Abstract
Severe forms of Coats' disease are often associated with total retinal detachment, and a differential diagnosis from retinoblastoma is critically important. In such eyes, laser- and/or cryoablation is often ineffective or sometimes impossible to perform. We report a case of advanced Coats' disease in which a rapid pathological examination of subretinal fluid was effective for the diagnosis, and external subretinal drainage combined with vitrectomy was effective in preserving the eye.
Keywords: Coats' disease, Retinoblastoma, Vitrectomy, Rapid pathological examination
Introduction
Coats' disease is characterized by telangiectatic and aneurysmal retinal vessels with retinal exudation and detachment. The conventional treatments of Coats' disease include laser photocoagulation and/or cryotherapy to the aneurysms and avascular retina in the early to middle stages. In the late stages with neovascular glaucoma, painful eyes are often enucleated [1].
In eyes suspected to have Coats' disease, a differential diagnosis from a retinoblastoma is critically important prior to any invasive therapy. This is because advanced Coats' disease can resemble exophytic retinoblastoma [2]. Considering the risk of a misdiagnosis and the low probability of preserving normal vision, eyes with advanced Coats' disease are sometimes enucleated even though the possibility of preserving the eye by surgical treatment exists.
Case Report
The patient was a 16-month-old boy whose parents noticed esotropia and a white pupil in his right eye at 1 year of age. He had visited 3 hospitals before he was finally referred to our hospital. At the first visit, the patient was noted to be esotropic with a deviation of the right eye. Visual acuity was not measurable because the patient was too young. The anterior segment of the right eye was normal by slit-lamp examinations, but a totally detached retina was observed. Because the detached retina was close to the lens, the peripheral retina could not be observed (fig. 1). There were no abnormal findings in the left eye. B-mode ultrasonography showed a diffuse, high echo area in the vitreous cavity with no apparent sign of calcification (fig. 2). The CT image that had been taken at a previous hospital 1 month earlier showed no evidence of calcification in the right eye (fig. 2). The MRI evaluations taken at 1 of the 2 previous hospitals showed high-intensity signals in the T1-weighted images and low-intensity signals in the T2-weighted images in the vitreous body of the right eye. However, high-intensity signals were observed in the T2-weighted images in the same area on the second MRI, which was taken 3 months after the first MRI examination (fig. 3). No evidence of a mass was seen in both eyes on the MRIs. He was born full-term without any abnormality. There was no positive family history of any eye diseases, and no systemic abnormality was found.
Fig. 1.
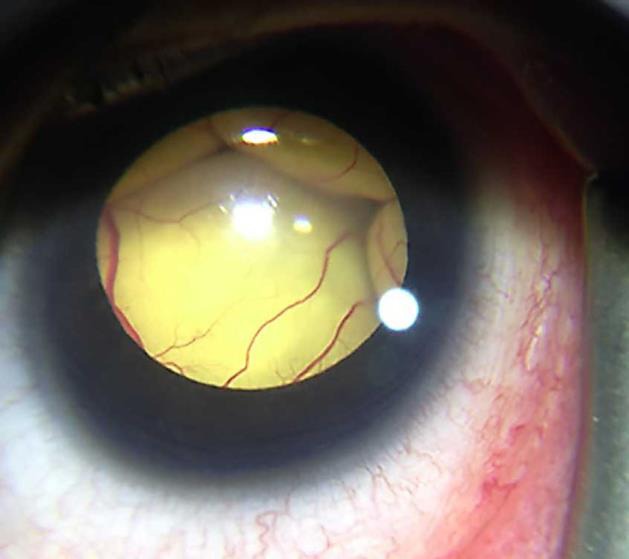
Anterior segment photograph at the first visit showing a totally detached retina in contact with the posterior surface of the lens. The peripheral retina could not be observed.
Fig. 2.
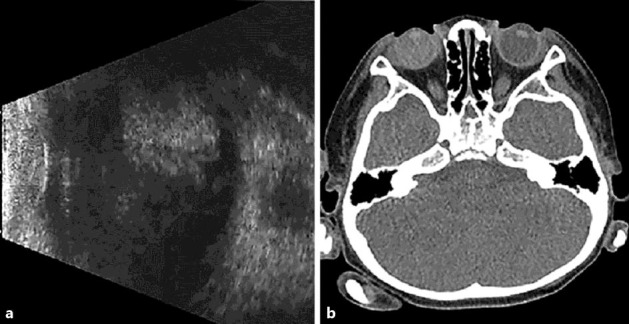
a B-mode echography of the right eye shows a high echo area in the vitreous cavity. b CT shows no evidence of calcification or tumor structure.
Fig. 3.
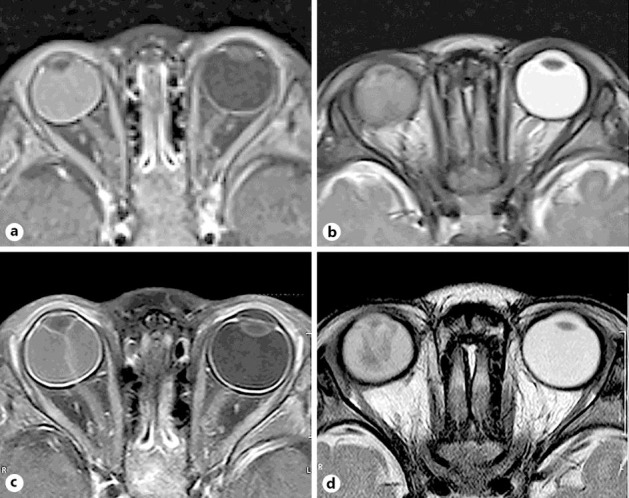
MRIs taken at two different periods. T1 (a) and T2 (b) images taken 3 months before the first visit show a hyperintense lesion and a slightly hypointense lesion in the subretinal space, respectively. Both T1 (c) and T2 (d) images taken at the first visit show hyperintense lesions in the subretinal space. Tumor structure is not observed in the eye.
Surgery was performed for exudative retinal detachment 2 months after the first visit to our hospital. First, external subretinal fluid (SRF) drainage was performed, and SRF was submitted for a rapid pathological examination, so this was a diagnostic procedure. The examination showed many histiocytes and a small number of epithelial cells but no signs of malignancy. Second, lens-sparing vitrectomy was performed, and the retina was reattached under perfluoro-n-octane. Thus, the fundus, especially the peripheral area, could be seen better, and the clinical characteristics of Coats' disease, including dilated retinal vessels, numerous microaneurysms, and intra- and subretinal exudates became visible (fig. 4). Endophotocoagulation was performed on the microaneurysms and the presumably avascular retina near the abnormal vessels. At the end of vitrectomy, 0.5 mg of bevacizumab was injected intravitreally.
Fig. 4.
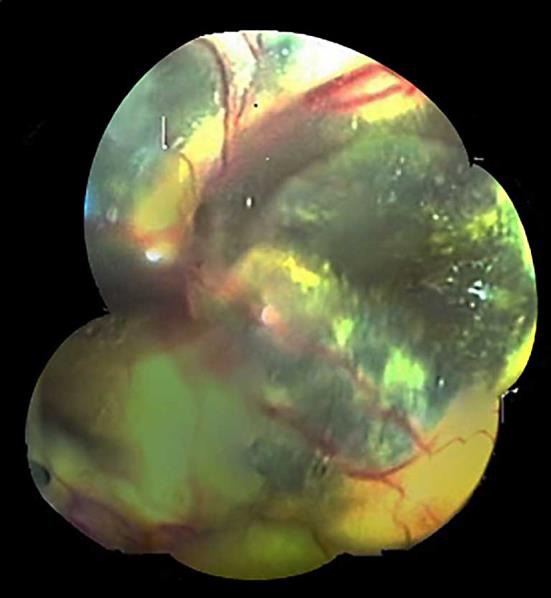
Fundus photograph of the right eye during the first operation under perfluoro-n-octane. Dilated retinal vessels, numerous microaneurysms, and intra- and subretinal exudates became visible.
Postoperatively, the posterior retina was reattached; however, the dilated retinal vessels and peripheral subretinal exudates had not improved even after 3 months.
A reoperation with similar techniques to the first surgery was performed (fig. 5).
Fig. 5.

Fundus photograph of the right eye during the second operation under perfluoro-n-octane. The amount of exudates were reduced.
Three months after the reoperation, a reduction in SRF and exudates was observed. Thereafter, the condition of the eye remained unchanged during the 11 months of follow-up.
Discussion
Severe Coats' disease can easily be misdiagnosed as retinoblastoma [3]. This is especially true when media opacity or a total bullous retinal detachment makes the visibility of the retina difficult or impossible [4]. Previous histological studies have reported that 95% of typical retinoblastomas are calcified [5]. However, atypical retinoblastomas which are neither calcified nor have tumor characteristics also exist [5]. CT scans have a sensitivity of 96% in detecting the calcification in retinoblastoma [6]. Typical MRI findings of retinoblastomas are high-intensity signals in T1-weighted images and low-intensity signals in T2-weighted images [4]. On the other hand, the typical MRI findings in Coats' disease are high-intensity signals in both T1- and T2-weighted images [7].
In our case, the characteristics of Coats' disease were difficult to detect ophthalmoscopically because of the bullous retinal detachment. The CT images did not show any signs of calcification; however, the first MRIs showed features consistent with a retinoblastoma. The second MRI evaluation at the second hospital showed features consistent with Coats' disease. Lai et al. [7] reported a case of Coats' disease in which MRI showed low signal intensity in the T2-weighted images. They postulated that T2-weighted MRIs may vary depending on the nature of the subretinal exudates, which can change during the natural course of the disease process.
The possibility of a retinoblastoma in our case was considered to be low due to the following reasons: first, there was no clear mass lesion in the MRI findings, and the T2-weighted images of the vitreous cavity showed a change in signal intensities; second, no sign of calcification was noted on the CT scans; and third, no tumor mass was detected by ophthalmoscopy and ultrasonography. Because a retinoblastoma could not be completely excluded, we used a rapid pathological examination of SRF to ascertain the diagnosis. As a result, no signs of malignancy were detected. In addition, the removal of SRF made the observation of the peripheral retina better, and typical features of Coats' disease became visible.
In our case, reoperation was necessary because there was significant SRF even at 3 months after surgery. The reason for this is unclear, however, and we consider that the presence of extensive subretinal exudates hindered the complete drainage of SRF regardless of multiple SRF drainage procedures. In addition, it is possible that laser ablation during primary vitrectomy was not enough to decrease the disease activity.
Several authors have reported that vitrectomy with posterior retinotomy, the use of intraocular silicone oil or gas, and scleral buckling were useful in treating eyes with Coats' disease [8, 9]. Adams et al. [2] recommend less invasive treatments consisting of pars plana vitreous infusion, sclerotomy, and external SRF drainage, followed by laser ablation and/or cryopexy for the treatment of Coats' disease. With regard to the surgical technique, SRF is usually drained internally through an intentional or preexisted retinal hole in eyes with rhegmatogenous retinal detachment. However, in eyes with total retinal detachment associated with Coats' disease, the presence of inflammation may induce severe proliferative vitreoretinopathy after surgery if internal SRF drainage and gas or silicone oil tamponade are performed. Therefore, it is strongly recommended that SRF should be drained externally.
Conclusions
In the treatment of severe Coats' disease with total retinal detachment, although careful consideration should be given to the possibility of tumor cell dissemination, a combination of external SRF drainage and a rapid pathological examination of the fluid may be beneficial both for diagnosis and preserving the eye.
Statement of Ethics
The subject of this case report has given informed consent for the publication of this article and the associated photographs.
Disclosure Statement
No conflicting relationship exists for any author.
References
- 1.Shields JA, Shields CL. Review: coats disease: the 2001 LuEsther T. Mertz lecture. Retina. 2002;22:80–91. doi: 10.1097/00006982-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Adam RS, Kertes PJ, Lam WC. Observations on the management of Coats' disease: less is more. Br J Ophthalmol. 2007;91:303–306. doi: 10.1136/bjo.2006.103382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ray R, Baranano DE, Hubbard GB. Treatment of Coats' disease with intravitreal bevacizumab. Br J Ophthalmol. 2013;97:272–277. doi: 10.1136/bjophthalmol-2012-302250. [DOI] [PubMed] [Google Scholar]
- 4.Grabowska A, Calvo JP, Fernandez-Zubillaga A, Rios JC, Gomez JA. A magnetic resonance imaging diagnostic dilemma: diffuse infiltrating retinoblastoma versus Coats' disease. J Pediatr Ophthalmol Strabismus. 2010;47:e1–e3. doi: 10.3928/01913913-20100818-10. [DOI] [PubMed] [Google Scholar]
- 5.Bhatnagar R, Vine AK. Diffuse infiltrating retinoblastoma. Ophthalmology. 1991;98:1657–1661. doi: 10.1016/s0161-6420(91)32072-4. [DOI] [PubMed] [Google Scholar]
- 6.Galluzzi P, Hadjistilianou T, Cerase A, De Francesco S, Toti P, Venturi C. Is CT still useful in the study protocol of retinoblastoma? AJNR Am J Neuroradiol. 2009;30:1760–1765. doi: 10.3174/ajnr.A1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai WW, Edward DP, Weiss RA, Mafee MF, Tso MO. Magnetic resonance imaging finding in a case of advanced Coats' disease. Ophthalmic Surg Lasers. 1996;27:234–238. [PubMed] [Google Scholar]
- 8.Yoshizumi MO, Kreiger AE, Lewis H, Foxman B, Hakakha BA. Vitrectomy techniques in late-stage Coats'-like exudative retinal detachment. Doc Ophthalmol. 1995;90:387–394. doi: 10.1007/BF01268124. [DOI] [PubMed] [Google Scholar]
- 9.Deveny RG. The use of perfluorocarbon liquid in the surgical repair of a bullous retinal detachment secondary to Coats' disease. Can J Ophthalmol. 1998;33:385–386. [PubMed] [Google Scholar]


