Abstract
High-quality relationships may be protective for family caregivers. This study focuses on relationship quality categories (supportive and ambivalent) in spouse caregivers in cancer home hospice. The goals of this article are to, first, describe relationship quality categories among end-of-life caregivers and, second, test the effects of relationship quality categories on caregiver burden and distress within a stress process model. Using questionnaire data collected at entry to home hospice, we found relationship quality categories were proportionally similar to those seen in noncaregiver older adults. Relationship quality significantly predicted caregiver burden, which completely mediated the relationship between caregiver relationship quality and distress. Caregivers whose social contexts place them at risk for greater distress may benefit from increased clinical attention or intervention.
Keywords: Burden, cancer, caregiving, distress, end of life, relationship quality
Despite a 5-year, 68% relative survival rate for cancer, and improvements in screening, detection, and treatment, the lifetime likelihood of developing this disease is one in two for men and one in three for women. Cancer is still the second most common cause of death in the U.S. (American Cancer Society, 204). Cancer impacts not only those diagnosed but also family members, especially those who become caregivers (Hagedoorn, Sanderman, Bolks, Tuinstra, & Coyne1, 2008; Mitschke, 2008; Resendes & McCorkle, 2006). Although many benefit from and are able to find meaning in providing care (Hasson-Ohayon et al., 2013; Kim, Carver, Deci, & Kasser, 2008), care provision has been recognized as stressful both emotionally and physically (Chentsova-Dutton et al., 2000; Girgis, Lambert, Johnson, Waller, & Currow, 2013; Haley, LaMonde, Han, Narramore, & Schonwetter, 2001; Romito, Goldzweig, Cormio, Hagedoorn, & Andersen, 2013) and is linked to higher incidences of anxiety and depression, weakened immune responses, a greater likelihood of long-term medical problems, and higher mortality rates (Chentsova-Dutton et al., 2000; Decker & Young, 1991; Grunfeld et al., 2004; Hebert, Arnold, & Schulz, 2007; Schulz & Beach, 1999; U.S. Department of Health and Human Services Office on Women’s Health, 2011). Family caregivers of patients with advanced cancer are at even greater risk for adverse outcomes based on heightened emotional concerns and increased need for physical care for patients in advanced stages of the disease (Kissane, Bloch, Burns, McKenzie, & Posterino, 1994; Kurtz, Given, Kurtz, & Given, 1994).
Relationship quality as a factor for caregiver health outcomes
Because not all caregivers experience negative health effects from providing care, other factors are likely at play. High-quality relationships have been linked to improved health outcomes in the general population (Uchino, Holt-Lunstad, Uno, Campo, & Reblin, 2007). Specifically, supportive relationships have been shown to ameliorate the specific health risk factors associated with caregiving and to improve stress response and psychological and physical outcomes, including depression, immune function, and all-cause mortality (Berkman, Glass, Brissette, & Seeman, 2000; Cohen, 1988; Uchino, 2004; Uchino, Kiecolt-Glaser, & Cacioppo, 1994), consistent with the buffering hypothesis (Cohen & Wills, 1985). High-quality relationships have also been linked to better care provision and patient outcomes (Williamson & Shaffer, 2000). Taken together, this research suggests the importance of considering the role of relationship quality when investigating caregiver health at end of life.
Despite these promising links, the impact of relationship quality at end of life has not been fully explored (Stajduhar et al., 2010). Research showing that spouses are often a primary source of an individual’s support and that existing interaction patterns are carried into periods of caregiving (Family Caregiver Alliance, 2012; Fromme et al., 2005; Salmon et al., 2003) suggests that a supportive spousal relationship would be beneficial during caregiving. However, the added complexity of the spouse’s impending death may complicate outcomes (McLean & Jones, 2007). Some research from the perspective of cancer patients on the role of relationship quality has been conducted (Ballantyne, 2004; Manne & Glassman, 2000; Manne, Pape, Taylor, & Dougherty, 1999), but the effects of relationship quality from the perspective of cancer caregivers has been understudied. Within the limited research that has been done on relationship quality at end of life, findings have been mixed in terms of the potential benefit of high-quality relationships. For example, one study on caregivers of patients with late-stage cancer found little evidence for caregiver–patient relationship quality influencing caregiver burden; however, researchers did find that caregivers’ high-quality relationships with other social ties alleviated burden (Francis, Worthington, Kypriotakis, & Rose, 2010). In contrast, other research found that caregiver–patient relationship quality was the critical element in predicting caregiver burden and satisfaction (Snyder, 2000).
Measurement of relationship quality
Mixed findings regarding the role of relationship quality may be due to the different operationalizations of the concept across and even within studies (Francis et al., 2010; Holt-Lunstad, Smith, & Layton, 2010; Wittenberg-Lyles, Washington, Demiris, Oliver, & Shaunfield, 2014). To obtain a clearer and more accurate pattern of results, some researchers have suggested that the assessment of relationship quality should be more finely grained than common unidimensional measures (Holt-Lunstad et al., 2010). Positive and negative aspects of relationships have been found to be separable dimensions (Finch, Okun, Barrera, Zautra, & Reich, 1989; Fiore, Becker, & Coppel, 1983) and hence can co-occur. By using multidimensional assessment, we can identify two different relationship types commonly seen in close relationships (Campo et al., 2009; Vaughn & Reblin, 2010) that previously would have been seen as the same type of high-quality relationship.
As seen in Figure 1, a supportive relationship is one perceived to have high positivity and low negativity or very helpful when one is in need of support and not at all upsetting. An ambivalent relationship is also perceived to have high positivity or seen as helpful when support is needed. It also involves the co-occurrence of high negativity and is perceived as somewhat upsetting. Although both supportive and ambivalent relationships have high positivity, the concurrent high levels of negativity in ambivalent relationships appear to have unique, detrimental influences on health outcomes (Uchino, 2004; Uchino et al., 2007). Also included in Figure 1 are indifferent and aversive relationships. Indifferent ties tend to be less important members of our social networks. Contact is often minimized with aversive ties (Uchino, Holt-Lunstad, Uno, & Flinders, 2001). Thus, neither is frequently seen in close relationships such as among spouses (Campo et al., 2009; Vaughn & Reblin, 2010), making them outside the scope of the current study. We propose to use this multidimensional framework to describe ambivalent and supportive relationships at the end of life and to test the effects of caregiver relationship quality categories on burden and distress (specifically anxiety and burden).
Figure 1.
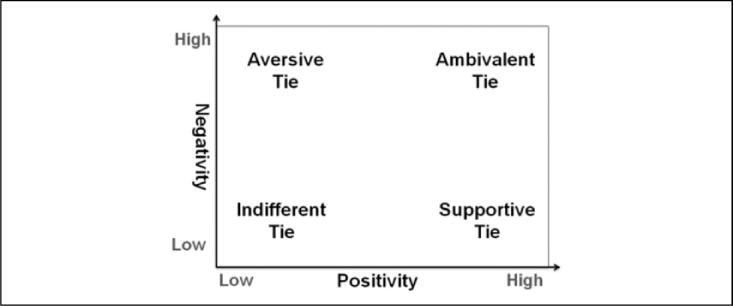
Relationships in two dimensions. Adapted from “Heterogeneity in the social networks of young and older adults: Prediction of mental health and cardiovascular reactivity during acute stress,” by Uchino, B. N., Holt-Lunstad, J., Uno, D., and Flinders, J. B., 2001, Journal of Behavioral Medicine, 24, 361–382.
Objective 1: Describing relationships at end of life
Even though one might expect higher relationship quality among spouses maintaining a relationship into old age (Levenson, Carstensen, & Gottman, 1993), ambivalent relationships in spouses are prevalent in the broader population (Campo et al., 2009; Uchino et al., 2013), and previous research suggests that relationship quality tends to be relatively stable over time (Campo et al., 2009; Vaughn & Reblin, 2010). Additionally, obligation may keep spouses with higher levels of negativity together at end of life (Feinberg, Wolkwitz, & Goldstein, 2006; Neufeld & Harrison, 1998). The existing relationship quality, along with its history of conflict (Kramer, Kavanaugh, Trentham-Dietz, Walsh, & Yonker, 2010) and the impact of caregiving itself on the relationship (Lawrence, Tennstedt, & Assmann, 1998; Walker, Shin, & Bird, 1990) builds a social environment that can have implications for caregivers’ ongoing interactions and their psychological health. However, to our knowledge, there have been no studies to date describing relationship quality using both positive and negative dimensions in couples at end of life. Therefore, the first objective of this research was to determine the presence of perceived supportive and ambivalent relationships of home hospice cancer spouse caregivers.
Objective 2: Testing effects of relationship quality on psychological health
Pearlin, Mullan, Semple, and Skaff (1990) have proposed a conceptual model of caregiving as a stress process that outlines the interrelationships of domains of factors pertaining to caregiver stress. As seen in Figure 2, we have adapted this model to test how relationship quality, along with the covariates of caregiver sex and relationship length, as contextual factors, impacts caregivers’ psychological health outcomes—specifically caregiver anxiety and depression, with possible mediation through stress, as measured by caregiver burden. For the purposes of this preliminary test of relationship quality, we did not include other mediators.
Figure 2.
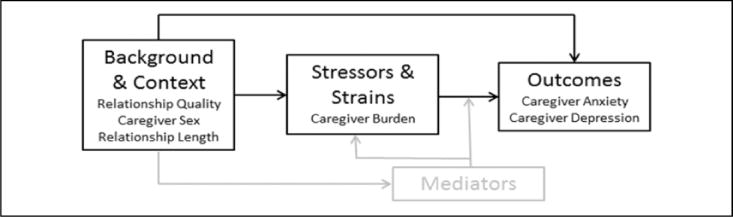
Conceptual model. Adapted from “Caregiving and the stress process: An overview of concepts and their measures,” by Pearlin, L. I., Mullan, J. T., Semple, S. J., and Skaff, M. M., 1990, Gerontologist, 30, 583–594.
Despite the lack of research focusing specifically on spouse caregiver’s supportive and ambivalent relationship quality and psychological health at end of life, we can extrapolate potential effects from research on the broader population. Thus, we hypothesize that the protective effects of supportive relationships and the deleterious effects of ambivalent relationships on psychological health carry through to this stage of life. However, because of the complexity of relationships at end of life, the expected outcomes may be reversed. For instance, the traditional viewpoint suggests spouse caregivers with supportive relationships may find more meaning in providing support through death (Li & Loke, 2013), reducing feelings of burden and protecting against anxiety and depression in this group. A contrasting viewpoint would suggest spouse caregivers with supportive relationships may be more adversely affected by the suffering of their dying partners (Monin & Schulz, 2009), increasing feelings of burden, anxiety, and depression. Because of this conflicting evidence, beyond describing the types of relationships found at end of life, the second objective of this study was to assess how relationship quality affects spouse cancer caregiver burden, anxiety, and depression upon entry to home hospice care. We hypothesized that, controlling for caregiver sex and length of relationship, relationship quality category (supportive or ambivalent) would significantly predict caregiver burden, anxiety, and depression at entry to home hospice.
Method
Cancer patients and their self-identified spouse caregivers were recruited upon enrollment to home hospice care as part of an ongoing larger study, Partners in Hospice Care (P01CA138317; PI Mooney). Within 1 week of enrollment, caregivers completed demographic information and questionnaires to assess co-occurring positive and negative relationship quality (Social Relationships Index [SRI]; Campo et al., 2009), anxiety (Hospital Anxiety and Depression Scale [HADS]; Zigmond & Snaith, 1983), depression (Geriatric Depression Scale–Short Form [GDS-SF]; Sheikh & Yesavage, 1986), and burden (Caregiver Reaction Assessment [CRA]; C. Given et al., 1992). This study was approved by the University Institutional Review Board and hospice administrators.
Participants
This subsample included 131 caregivers who were enrolled in the larger study and who completed questionnaires at enrollment. In our sample, all couples were heterosexual and were either married or living as married. Participants were from 10 hospice agencies located in three metropolitan areas in the U.S., representing the Midwest, the Intermountain West, and the Northeast. A priori power calculations indicated that a sample of this size would generate excellent precision of estimation, achieving a power of 0.95. Eligibility criteria for the larger study (and therefore this sample) included adult family self-identified caregivers of patients with a histological diagnosis of cancer admitted to a participating home care hospice program. Other criteria included English speaking/writing, daily access to a telephone, assignment to a participating hospice nurse, and cognitive and physical ability to participate.
Measures
A demographic questionnaire, including assessment of patient and caregiver age, sex, and length of relationship, was completed at enrollment.
The SRI (Campo et al., 2009) was used to assess caregiver perception of relationship quality. In this scale, caregivers rate their relationships in terms of how helpful and upsetting they saw their partner to be (1 = not at all, 6 = extremely). The SRI also includes a measure of importance of the relationship (1 = not at all, 6 = extremely). Helpful (positivity) and upsetting (negativity) scores are then used to assign a relationship type. A supportive relationship is defined as one with positivity rated as 2 or greater and negativity of 1 (at least a little helpful and not at all upsetting). An ambivalent relationship is defined as one with both positivity and negativity rated as 2 or greater (at least a little helpful and at least a little upsetting). Relationship categories defined using these absolute cutoffs are used within this analysis for consistency with our model (i.e., focus on the presence or absence of positivity/negativity) and for consistency with prior research to make comparisons with broader, noncaregiving populations. The SRI has a two-factor structure (i.e., positivity and negativity) and good psychometric properties including convergent and divergent validity and test–retest reliability (Campo et al., 2009). Relationship categories also show good predictive validity on psychological well-being and physical health outcomes (e.g., Holt-Lunstad, Uchino, Smith, Olsen-Cerny, & Nealey-Moore, 2003; Uchino et al., 2001).
Caregiver burden was assessed with the 24-item, 5-subscale CRA (C. Given et al., 1992). The five subscales include caregiver self-esteem (e.g., “Caring for my spouse makes me feel good”), burden from lack of family support (e.g., “It is very difficult to get help from my family in taking care of my spouse”), financial burden (e.g., “It’s difficult to pay for my spouse’s health needs and services”), scheduling burden (e.g., “My activities are centered around care for my spouse”), and health burden (e.g., “My health has gotten worse since I’ve been caring for my spouse”). This instrument has well-documented validity and reliability (B. Given & Given, 1992; B. Given et al., 2004; C. Given et al., 1992; Nijboer et al., 2000; Stommel, Wang, Given, & Given, 1992). In the current study, Cronbach’s α was .74. Mean scores were calculated for each subscale.
The HADS anxiety subscale (Zigmond & Snaith, 1983) was used to measure self-reported caregiver anxiety. This 7-item scale has been found to perform well as a test for such symptoms in caregivers of cancer patients, including at end of life (Gough & Hudson, 2009; Lambert, Pallant, & Girgis, 2011). This scale has good screening properties (specificity of 0.78 and sensitivity of 0.9). A summed score of greater than 8 is an established cutoff for anxiety in the general population, with a score of 11 or greater defined as clinically abnormal (Bjelland, Dahl, Haug, & Neckelmann, 2002). The Cronbach’s α for this scale in the current study was .88.
Caregiver depression was assessed using the GDS-SF (Sheikh & Yesavage, 1986), a 15-item version of the longer GDS. The short version was developed with items that produced the greatest item–total correlations and is as effective as the longer form in discriminating depressed from nondepressed older adults (r = 0.84). Summed scores greater than 5 are suggestive of depression, and scores greater than 10 almost always indicate depression (Sheikh & Yesavage, 1986; Yesavage et al., 1982). In the current study, Cronbach’s α was .83.
Analysis
Descriptive statistics, independent t, and χ2 tests were used to describe and compare caregiver supportive and ambivalent relationships. Maximum likelihood structural equation modeling in MPlus software was used to determine the relationships between measured variables of anxiety, depression, and relationship quality and the latent variable of burden, controlling for caregiver gender, and length of relationship. Based on the conceptual model outlined by Pearlin et al. (1990), as well as the broader research literature, we proposed a model in which contextual variables, specifically relationship quality, would predict outcome variables of caregiver state depression and anxiety (where depression and anxiety were correlated with each other), with potential mediation through stress variables, as measured by caregiver burden. We hypothesized that, controlling for caregiver sex and length of relationship, relationship quality category (supportive or ambivalent) would significantly predict caregiver burden, anxiety, and depression at entry to home hospice. Both indirect and direct relationships can be tested using structural equation modeling, making it possible to identify possible mediation of burden between relationship quality, anxiety, and depression.
Results
Demographics
All demographics and questionnaire means for the overall sample and split between ambivalent and supportive groups are presented in Table 1. Caregivers were 92% White and 35% male. Caregivers were, on average, 65 years old (SD = 10.74), and patients were, on average, 68 years (SD = 11.27). Couples were married or coresiding a mean of 35.9 years (SD = 17.76). Most caregivers were relatively well educated (over 75% had at least some college) but had a wide range in income. Caregivers reported high levels of anxiety and depression. The mean anxiety score was 9.89 (SD = 2.41), and most caregivers fell between the established cutoff for anxiety in the general population (HADS score of 8) and the score defined as clinically anxious (HADS score of 11). The mean depression score was 5.49 (SD = 2.55), which falls above the score suggestive of depression (GDS score of 5).
Table 1.
Caregiver means and demographics.
| Variables | All
|
Ambivalent
|
Supportive
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Freq | % | N | Freq | % | N | Freq | % | |||||||
| Caregiver male | 131 | 46 | 35 | 90 | 29 | 32 | 41 | 17 | 42 | ||||||
| Patient male | 131 | 86 | 65 | 90 | 62 | 69 | 41 | 24 | 59 | ||||||
| Caregiver White | 131 | 120 | 97 | 90 | 80 | 96 | 41 | 40 | 97 | ||||||
| Patient White | 131 | 127 | 97 | 90 | 87 | 97 | 41 | 40 | 97 | ||||||
| Education | |||||||||||||||
| Less than high school | 131 | 2 | 1 | 90 | 2 | 2 | 41 | 0 | 0 | ||||||
| High school graduate | 131 | 29 | 22 | 90 | 21 | 23 | 41 | 8 | 20 | ||||||
| Some college | 131 | 44 | 34 | 90 | 29 | 32 | 41 | 15 | 37 | ||||||
| College graduate | 131 | 23 | 18 | 90 | 16 | 18 | 41 | 7 | 17 | ||||||
| Some graduate school | 131 | 8 | 6 | 90 | 5 | 6 | 41 | 3 | 7 | ||||||
| Graduate degree | 131 | 25 | 19 | 90 | 17 | 19 | 41 | 8 | 19 | ||||||
| Income | |||||||||||||||
| Less than US$10,000 | 131 | 3 | 2 | 90 | 3 | 3 | 41 | 0 | 0 | ||||||
| US$10,000–US$24,999 | 131 | 15 | 12 | 90 | 8 | 9 | 41 | 7 | 17 | ||||||
| US$25,000–US$39,999 | 131 | 18 | 14 | 90 | 11 | 12 | 41 | 7 | 17 | ||||||
| US$40,000–US$49,999 | 131 | 15 | 12 | 90 | 11 | 12 | 41 | 4 | 10 | ||||||
| US$50,000–US$74,999 | 131 | 32 | 24 | 90 | 25 | 28 | 41 | 7 | 17 | ||||||
| US$75,000+ | 131 | 32 | 24 | 90 | 22 | 24 | 41 | 10 | 24 | ||||||
| Prefer not to answer | 131 | 16 | 12 | 90 | 10 | 11 | 41 | 6 | 15 | ||||||
|
| |||||||||||||||
| Variables | N | Min | Max | Mean | SD | N | Min | Max | Mean | SD | N | Min | Max | Mean | SD |
|
| |||||||||||||||
| Patient age | 131 | 41 | 92 | 67.82 | 11.27 | 90 | 42 | 92 | 67.06 | 10.96 | 41 | 41 | 89 | 69.88 | 11.88 |
| Caregiver age | 131 | 39 | 89 | 65.30 | 10.74 | 90 | 45 | 88 | 64.43 | 10.14 | 41 | 39 | 89 | 67.20 | 11.87 |
| Relationship length | 121 | 1 | 70 | 35.90 | 17.76 | 82 | 1 | 70 | 35.56 | 16.97 | 39 | 2 | 68 | 36.62 | 19.52 |
| Importance of relationship | 131 | 4 | 6 | 5.84 | 0.43 | 90 | 4 | 6 | 5.78 | 0.49 | 41 | 5 | 6 | 5.98 | 0.16 |
| Positivity | 131 | 2 | 6 | 5.28 | 0.99 | 90 | 2 | 6 | 5.02 | 1.07 | 41 | 5 | 6 | 5.85 | 0.36 |
| Negativity | 131 | 1 | 6 | 2.44 | 1.47 | 90 | 2 | 6 | 3.10 | 1.32 | 41 | 1 | 1 | 1.00 | 0.00 |
| Anxiety | 131 | 5 | 16 | 9.89 | 2.41 | 90 | 6 | 16 | 10.19 | 2.23 | 41 | 5 | 16 | 9.22 | 2.68 |
| Depression | 131 | 1 | 14 | 5.49 | 2.55 | 90 | 1 | 14 | 5.81 | 2.63 | 41 | 2 | 11 | 4.78 | 2.23 |
| Burden:esteem | 131 | 2.71 | 4.86 | 4.18 | 0.41 | 90 | 2.86 | 4.86 | 4.13 | 0.42 | 41 | 2.71 | 4.86 | 4.29 | 0.37 |
| Burden:family support | 131 | 1 | 4 | 1.80 | 0.70 | 90 | 1 | 4 | 1.89 | 0.71 | 41 | 1 | 3.8 | 1.60 | 0.64 |
| Burden:finances | 131 | 1 | 5 | 2.46 | 0.97 | 90 | 1 | 5 | 2.50 | 0.91 | 41 | 1 | 5 | 2.37 | 1.09 |
| Burden:scheduling | 131 | 1 | 5 | 3.44 | 0.75 | 90 | 1 | 5 | 3.56 | 0.74 | 41 | 1.8 | 4.4 | 3.18 | 0.71 |
| Burden:health | 131 | 1.5 | 3.75 | 2.75 | 0.54 | 90 | 1.75 | 3.75 | 2.85 | 0.49 | 41 | 1.5 | 3.5 | 2.53 | 0.59 |
Forty-one caregivers saw their partner as supportive (31%), and 90 saw their partner as ambivalent (69%). Both groups on average rated their relationship with their spouse as highly important (of 6 possible; supportive M = 5.97, SD = 0.16; ambivalent M = 5.78, SD = 0.49) and highly positive (of 6 possible; supportive M = 5.85, SD = 0.36; ambivalent M = 5.02, SD = 1.07). The mean negativity rating in the ambivalent group was 3.10 (SD = 1.32; by definition, the mean supportive group negativity is 1.00, SD = 0). Chi-square and t-test analyses comparing groups showed no significant differences in education, income, patient and caregiver age, or length of relationship between supportive and ambivalent groups (p > .05).
Factor structure of caregiver reaction assessment
A latent variable for burden was created using the CRA subscale scores: family support, self-esteem, financial, scheduling, and health. We tested this factor structure using confirmatory factor analysis in MPlus software. Based on the published work on the scale (B. Given & Given, 1992; B. Given et al., 2004; C. Given et al., 1992; Nijboer et al., 2000; Stommel et al., 1992), a one-factor solution was proposed using a marker variable strategy (family support was fixed to 1) with uncorrelated errors. Analyses found the model fit was poor (χ2 = 20.734, degree of freedom (df) = 5, p < .01; root mean square error of approximation (RMSEA) = 0.152; standardized root mean square residual (SRMR) = 0.060). Although the fit is not within the acceptable range, these findings are consistent with previous research that found better solutions than the accepted five-factor model (Grov, Fossa, Tonnessen, & Dahl, 2006). Additionally, there is some evidence that fit indices do not perform well in models with a small df (Kenny, Kaniskan, & McCoach, in press). Given the factor model is well established, we used this factor structure in the overall structural model.
Overall model estimation
Maximum likelihood estimation was employed to estimate the overall structural model fit. Based on data from 131 individuals (41 supportive and 90 ambivalent), model fit was acceptable (χ2 = 48.059, df = 25, p = .0037; RMSEA = 0.084; SRMR = 0.056). The final model results with estimated betas and standard errors are presented in Figure 3 (circles represent latent variables and rectangles represent measured variables). The absence of a line connecting the variables implies no hypothesized direct effect. Using caregiver family support as a marker variable, burden subscales significantly mapped onto the latent variable of caregiver burden (p < .01). As expected, all loadings were positive, with the exception of caregiver self-esteem, which has an inverse relationship to the other subscales.
Figure 3.
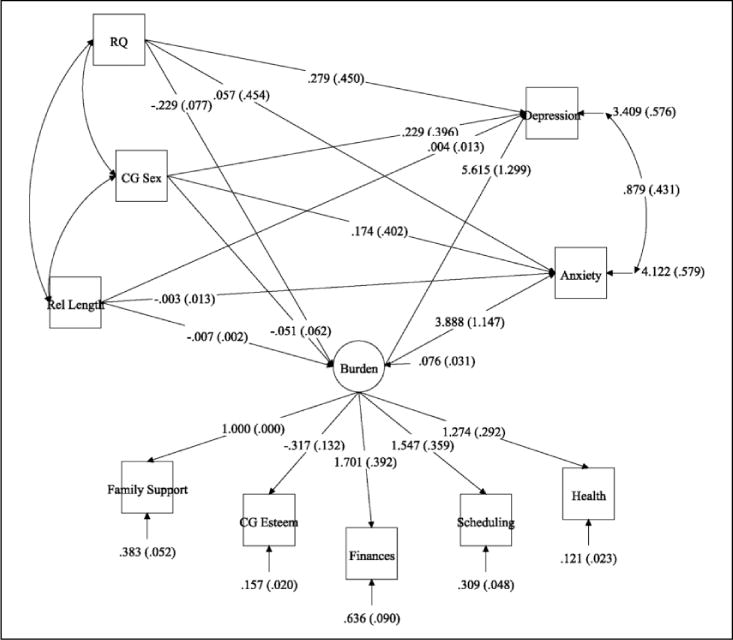
Final model with estimated betas and standard errors.
Controlling for caregiver sex and relationship length, relationship quality significantly predicted burden (B = −0.229, SE = 0.077, p < .01) but not anxiety (p = .899) or depression (p = .536). Although there was no significant difference between those with supportive and ambivalent relationships in financial burden (p > .05), caregivers with supportive spousal relationships had significantly higher caregiver self-esteem (t = −2.096, df = 129, p < .05), significantly lower burden from scheduling (t = 2.750, df = 129, p < .01), health (t = 2.980, df = 66.40, p < .01), and burden from family support (t = 2.294, df = 129, p < .05). Means are displayed in Table 1.
Burden significantly predicted anxiety (B = 3.888, SE = 1.147, p < .01) and depression (B = 5.615, SE = 1.299, p < .01) in that those who had greater burden were also more anxious and depressed. An advantage of structural equation modeling is that mediation can be tested within the main model. Tests of indirect paths between relationship quality and anxiety and depression through burden were conducted. Although neither direct pathway was significant between relationship quality and anxiety or depression, the specific indirect relationships between relationship quality and anxiety (B = −1.286, SE = 0.408, p < .01) and relationship quality and depression (B = −0.891, SE = 0.315, p < .01) showed that burden was a significant mediator of both variables, such that caregivers with supportive relationships had less anxiety and depression by way of decreased burden. Finally, we found a significant positive relationship between anxiety and depression (B = 0.879, SE = 0.431, p = .041).
Discussion
This study’s objectives were first to assess the existence of ambivalent and supportive caregiver relationships at entry to cancer home hospice as defined using a multidimensional operationalization of relationship quality and second to assess how caregiver relationship quality affects caregiver burden, anxiety, and depression. This is the first study to our knowledge that has used the SRI to assess relationship quality at end of life to parse out supportive versus ambivalent relationships. In our sample, we found that 31% of caregivers saw their spouse as supportive and 69% saw their partner as ambivalent. These percentages are similar to previous research assessing relationship quality with the SRI in older adults (Uchino et al., 2013) and confirm that ambivalence is prevalent in close relationships at end of life. We also found evidence to conclude that caregivers with supportive relationships reported significantly lower burden in comparison to caregivers with ambivalent relationships. Although relationship quality did not significantly predict anxiety and depression in a direct pathway, we found a significant, indirect relationship in that burden completely mediated the relationship between relationship quality and these distress measures.
Describing relationship quality at end of life
Our findings taken in combination with other works assessing relationship quality throughout the adult life span (Campo et al., 2009; Reblin, Uchino, & Smith, 2010; Uchino et al., 2013) now suggest that both ambivalent and supportive relationships exist throughout the trajectory of a close relationship. Although other research suggests that couples increasingly emphasize the positive aspects of relationships over time (Carstensen, Graff, Levenson, & Gottman, 1995), this does not preclude the coexistence of negativity. Previous research suggests that relationship quality within a particular relationship is relatively stable over time (Campo et al., 2009; Vaughn & Reblin, 2010); however, most longitudinal research in this area is limited by a short time lapse of only a few days or months. Future research following couples longitudinally over more extensive periods of time is needed to determine how individual couples’ relationship quality develops. In particular, it will be important to capture how perceived relationship quality may change through life challenges and impact roles, interaction patterns, and perceptions relevant to a close relationship. While some research has found caregivers view their relationships as deepening during this time (Walker et al., 1990), others find relationships weakening (Lawrence et al., 1998). Understanding potential change over the developmental trajectory into end of life and even bereavement has implications for relationship research as well as better understanding of the association between relationships and health.
The role of relationship quality in caregiver burden and distress
This study found that caregivers who had greater burden were also more anxious and depressed and that those caregivers who were more anxious were also more depressed. This relationship between burden and anxiety and depression in caregivers is supported widely throughout the literature (Burton et al., 2012; Cooper, Katona, Orrell, & Livingston, 2008; Grov, 2005; Price et al., 2010). In other research in palliative care populations, burden was found to be the most important predictor of anxiety and depression (Grunfeld et al., 2004).
While there was no direct relationship between relationship quality and anxiety and depression, there was an indirect relationship completely mediated by caregiver burden. In comparison to caregivers with ambivalent relationships, caregivers with supportive relationships reported higher caregiver self-esteem and less burden due to a disrupted schedule, health problems, and lack of family support, though there was no difference in financial burden. Those caregivers with lower burden were more likely to have lower levels of anxiety and depression.
The finding that relationship quality is related to caregiver burden is consistent with the idea that caregiver burden can be subjective and not necessarily tied to the difficulty of the task. Perhaps it is for this reason that the most objective type of burden—financial—was not found to differ between caregivers with supportive and ambivalent relationships. Although there is some research to support reports of burden being tied to objectively difficult caregiving situations (Pinquart & Sörensen, 2003), other research suggests caregiver burden accounts for factors over and above actual tasks (Braun, Mikulincer, Rydall, Walsh, & Rodin, 2007; Hughes, Giobbie-Hurder, Weaver, Kubal, & Henderson, 1999). Caregivers may become fatigued from the physical, emotional, psychosocial, and spiritual strain associated with cancer caregiving (Clark et al., 2014), which has a direct association with caregiver burden (Jensen & Given, 1993). It is also not surprising that caregivers who report greater burden are more likely to be anxious and depressed, as this has been well documented in the literature (e.g., Grov, Fosså, Sørebø, & Dahl, 2006; Grunfeld et al., 2004; Nijboer et al., 1998).
This study is in line with the previous qualitative research (Snyder, 2000) in which findings from caregiver interviews showed that despite the presence of objective burden, caregivers with high-quality relationships experienced less subjective burden. Others have also found conflict and discord within the relationship, which has been shown to contribute to reporting greater burden for those households with poorer relationship quality (Snyder, 2000; Wittenberg-Lyles et al., 2014). Quantitative work has also found similar results using different assessments of relationships (Spaid & Barusch, 1994; Steadman, Tremont, & Davis, 2007). However, given the cross-sectional nature of our study, we are unable to confirm the directionality of our results. Although the model tested in this study, based on the conceptual stress process model (Pearlin, Mullan, Semple, & Skaff, 1990), proposed that existing relationship quality impacts caregiver burden, which then predicts anxiety and depression levels, it is also possible that individuals who find caregiving more burdensome also increase their negative feelings about their partner, changing their view of the relationship to ambivalent, and have increased distress. However, previous research makes this alternative scenario unlikely. Our research has shown the stability of relationship quality (Campo et al., 2009; Vaughn & Reblin, 2010). Clyburn, Stones, Hadjistavropoulos, and Tuokko (2000) tested competing models of the relationships among caregiving stressors, burden, and depression in a large sample of caregivers of Alzheimer’s patients and found the best fit for the model in which burden mediated depression.
Limitation of a single time point
We speculated that there were several reasons why no direct relationship was found between relationship quality and distress. The first is that this study focused on a single time point of extreme adjustment distress. Entry into home hospice represented a time of transition. The caregiver is often just coming to terms with the death of the patient, navigating both family and health-care systems to set up home-based care (Schulman-Green et al., 2004; Waldrop, Kramer, Skretny, Milch, & Finn, 2005). Enrollment into hospice comes on top of the prior stress of caregiving through active treatment, which often wears down support resources (Bevans & Sternberg, 2012; Tilden & Weinert, 1987), and before the added support and involvement of the hospice team. Because our measures captured relationship, distress, and burden variables only at a single moment in time—entry to home hospice—it is possible that the acute stress and burden of this transition overshadowed any unique variance from relationship quality, which may later differentiate over the course of the chronic stress of continued caregiving. It might also be possible that the anticipated loss of the relationship makes its quality less important. Future longitudinal research is needed to determine how relationship quality impacts burden, anxiety, and depression over the course of the cancer caregiving trajectory—through both the chronic and acute stressors.
The importance of the broader social context
The caregivers’ broader social context is a second factor that could potentially impact caregiver burden (Harrison & Cole, 1991; Lai & Thomson, 2011; Sherman, Webster, & Antonucci, 2013) and thus the findings of this article. Although the spouse is often the most important member of one’s social network, friendships and other family relationships are also important predictors of well-being (Antonucci, Lansford, & Akiyama, 2001; Cable, Bartley, Chandola, & Sacker, 2013; de Vries, Utz, Caserta, & Lund, 2014). Support from the larger social network of friends and family can be particularly important when the spouse is dying and may serve as a protective buffer in more contentious relationships. Contributions from family and health-care providers cannot be ignored as most end-of-life decisions and care occur within this context (Haley et al., 2002; Williams et al., 2008).
Unfortunately, many forms of helpful support often drop-off after an initial influx in response to an acute stressor (Arora, Finney Rutten, Gustafson, Moser, & Hawkins, 2007), like cancer diagnosis. Further, caregivers may withdraw from their social networks as they become overwhelmed by their new tasks (Carr, House, Wortman, Nesse, & Kessler, 2001). Research has shown that a lack of support and resources from a broader network, including providers, can lead to even greater caregiver burden (Burton et al., 2012; Francis et al., 2010; Goldstein et al., 2004; Wittenberg-Lyles et al., 2014). Relationship quality likely plays a role in this context as well. For instance, recent findings suggest that caregiving in pairs—such as two siblings caring for a parent, which should reduce caregiver burden—may place individuals at a greater risk for anxiety and depression (Wittenberg-Lyles, Kruse, Oliver, Demiris, & Petroski, 2014). This study did not account for relationship quality or existing conflict, which may explain the counterintuitive results. More research is needed to investigate advanced cancer caregivers’ wider social networks.
Limitations
This study represents a snapshot of the caregiver experience at hospice enrollment. Future longitudinal research should investigate the end-of-life experience to determine how relationship quality and psychological distress change over time, including into bereavement (Grbich, Parker, & Maddocks, 2001). This research would also inform the literature about the mechanisms and processes involved. Additionally, there are a multitude of factors that we were unable to capture, which may also play a role in the relationships explored in this article, including the patient experience and the broader social context. The reader should also take into consideration that these caregiver participants have chosen to participate in research at end of life and therefore some selection bias may be at play. Finally, although hospice is predominantly used by non-Hispanic Caucasians (National Hospice and Palliative Care Organization, 2014), future research should seek to include a more racial and ethnically diverse sample to determine how best to serve a broader population.
Conclusion
This study represents a first look at relationship quality measured using multiple dimensions in spouse caregivers at entry to home hospice. We extended the relationship literature and established the existence of both supportive and ambivalent types of relationships in spouse caregivers of home hospice patients. We also assessed the interplay of relationship quality with caregiver burden, anxiety, and depression. Caregiver–spouse relationship quality significantly predicted caregiver burden, which mediated the association between relationship quality and anxiety and depression. This may be a function of the overwhelming impact of burden on these variables in a situation where often informal support resources have waned and formal hospice resources have yet to be available. Future research should further investigate supportive and ambivalent relationships as an important factor for caregiving across the cancer trajectory to end of life. Caregivers whose social contexts place them at risk for higher levels of distress may benefit from increased clinical attention or intervention.
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the American Cancer Society or the National Institutes of Health. The authors would like to thank the participants who make this research possible.
Funding: Research reported in this publication was supported by the American Cancer Society under award number ACS MRSG 13-234-01-PCSM and the National Cancer Institute of the National Institutes of Health under award number P01CA138317.
References
- American Cancer Society. Cancer facts & figures, 2014. Atlanta, GA: American Cancer Society; 2014. [Google Scholar]
- Antonucci TC, Lansford JE, Akiyama H. Impact of positive and negative aspects of marital relationships and friendships on well-being of older adults. Applied Developmental Science. 2001;5:68–75. [Google Scholar]
- Arora NK, Finney Rutten LJ, Gustafson DH, Moser R, Hawkins RP. Perceived helpfulness and impact of social support provided by family, friends, and health care providers to women newly diagnosed with breast cancer. Psychooncology. 2007;16:474–486. doi: 10.1002/pon.1084. [DOI] [PubMed] [Google Scholar]
- Ballantyne PJ. Social context and outcomes for the ageing breast cancer patient: Considerations for clinical practitioners. Journal of Clinical Nursing. 2004;13:11–21. doi: 10.1111/j.1365-2702.2004.00921.x. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. S0277953600000654. [DOI] [PubMed] [Google Scholar]
- Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. Journal of American Medical Association. 2012;307:398–403. doi: 10.1001/jama.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of Psychosomatic Research. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. S0022399901002963. [DOI] [PubMed] [Google Scholar]
- Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: Spouse caregivers. Journal of Clinical Oncology. 2007;25:4829–4834. doi: 10.1200/jco.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- Burton AM, Sautter JM, Tulsky JA, Lindquist JH, Hays JC, Olsen MK, Steinhauser KE. Burden and well-being among a diverse sample of cancer, congestive heart failure, and chronic obstructive pulmonary disease caregivers. Journal of Pain and Symptom Management. 2012;44:410–420. doi: 10.1016/j.jpainsymman.2011.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cable N, Bartley M, Chandola T, Sacker A. Friends are equally important to men and women, but family matters more for men’s well-being. Journal of Epidemiology and Community Health. 2013;67:166–171. doi: 10.1136/jech-2012-201113. [DOI] [PubMed] [Google Scholar]
- Campo RA, Uchino BN, Vaughn AA, Reblin M, Smith TW, Holt-Lunstad J. The assessment of positivity and negativity in social networks: The reliability and validity of the Social Relationships Index. Journal of Community Psychology. 2009;37:471–486. doi: 10.1002/jcop.20308. [DOI] [Google Scholar]
- Carr D, House JS, Wortman CB, Nesse R, Kessler RC. Psychological adjustment to sudden and anticipated spousal death among the older widowed. Journal of Gerontology: Social Sciences. 2001;56B:237–248. doi: 10.1093/geronb/56.4.s237. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Graff JC, Levenson RW, Gottman JM. Affect in intimate relationships: The developmental course of marriage. In: Magai C, McFadden SH, editors. Handbook of emotion, adult development, and aging. San Diego, CA: Academic Press; 1995. pp. 227–247. [Google Scholar]
- Chentsova-Dutton Y, Shuchter S, Hutchin S, Strause L, Burns K, Zisook S. The psychological and physical health of hospice caregivers. Annals of Clinical Psychiatry. 2000;12:19–27. doi: 10.1023/a:1009070826012. [DOI] [PubMed] [Google Scholar]
- Clark MM, Atherton PJ, Lapid MI, Rausch SM, Frost MH, Cheville AL, … Rummans TA. Caregivers of patients with cancer fatigue: A high level of symptom burden. American Journal of Hospice and Palliative Medicine. 2014;31:121–125. doi: 10.1177/1049909113479153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clyburn LD, Stones MJ, Hadjistavropoulos T, Tuokko H. Predicting caregiver burden and depression in Alzheimer’s disease. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2000;55:2–13. doi: 10.1093/geronb/55.1.s2. [DOI] [PubMed] [Google Scholar]
- Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Cooper C, Katona C, Orrell M, Livingston G. Coping strategies, anxiety and depression in caregivers of people with Alzheimer’s disease. International Journal of Geriatric Psychiatry. 2008;23:929–936. doi: 10.1002/gps.2007. [DOI] [PubMed] [Google Scholar]
- de Vries B, Utz R, Caserta M, Lund D. Friend and family contact and support in early widowhood. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;69:75–84. doi: 10.1093/geronb/gbt078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker SD, Young E. Self-perceived needs of primary caregivers of home-hospice clients. Journal of Community Health Nursing. 1991;8:147–154. doi: 10.1207/s15327655jchn0803_4. [DOI] [PubMed] [Google Scholar]
- Family Caregiver Alliance. Fact sheet: Selected caregiver statistics. 2012 Retrieved from http://www.caregiver.org/caregiver/jsp/home.jsp.
- Feinberg LF, Wolkwitz K, Goldstein C. Ahead of the curve: Emerging trends and practices in family caregiver support. Washington, DC: AARP Public Policy Institute; 2006. [Google Scholar]
- Finch JF, Okun MA, Barrera M, Jr, Zautra AJ, Reich JW. Positive and negative social ties among older adults: Measurement models and the prediction of psychological distress and well-being. American Journal of Community Psychology. 1989;17:585–605. doi: 10.1007/BF00922637. [DOI] [PubMed] [Google Scholar]
- Fiore J, Becker J, Coppel DB. Social network interactions: A buffer or a stress. American Journal of Community Psychology. 1983;11:423–439. doi: 10.1007/BF00894057. [DOI] [PubMed] [Google Scholar]
- Francis LE, Worthington J, Kypriotakis G, Rose JH. Relationship quality and burden among caregivers for late-stage cancer patients. Support Care Cancer. 2010;18:1429–1436. doi: 10.1007/s00520-009-0765-5. [DOI] [PubMed] [Google Scholar]
- Fromme EK, Drach LL, Tolle SW, Ebert P, Miller P, Perrin N, Tilden VP. Men as caregivers at the end of life. Journal of Palliative Medicine. 2005;8:1167–1175. doi: 10.1089/jpm.2005.8.1167. [DOI] [PubMed] [Google Scholar]
- Girgis A, Lambert S, Johnson C, Waller A, Currow D. Physical, psychosocial, relationship, and economic burden of caring for people with cancer: A review. Journal of Oncology Practice. 2013;9:197–202. doi: 10.1200/JOP.2012.000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given B, Given CW. Patient and family caregiver reaction to new and recurrent breast cancer. Journal of the American Medical Women’s Association. 1992;47:201. [PubMed] [Google Scholar]
- Given B, Wyatt G, Given C, Sherwood P, Gift A, DeVoss D, Rahbar M. Burden and depression among caregivers of patients with cancer at the end of life. Oncology Nursing Forum. 2004;31:1105–1117. doi: 10.1188/04.ONF.1105-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Research in Nursing & Health. 1992;15:271–283. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- Goldstein NE, Concato J, Fried TR, Kasl SV, Johnson-Hurzeler R, Bradley EH. Factors associated with caregiver burden among caregivers of terminally ill patients with cancer. Journal of Palliative Care. 2004;20:38–43. [PubMed] [Google Scholar]
- Gough K, Hudson P. Psychometric properties of the Hospital Anxiety and Depression Scale in family caregivers of palliative care patients. Journal of Pain and Symptom Management. 2009;37:797–806. doi: 10.1016/j.jpainsymman.2008.04.012. [DOI] [PubMed] [Google Scholar]
- Grbich C, Parker D, Maddocks I. The emotions and coping strategies of caregivers of family members with a terminal cancer. Journal of Palliative Care. 2001;17:30–36. [PubMed] [Google Scholar]
- Grov EK. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Annals of Oncology. 2005;16:1185–1191. doi: 10.1093/annonc/mdi210. [DOI] [PubMed] [Google Scholar]
- Grov EK, Fosså SD, Sørebø O, Dahl AA. Primary caregivers of cancer patients in the palliative phase: A path analysis of variables influencing their burden. Social Science & Medicine. 2006;63:2429–2439. doi: 10.1016/j.socscimed.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Grov EK, Fosså SD, Tonnessen A, Dahl AA. The caregiver reaction assessment: Psychometrics, and temporal stability in primary caregivers of Norwegian cancer patients in late palliative phase. Psychooncology. 2006;15:517–527. doi: 10.1002/pon.987. [DOI] [PubMed] [Google Scholar]
- Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, … Glossop R. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Canadian Medical Association Journal. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Haley WE, Allen RS, Reynolds S, Chen H, Burton A, Gallagher-Thompson D. Family issues in end-of-life decision making and end-of-life care. American Behavioral Scientist. 2002;46:284–298. doi: 10.1177/000276402236680. [DOI] [Google Scholar]
- Haley WE, LaMonde LA, Han B, Narramore S, Schonwetter R. Family caregiving in hospice: Effects on psychological and health functioning among spousal caregivers of hospice patients with lung cancer or dementia. The Hospice Journal. 2001;15:1–18. doi: 10.1080/0742-969x.2000.11882959. [DOI] [PubMed] [Google Scholar]
- Harrison DS, Cole KD. Family dynamics and caregiver burden in home health care. Clinics in Geriatric Medicine. 1991;7:817–829. [PubMed] [Google Scholar]
- Hasson-Ohayon I, Goldzweig G, Sela-Oren T, Pizem N, Bar-Sela G, Wolf I. Attachment style, social support and finding meaning among spouses of colorectal cancer patients: Gender differences. Palliative and Supportive Care. 2013;8:1–9. doi: 10.1017/s1478951513000242. [DOI] [PubMed] [Google Scholar]
- Hebert RS, Arnold RM, Schulz R. Improving well-being in caregivers of terminally ill patients: Making the case for patient suffering as a focus for intervention research. Journal of Pain & Symptom Management. 2007;34:539–546. doi: 10.1016/j.jpainsymman.2006.12.016. doi:S0885-3924(07)00350-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Uchino BN, Smith TW, Olsen-Cerny C, Nealey-Moore JB. Social relationships and ambulatory blood pressure: Structural and qualitative predictors of cardiovascular function during everyday social interactions. Health Psychology. 2003;22:388–397. doi: 10.1037/0278-6133.22.4.388. [DOI] [PubMed] [Google Scholar]
- Hughes SL, Giobbie-Hurder A, Weaver FM, Kubal JD, Henderson W. Relationship between caregiver burden and health-related quality of life. The Gerontologist. 1999;39:534–545. doi: 10.1093/geront/39.5.534. [DOI] [PubMed] [Google Scholar]
- Jensen S, Given B. Fatigue affecting family caregivers of cancer patients. Support Care Cancer. 1993;1:321–325. doi: 10.1007/BF00364970. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kaniskan B, McCoach DB. The performance of RMSEA in models with small degrees of freedom. Sociological Methods & Research. doi: 10.1177/0049124114543236. in press. [DOI] [Google Scholar]
- Kim Y, Carver CS, Deci EL, Kasser T. Adult attachment and psychological well-being in cancer caregivers: The mediational role of spouses’ motives for caregiving. Health Psychology. 2008;27:144–154. doi: 10.1037/0278-6133.27.2(Suppl.).S144. doi:2008-03488-007. [DOI] [PubMed] [Google Scholar]
- Kissane DW, Bloch S, Burns WI, McKenzie D, Posterino M. Psychological morbidity in the families of patients with cancer. Psycho-Oncology. 1994;3:47–56. doi: 10.1002/pon.2960030109. [DOI] [Google Scholar]
- Kramer BJ, Kavanaugh M, Trentham-Dietz A, Walsh M, Yonker JA. Predictors of family conflict at the end of life: The experience of spouses and adult children of persons with lung cancer. Gerontologist. 2010;50:215–225. doi: 10.1093/geront/gnp121. doi: gnp121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz ME, Given B, Kurtz JC, Given CW. The interaction of age, symptoms, and survival status on physical and mental health of patients with cancer and their families. Cancer. 1994;74:2071–2078. doi: 10.1002/1097-0142(19941001)74:7+<2071::aid-cncr2820741715>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Lai D, Thomson C. The impact of perceived adequacy of social support on caregiving burden of family caregivers. Families in Society: The Journal of Contemporary Social Services. 2011;92:99–106. doi: 10.1606/1044-3894.4063. [DOI] [Google Scholar]
- Lambert S, Pallant JF, Girgis A. Rasch analysis of the Hospital Anxiety and Depression Scale among caregivers of cancer survivors: Implications for its use in psycho-oncology. Psycho-Oncology. 2011;20:919–925. doi: 10.1002/pon.1803. [DOI] [PubMed] [Google Scholar]
- Lawrence RH, Tennstedt SL, Assmann SF. Quality of the caregiver–care recipient relationship: Does it offset negative consequences of caregiving for family caregivers? Psychology and Aging. 1998;13:150–158. doi: 10.1037/0882-7974.13.1.150. [DOI] [PubMed] [Google Scholar]
- Levenson RW, Carstensen LL, Gottman JM. Long-term marriage: Age, gender, and satisfaction. Psychology and Aging. 1993;8:301–313. doi: 10.1037//0882-7974.8.2.301. [DOI] [PubMed] [Google Scholar]
- Li Q, Loke AY. The positive aspects of caregiving for cancer patients: A critical review of the literature and directions for future research. Psycho-Oncology. 2013;22:2399–2407. doi: 10.1002/pon.3311. [DOI] [PubMed] [Google Scholar]
- Manne SL, Glassman M. Perceived control, coping efficacy, and avoidance coping as mediators between spouses’ unsupportive behaviors and cancer patients’ psychological distress. Health Psychology. 2000;19:155–164. doi: 10.1037//0278-6133.19.2.155. [DOI] [PubMed] [Google Scholar]
- Manne SL, Pape SJ, Taylor KL, Dougherty J. Spouse support, coping, and mood among individuals with cancer. Annals of Behavioral Medicine. 1999;21:111–121. doi: 10.1007/BF02908291. [DOI] [PubMed] [Google Scholar]
- McLean LM, Jones JM. A review of distress and its management in couples facing end-of-life cancer. Psycho-Oncology. 2007;16:603–616. doi: 10.1002/pon.1196. [DOI] [PubMed] [Google Scholar]
- Mitschke DB. Cancer in the family: Review of the psychosocial perspectives of patients and family members. Journal of Family Social Work. 2008;11:166–184. doi: 10.1080/10522150802175159. [DOI] [Google Scholar]
- Monin JK, Schulz R. Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging. 2009;24:681–695. doi: 10.1037/a0016355. doi:2009-13203-017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Hospice and Palliative Care Organization. NHPCO facts and figures: Hospice care in America. Alexandria, VA: National Hospice and Palliative Care Organization; 2014. [Google Scholar]
- Neufeld A, Harrison MJ. Men as caregivers: Reciprocal relationships or obligation? Journal of Advanced Nursing. 1998;28:959–968. doi: 10.1046/j.1365-2648.1998.00818.x. [DOI] [PubMed] [Google Scholar]
- Nijboer C, Tempelaar R, Sanderman R, Triemstra M, Spruijt RJ, Van Den Bos GAM. Cancer and caregiving: The impact on the caregiver’s health. Psycho-Oncology. 1998;7:3–13. doi: 10.1002/(SICI)1099-1611(199801/02)7:1<3::AID-PON320>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Nijboer C, Triemstra M, Tempelaar R, Mulder M, Sanderman R, van den Bos GA. Patterns of caregiver experiences among partners of cancer patients. Gerontologist. 2000;40:738–746. doi: 10.1093/geront/40.6.738. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Price MA, Butow PN, Costa DS, King MT, Aldridge LJ, Fardell JE, Webb PM, Australian Ovarian Cancer Study Group Quality of Life Study, Investigators Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. Medical Journal of Australia. 2010;193:S52–S57. doi: 10.5694/j.1326-5377.2010.tb03929.x. [DOI] [PubMed] [Google Scholar]
- Reblin M, Uchino BN, Smith TW. Provider and recipient factors that may moderate the effectiveness of received support: Examining the effects of relationship quality and expectations for support on behavioral and cardiovascular reactions. Journal of Behavioral Medicine. 2010;33:423–431. doi: 10.1007/s10865-010-9270-z. [DOI] [PubMed] [Google Scholar]
- Resendes LA, McCorkle R. Spousal responses to prostate cancer: An integrative review. Cancer Investigation. 2006;24:192–198. doi: 10.1080/07357900500524652. [DOI] [PubMed] [Google Scholar]
- Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal caregiving for cancer patients. Cancer. 2013;119:2160–2169. doi: 10.1002/cncr.28057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon JR, Deming AM, Kwak J, Acquiaviva KD, Brandt K, Egan K. Caregiving at life’s end: The national needs assessment and implications for hospice practice. Clearwater, FL: Hospice Institute of the Florida Suncoast; 2003. [Google Scholar]
- Schulman-Green D, McCorkle R, Curry L, Cherlin E, Johnson-Hurzeler R, Bradley E. At the crossroads: Making the transition to hospice. Palliative and Supportive Care. 2004;2:351–360. doi: 10.1017/s1478951504040477. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality: The caregiver health effects study. Journal of the American Medical Association. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. doi:joc91040. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health. 1986;5:165–173. doi: 10.1300/J018v05n01_09. [DOI] [Google Scholar]
- Sherman CW, Webster NJ, Antonucci TC. Dementia caregiving in the context of late-life remarriage: support networks, relationship quality, and well-being. Journal of Marriage and Family. 2013;75:1149–1163. doi: 10.1111/jomf.12059. [DOI] [Google Scholar]
- Snyder J. Impact of caregiver-receiver relationship quality on burden and satisfaction. Journal of Women & Aging. 2000;12:147–167. doi: 10.1300/J074v12n01_10. [DOI] [PubMed] [Google Scholar]
- Spaid WM, Barusch A. Emotional closeness and caregiver burden in the marital relationship. Journal of Gerontological Social Work. 1994;21:197–212. doi: 10.1300/J083V21N03_13. [DOI] [Google Scholar]
- Stajduhar KI, Funk L, Toye C, Grande GE, Aoun S, Todd CJ. Part 1: Home-based family caregiving at the end of life: A comprehensive review of published quantitative research (1998–2008) Palliative Medicine. 2010;24:573–593. doi: 10.1177/0269216310371412. [DOI] [PubMed] [Google Scholar]
- Steadman PL, Tremont G, Davis JD. Premorbid relationship satisfaction and caregiver burden in dementia caregivers. Journal of Geriatric Psychiatry and Neurology. 2007;20:115–119. doi: 10.1177/0891988706298624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stommel M, Wang S, Given CW, Given B. Focus on psychometrics: Confirmatory factor analysis (CFA) as a method to assess measurement equivalence. Research in Nursing & Health. 1992;15:399–405. doi: 10.1002/nur.4770150508. [DOI] [PubMed] [Google Scholar]
- Tilden VP, Weinert C. Social support and the chronically ill individual. The Nursing Clinics of North America. 1987;22:613–620. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services Office on Women’s Health. Caregiver stress. 2011 Retrieved from www.womenshealth.gov.
- Uchino BN. Social support and physical health: Understanding the health consequences of our relationships. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- Uchino BN, Bosch JA, Smith TW, Carlisle M, Birmingham W, Bowen KS, O’Hartaigh B. Relationships and cardiovascular risk: Perceived spousal ambivalence in specific relationship contexts and its links to inflammation. Health Psychology. 2013;32:1067–1075. doi: 10.1037/a0033515. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Holt-Lunstad J, Uno D, Flinders JB. Heterogeneity in the social networks of young and older adults: Prediction of mental health and cardiovascular reactivity during acute stress. Journal of Behavioral Medicine. 2001;24:361–382. doi: 10.1023/a:1010634902498. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Holt-Lunstad J, Uno D, Campo R, Reblin M. The social neuroscience of relationships: An examination of health-relevant pathways. In: Harmon-Jones E, Winkielman P, editors. Social neuroscience: Integrating biological and psychological explanations of social behavior. New York, NY: Guilford Press; 2007. pp. 474–492. [Google Scholar]
- Uchino BN, Kiecolt-Glaser JK, Cacioppo JT. Construals of preillness relationship quality predict cardiovascular response in family caregivers of Alzheimer’s disease victims. Psychology and Aging. 1994;9:113–120. doi: 10.1037//0882-7974.9.1.113. [DOI] [PubMed] [Google Scholar]
- Vaughn A, Reblin M. Engaged couples’ transition into marriage: Relationship quality and dyadic adjustment; Paper presented at the Western Psychological Association; Cancun, Mexico. 2010. [Google Scholar]
- Waldrop DP, Kramer BJ, Skretny JA, Milch RA, Finn W. Final transitions: Family caregiving at the end of life. Journal of Palliative Medicine. 2005;8:623–638. doi: 10.1089/jpm.2005.8.623. [DOI] [PubMed] [Google Scholar]
- Walker AJ, Shin H, Bird DN. Perceptions of relationship change and caregiver satisfaction. Family Relations. 1990;39:147–152. doi: 10.2307/585716. [DOI] [Google Scholar]
- Williams SW, Williams CS, Zimmerman S, Munn J, Dobbs D, Sloane PD. Emotional and physical health of informal caregivers of residents at the end of life: The role of social support. Journal of Gerontology: Part B Psychological Science and Social Science. 2008;63:171–183. doi: 10.1093/geronb/63.3.s171. doi:63/3/S171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson GM, Shaffer DR. Caregiver loss and quality of care provided: Preillness relationship makes a difference. In: Harvey JH, Miller ED, editors. Loss and trauma: General and close relationship perspectives. New York, NY: Brunner-Routledge; 2000. pp. 307–330. [Google Scholar]
- Wittenberg-Lyles E, Kruse RL, Oliver DP, Demiris G, Petroski G. Exploring the collective hospice caregiving experience. Journal of Palliative Medicine. 2014;17:50–55. doi: 10.1089/jpm.2013.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittenberg-Lyles E, Washington K, Demiris G, Oliver DP, Shaunfield S. Understanding social support burden among family caregivers. Health Communication. 2014;29:901–910. doi: 10.1080/10410236.2013.815111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]


