Abstract
Candida mediastinitis is a rare complication of open heart surgery with high mortality and morbidity usually associated with C. albicans. We are reporting the case of a 57 year old male who after having a triple coronary artery bypass graft procedure, had mediastinitis caused by Candida famata, a yeast, that had only been reported once before as the causal agent of this condition. It is of vital importance, that future cases be reported, due to the fact that both reported cases have led to patient demise.
Introduction
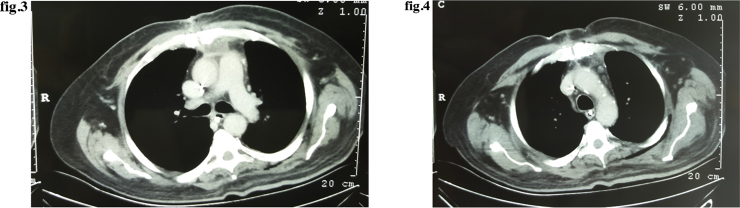
Candida famata (Candida flareri) is a riboflavin overproducing [1], high osmotolerant yeast [2] that produce white to cream colored colonies on yeast extract peptone dextrose (YPD) medium(Fig. 1). This organism was considered to be a teleomorph of Debaryomyces hansenii [3] but was reclassified via rRNA gene intergenic spacer fingerprinting as a unique phylogenetic entity [4].
Fig. 1.
C. famata growth on YPD medium.
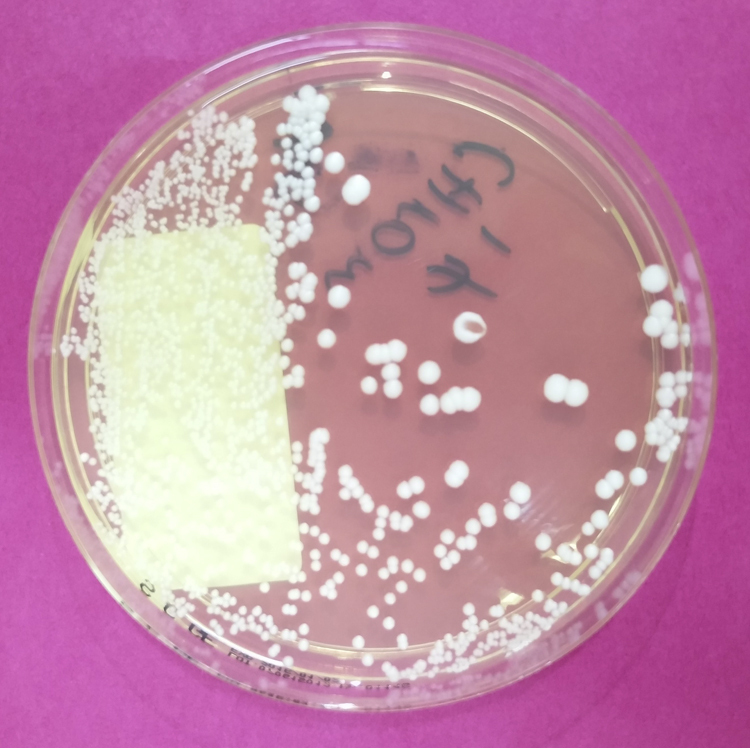
This organism is isolated from many sources, mainly related to food production. It has been detected in the teats of dairy cows [5], various types of cheese [6], prawns [7], feral pigeons [8], wild birds [9] and albino rats [10] among others (Fig. 2).
Fig. 2.
C. famata observed under light microscopy at 40x via KOH staining.
Infections by this agent are mainly observed in patients with depressed immune response, it has been identified as the cause of neonatal sepsis in a low weight preterm infant [11], oral thrush in patients with chronic kidney disease [12], peritonitis in patients with continuous ambulatory peritoneal dialysis [13], invasive infection in stem cell transplant patients [14], candidemia in pediatric cancer patients [15]. This pathogen has also been described as an atypical cause of vaginitis [16], onychomycosis of the hands and feet [17] and cholecystitis [18].
After an exhaustive literary review utilizing Pubmed and Ebscohost databases, we were able to find one previous report of mediastinitis by this agent [19].
We present the case of a 57 year old male who was diagnosed with Candida famata mediastinitis after having coronary artery bypass surgery.
Case report
A 57 year old male with a past medical history of type 2 diabetes, hypertension, a 90 pack year history of smoking and a previous inferior wall myocardial infarction treated with multiple vessel stent placement who was referred to our hospital after failing a dobutamine stress test. After admission an angiography was performed that showed a 90% obstruction of the distal third of the anterior and posterior descending artery as well as an 80–90% occlusion of the medial third of the right main coronary artery. A triple coronary artery bypass grafting (CABG) with saphenous vein graft was performed 29 days after admission, and a mediastinal drain was left in place. During the procedure it was noted that the patient’s pericardium was inflamed therefore he was diagnosed with Dressler syndrome. The patient had multiple post op complications such as a documented cerebral infarction and a difficult airway 24 h post op.
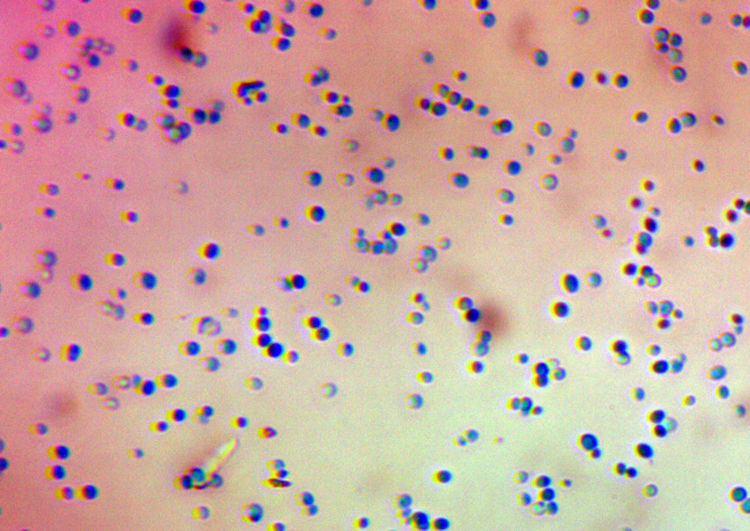
An infected sternotomy site was noted on post op day #7. During status postop day #13 he went into septic shock that was further complicated by acute kidney injury. The patient received a course of vancomycin and piperacillin-tazobactam, which was later switched to imipenem. An obvious thickening of the mediastinum was observed in a chest X-ray and the diagnosis of post-surgical mediastinitis was made. The patient had multiple cultures and a chest computerized tomography (CT) was ordered. The CT revealed small amounts of fluid in the superior mediastinum, fat stranding (Figs. 3 and 4 ), as well as reactive inflammation of the precarinal and prevascular lymph nodes, therefore, surgical drainage via sternotomy was performed.
Figs. 3 and 4.
Fluid level observed on chest CT with thickening of the anterior portion of the superior mediastinum.
The patient grew two different species of fungi from different sources. Candida parapsilosis was identified in the patient’s urine and central venous catheter, and Candida famata was retrieved from the mediastinal drain and the sternotomy wound. Antimicrobial sensitivity test was not performed. The patient was given amphotericin B for 2 days, and after the final cultures were obtained, a course of caspofungin was begun. Unfortunately, the patient had poor therapeutic response, went into multiorgan failure and expired on day 81 of his stay.
Discussion
Candida mediastinitis is a rare complication of open heart surgery [20] with high mortality and morbidity. We were able to identify one previous case report of mediastinitis by C. famata, that patient shared multiple similarities with our patient: coronary artery bypass grafting, a prolonged hospital stay and a fatal outcome to the infection.
There are multiple chemotherapeutic agents that can be utilized to treat C. famata infections. In vitro studies have shown that many agents are active against this yeast. The echinocandin anidulafungin [21] flucytosine, amphotericin B, caspofungin [22] and posaconazole [23] show the greatest antimicrobial activity. Resistance to fluconazole [24], [25] make it a poor choice as first line treatment. The underlying condition and the source of contamination play an important role in the natural progression of the infection. In the case of mediastinitis, surgical drainage and wound debridement are critical components to managing this condition [20].
Due to the rarity of this particular surgical complication, we yet don’t have a clear understanding as to whether or not this species of Candida requires a different therapeutic approach than the more common C. albicans. Hopefully in the future, we will have a clearer picture as to what measures will help reduce mortality in these patients.
Author participation statement
The roles of the authors involved in the elaboration of this paper are as follows:
Dr. Alfredo Sanchez Betancourt: wrote the article, took part in the literary review, and took part in obtaining and processing the information necessary for the writing process.
Dr. Pablo Sibaja Alvarez: was the main reviewer of the manuscript, also helped procure some of the information related to the publication.
Dr. Rolando Arguedas Camacho: took part in editing and review of the manuscript.
Dr. Edward Guevara Espinoza: took part in editing and review of the manuscript.
References
- 1.Voronovsky A.Y., Abbas C.A., Dmytruk K.V., Ishchuk O.P., Kshanovska B.V., Sybirna K.A. Candida famata (Debaryomyces hansenii) DNA sequences containing genes involved in riboflavin synthesis. Yeast. 2004;21(November 15):1307–1316. doi: 10.1002/yea.1182. [DOI] [PubMed] [Google Scholar]
- 2.Dmytruk K.V., Sibirny A.A. Candida famata (Candida flareri) Yeast [Internet] 2012;29(November 11):453–458. doi: 10.1002/yea.2929. [DOI] [PubMed] [Google Scholar]
- 3.Nakase T., Suzuki M. Taxonomic studies on Debaryomyces hansenii (Zopf) Lodder et Kreger-van Rij and related species. I. Chemotaxonomic investigations. J Gen Appl Microbiol. 1985;31:49–69. [Google Scholar]
- 4.Nguyen H.V., Gaillardin C., Neuveglise C. Differentiation of Debaryomyces hansenii and Candida famata by rRNA gene intergenic spacer fingerprinting and reassessment of phylogenetic relationships among D. hansenii, C. famata, D. fabryi, C. flareri (=D. subglobosus) and D. prosopidis: description. FEMS Yeast Res. 2009;9(4):641–662. doi: 10.1111/j.1567-1364.2009.00510.x. [DOI] [PubMed] [Google Scholar]
- 5.Wawron W., Bochniarz M., Szczubiał M. Enzymatic activity of yeasts isolated from the inflamed mammary secretion in dairy cows. Pol J Vet Sci. 2011;14(1):65–68. doi: 10.2478/v10181-011-0009-8. [DOI] [PubMed] [Google Scholar]
- 6.Desnos-Ollivier M., Ragon M., Robert V., Raoux D., Gantier J.-C., Dromer F. Debaryomyces hansenii (Candida famata), a rare human fungal pathogen often misidentified as Pichia guilliermondii (Candida guilliermondii) J Clin Microbiol. 2008;46(October 10):3237–3242. doi: 10.1128/JCM.01451-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brilhante R.S.N., Paiva M.A.N., Sampaio C.M.S., Teixeira C.E.C., Castelo-Branco D.S.C.M., Leite J.J.G. Yeasts from Macrobrachium amazonicum: a focus on antifungal susceptibility and virulence factors of Candida spp. FEMS Microbiol Ecol. 2011;76(2):268–277. doi: 10.1111/j.1574-6941.2011.01050.x. [DOI] [PubMed] [Google Scholar]
- 8.Jang Y.H., Lee S.J., Lee J.H., Chae H.S., Kim S.H., Choe N.H. Prevalence of yeast-like fungi and evaluation of several virulence factors from feral pigeons in Seoul. Korea Lett Appl Microbiol. 2011;52(4):367–371. doi: 10.1111/j.1472-765X.2011.03009.x. [DOI] [PubMed] [Google Scholar]
- 9.Mendes J.F., Albano A.P.N., Coimbra M.A.A., de Ferreira G.F., Gonçalves C.L., Nascente P. Fungi isolated from the excreta of wild birds in screening centers in pelotas, Rs, Brazil. Rev Inst Med Trop Sao Paulo. 2014;56(6):525–528. doi: 10.1590/S0036-46652014000600012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nawange S.R., Singh K., Naidu J., Singh S.M. Naturally acquired systemic dual infection caused by Candida famata (Debaryomyces hansenii) and Candida catenulata in albino rats bred for sale in the market at Jabalpur (Madhya Pradesh), India. Mycoses. 2010;53(2):173–175. doi: 10.1111/j.1439-0507.2008.01686.x. [DOI] [PubMed] [Google Scholar]
- 11.Raturi S., Chandran S., Viswanathan R. A case of Candida famata sepsis in a very low birth weight infant successfully treated with fluconazole following antifungal susceptibility testing. Med J Dr DY Patil Univ. 2015;8(4):528. [Google Scholar]
- 12.Rosa-Garcia La E.D., Miramontes-Zapata M., Sanchez-Vargas L.O., Mondragon-Padilla A. Colonizacion e infeccion bucal por Candida sp. en pacientes diabeticos y no diabeticos con enfermedad renal cronica en dialisis. Nefrologia. 2013;33(6):764–770. doi: 10.3265/Nefrologia.pre2013.Aug.11790. [DOI] [PubMed] [Google Scholar]
- 13.Kerr C.M., Perfect J.R., Craven P.C., Jorgensen J.H., Drutz D.J., Shelburne J.D. Fungal peritonitis in patients on continuous ambulatory peritoneal dialysis. Ann Intern Med Am College Physicians. 1983;99(September 3):334. doi: 10.7326/0003-4819-99-3-334. [DOI] [PubMed] [Google Scholar]
- 14.Wagner D., Sander A., Bertz H., Finke J., Kern W.V. Breakthrough invasive infection due to Debaryomyces hansenii (teleomorph Candida famata) and Scopulariopsis brevicaulis in a stem cell transplant patient receiving liposomal amphotericin B and caspofungin for suspected aspergillosis. Infection. 2005;33(5–6):397–400. doi: 10.1007/s15010-005-5082-4. [DOI] [PubMed] [Google Scholar]
- 15.Devrim I., Demirag B., Yaman Y., Bayram N., Ozdemir F., Kara A. A 7-year study of the distribution of nosocomial candidemia in children with cancer. Turk J Pediatr. 2015;57(3):225–229. [PubMed] [Google Scholar]
- 16.Luis J., Benavides I., Rodríguez D.S., Menchaca R.T., González G., González E.G. Especies de Candida no albicans en la consulta de ginecologia. Med Univ. 2007;9(37):161–165. [Google Scholar]
- 17.Manzano-Gayosso P., Méndez-Tovar L.J., Arenas R., Hernández-Hernández F., Millán-Chiu B., Torres-Rodríguez J.M. Levaduras causantes de onicomicosis en cuatro centros dermatológicos mexicanos y su sensibilidad antifúngica a compuestos azólicos. Rev Iberoam Micol. 2011;28(1):32–35. doi: 10.1016/j.riam.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Sergio P., De Araujo R., Medeiros Z., De Melo F.L. Case Report Candida famata- induced fulminating cholecystitis. Rev Soc Bras Med Trop. 2013;46(August):795–796. doi: 10.1590/0037-8682-0162-2013. [DOI] [PubMed] [Google Scholar]
- 19.Ahmed I.M., Gupta A., Gould K., Clark S.C. A fatal fungus. Ann Thorac Surg. 2005;80(August 2):723–724. doi: 10.1016/j.athoracsur.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 20.Glower D.D., Douglas J.M., Gaynor J.W., Jones R.N., Oldham H.N. Candida mediastinitis after a cardiac operation. Ann Thorac Surg Soc Thorac Surg. 1990;49(1):157–163. doi: 10.1016/0003-4975(90)90382-g. [DOI] [PubMed] [Google Scholar]
- 21.Arévalo M.P., Carrillo-Muñoz A.J., Salgado J., Cardenes D., Brió S., Quindós G. Antifungal activity of the echinocandin anidulafungin (VER002, LY-303366) against yeast pathogens: a comparative study with M27-A microdilution method. J Antimicrob Chemother. 2003;51(1):163–166. doi: 10.1093/jac/dkg018. [DOI] [PubMed] [Google Scholar]
- 22.Beyda N.D., Chuang S.H., Jahangir Alam M., Shah D.N., Ng T.M., McCaskey L. Treatment of Candida famata bloodstream infections: case series and review of the literature. J Antimicrob Chemother. 2013;68(2):438–443. doi: 10.1093/jac/dks388. [DOI] [PubMed] [Google Scholar]
- 23.Pfaller M.A., Diekema D.J., Messer S.A., Boyken L., Hollis R.J., Jones R.N. In vitro activities of voriconazole, posaconazole, and four licensed systemic antifungal agents against Candida species infrequently isolated from blood. J Clin Microbiol. 2003;41(1):78–83. doi: 10.1128/JCM.41.1.78-83.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barchiesi F., Tortorano A.M., Falconi Di Francesco L., Cogliati M., Scalise G., Viviani M.A. In-vitro activity of five antifungal agents against uncommon clinical isolates of Candida spp. J Antimicrob Chemother. 1999;43(2):295–299. doi: 10.1093/jac/43.2.295. [DOI] [PubMed] [Google Scholar]
- 25.Zuluaga Rodriguez A., de Bedout Gomez C., Agudelo Restrepo C.A., Hurtado Parra H., Arango Arteaga M., Moreno Angela Restrepo. Sensibilidad a fluconazol y voriconazol de especies de Candida aisladas de pacientes provenientes de unidades de cuidados intensivos en Medellin, Colombia (2001–2007) Rev Iberoam Micol. 2010;27(3):125–129. doi: 10.1016/j.riam.2010.04.001. [DOI] [PubMed] [Google Scholar]