory microenvironment because airway macrophages are less responsive (3) and “memory” NK cells have already reduced the viral load (4). Furthermore, lung remodeling (5) by prior infection has made the lung more resilient.
