Abstract
AIM: To compare the postoperative mechanical alignment achieved after total knee arthroplasty (TKA) using computer tomography (CT) based patient specific blocks (PSB) to conventional instruments (CI).
METHODS: Total 80 knees were included in the study, with 40 knees in both the groups operated using PSB and CI. All the knees were performed by a single surgeon using the same cruciate sacrificing implants. In our study we used CT based PSB to compare with CI. Postoperative mechanical femoro-tibial angle (MFT angle) was measured on long leg x-rays using picture archiving and communication system (PACS). We compared mechanical alignment achieved using PSB and CI in TKA using statistical analysis.
RESULTS: The PSB group (group 1) included 17 females and seven males while in CI group (group 2) there were 15 females and eight males. The mean age of patients in group 1 was 60.5 years and in group 2 it was 60.2 years. The mean postoperative MFT angle measured on long-leg radiographs in group 1 was 178.23° (SD = 2.67°, range: 171.9° to 182.5°) while in group 2, the mean MFT angle was 175.73° (SD = 3.62°, range: 166.0° to 179.8°). There was significant improvement in postoperative mechanical alignment (P value = 0.001), in PSB group compared to CI. Number of outliers were also found to be less in group operated with PSB (7 Knee) compared to those operated with CI (17 Knee).
CONCLUSION: PSB improve mechanical alignment after total knee arthroplasty, compared to CI. This may lead to lower rates of revision in the PSB based TKA as compared to the conventional instrumentation.
Keywords: Knee, Replacement, Arthroplasty, Patient specific jigs, Conventional jigs
Core tip: Computer tomography (CT) based patient specific blocks (PSB) can help restore the mechanical axis of the patients undergoing primary total knee replacement. In the present study, the PSB group had significantly better post-operative mechanical axis as compared to the conventional instrumentation group. CT based PSB holds promise to help in accurate restoration of the mechanical axis and might decrease the rates of revision after total knee arthroplasty.
INTRODUCTION
Total knee arthroplasty (TKA) has been a successful surgery providing excellent functional results in a patient with an advanced degenerative joint disease of the knee. It has been accepted that postoperative lower limb alignment is an important parameter for favorable functional outcomes in TKA[1]. Arthroplasty surgeons aim to achieve an average mechanical angle (i.e., 180°) and any variation more than 3° may lead to poor functional results and early implant failure[2,3]. Therefore, postoperative mechanical alignment has been considered an important index for a successful surgery amongst arthroplasty surgeons.
The commonly used conventional instruments (CI) in TKA consist of intramedullary (I/M) femoral alignment guide and extramedullary (E/M) tibial alignment guide. Although these instruments are familiar to most surgeons and easy to use, they have demonstrated a limited degree of accuracy[4]. The CI used as I/M femoral guide is aligned on the basis of anatomical axis of the femur. However, the surgeon intends to have distal femur bone cut perpendicular to the mechanical axis (MA) of the femur. In this technique, the surgeon has to make an assumption about the femoral valgus angle which may lead to error in bone cuts, due to the discrepancy in the assumed and the real femoral valgus angle. Also, there could be errors in rotational alignment that is estimated using the epicondylar axis or the anteroposterior axis as popularized by Whiteside et al[5]. The epicondylar axis is hard to determine and can lead to significant inter as well as intra-observer variability[6-8]. The I/M guide is dependent on an exact fit of the rod in the femoral canal, which is not always obtained and on the position of the entrance hole in the femur, which is user dependent and may significantly alter the distal femoral mechanical angle[9-12]. Due to several inherent limitations of CI, there was a need for improvement, and this has prompted efforts to develop a more precise surgical technology for restoring an accurate mechanical axis after TKA.
This initiative led the development of computer-assisted surgery (CAS) techniques. Although, CAS has been shown to improve MA over CI, it is also associated with disadvantages like increased surgical time, expensive instrumentation, steep learning curve, higher number of personnel required and higher infection rates[13,14].
Patient specific blocks (PSB) were introduced as an alternative to CAS and CI, with the goal of improving postoperative alignment, implant positioning and overcoming the shortcomings associated with the CAS and CI. These blocks were manufactured before the surgery after a computerized tomography (CT) analysis (Figure 1). The primary aim of these blocks is to optimize the bone cuts so as to achieve accurate MA of the lower limb. There has been recent interest seen in the literature regarding the use and efficacy of patient specific instruments (PSI) in achieving the optimal MA after TKA. But, until now the published reports comparing PSI and CI in primary TKA vary regarding the actual advantages of PSB[15-19].
Figure 1.
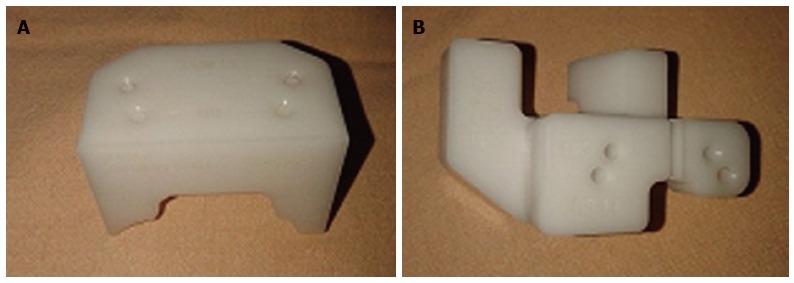
Patient specific blocks used in the present study (A: Femoral jig, B: Tibial jig).
We undertook this study with the aim to compare the postoperative mechanical alignment achieved using PSI and CI in TKA to assess the efficacy of CT-based PSB in the achievement of anatomical alignment after primary TKA.
MATERIALS AND METHODS
This study was a prospective, comparative single study conducted over a period of one year. All the patients who came with severe degenerative arthritis of knee (Ahlback’s grade 3 or 4) and planned for TKA during the period from November 2013 to October 2014 in one unit were included in this study. An approval from the institutional review board was taken. As the technique of PSB was still new and very few patients were aware of it, all the subjects were first explained and made familiar with the technique of PSB and its difference from CI for TKA. Patient were informed about the expected benefits and advantages of PSB, and also about the extra cost of 400$ per knee involved in using the PSB (cost of CT Scannogram and manufacturing of the blocks). Subjects who were ready to bear the extra cost, willing to undergo the CT scan, and gave consent were operated using PSB, and were named as group 1. Remaining subjects were conducted using CI and designated as group 2.
Each group included 40 knees. Most of the knees had varus deformity except six knees in each group having a valgus deformity. CT scan of group 1 subjects was done preoperatively in the same institute and data sent to PSB manufacturing unit. PSB manufactured from Stryker® was used for all subjects in group 1 (Figure 1). Stryker Scorpio™ posterior stabilized knee system was used in all the patients.
An anterior-posterior radiograph of the knee in standing and lateral positions was done preoperatively. Each of these patients was operated by the same surgeon (RV) in the same operating setup and using a similar protocol.
An anterior midline longitudinal incision with modified Insall’s approach[20] was used in all the TKA and the majority of operating steps were same in both the groups, except that the alignment guides (PSB) were used in group 1 (Figures 2 and 3). In group 2, E/M alignment guide for tibia and I/M alignment guide for femur were used. The tibial alignment guide was adjusted to achieve 0º varus/valgus cut with 5º posterior slope, whereas on the femoral side 50 valgus (which was reduced to 30 valgus for valgus knees) and 30 external rotation was kept in the alignment guide. The decision to change the femoral valgus angle in the valgus knees in the CI group was taken based on standard protocol and was not based on any pre-operative femoral valgus angle calculation.
Figure 2.
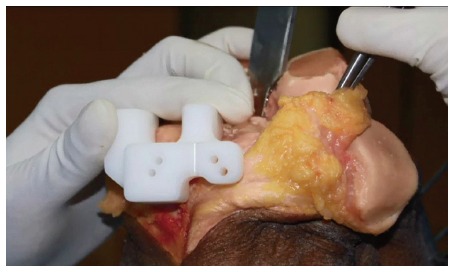
Tibial jig conforming to the proximal tibial anatomy and fiiting well to the bone. This jig is used for insertion of the proximal tibial pins followed by use of the conventional proximal tibial jig.
Figure 3.

Femoral jig matching the contour of the anterior femoral cortex.
We aimed to achieve a rectangular gap of 20 mm which was equally symmetrical in both flexion and extension. All the modifications required in operating steps for proper bone cuts to achieve accurate alignment were done intraoperatively in group 2 patients performed with CI. Whereas, in group 1 patients all the planning was done preoperatively, which started with preoperative CT scannogram followed by an assessment of bone cut on virtual bone models and finally fabrication of blocks after approval from the operating surgeon (Figure 1). These blocks were then used intraoperatively to decide the pin position over which a conventional cutting jig was placed for planned bone cuts.
The primary aim of this study was to compare the postoperative mechanical alignment achieved with using PSI and CI in TKA. The MA was assessed by measuring the Mechanical femoral-tibial angle (MFT angle) on a long-leg radiograph of lower limb done on second follow-up visits, planned after one month of surgery, as most of the patients were able to stand erect with full knee extension and without any support (Figure 4). All the MFT angles were measured by a single individual of the operating unit (VB) who first underwent adequate training in the measurement of the MFT angle on long leg standing radiographs. Outliers of the mechanical axis after total knee arthroplasty were defined as those patients who had values of mechanical axis ± 3 degrees from the neutral 180º. Thus, inter-observer and intra-observer variation were avoided. Data from both the groups was analyzed and compared using statistical analysis as mentioned below.
Figure 4.
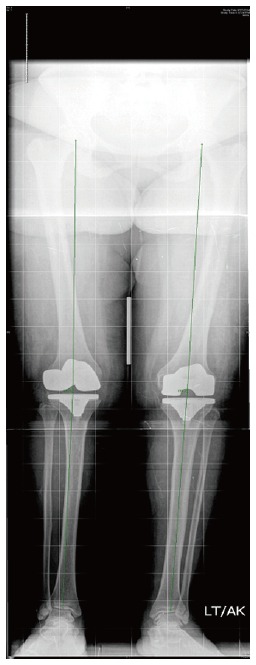
Postoperative weight bearing long leg radiograph measuring the hip-knee-ankle angle axis (mechanical axis).
Statistical analysis
Statistical analysis was performed by the SPSS program for Windows, version 17.0. Continuous variables were presented as mean ± SD or median and categorical variables were presented as absolute numbers and percentage. Data were checked for normality before statistical analysis. Normally distributed continuous variables were compared using the unpaired t test, whereas the Mann-Whitney U test was used for those variables that were not normally distributed. Categorical variables were analyzed using either the χ2 test or Fisher’s exact test. For all statistical tests, a P value less than 0.05 were taken to indicate a significant difference.
RESULTS
The study group 1 included 17 females and seven males while in group 2 there were 15 females and eight males. The mean age of patients in group 1 was 60.5 years and in group 2 it was 60.2 years. In group 1, 16 patients had bilateral, and 8 had unilateral TKA. In group 2, 17 patients had bilateral, and 6 had unilateral TKA. No significant difference was found between the two groups concerning age, sex, and sidewise distribution. The mean postoperative MFT angle measured on long-leg radiographs in group 1 was 178.23° (SD = 2.67°, range - 171.9° to 182.5°) while in group 2, the mean MFT angle was 175.73° (SD = 3.62°, range - 166.0° to 179.8°) (Table 1).There was a significant difference in postoperative MA achieved in PSI (group 1) compared to CI (group 2) with p-value = 0.001. In group 1 there were 7 outliers while in group 2, there were 17 outliers (Figures 5 and 6). Thus, there was also increase in outliers in group 2 compared to group 1. There was a significant difference in outliers achieved in PSI (group 1) compared to CI (group 2) with p-value = 0.0147 (Figures 5 and 6).
Table 1.
comparison of post-operative mechanical femoral tibial angle between the patient specific block group and the conventional group
| PSB group (n = 40) Mean ± SD | Conventional group (n = 40) Mean ± SD | Mean difference | P value | |
| Postop MFT angle | 178.23 ± 2.67 | 175.73 ± 3.62 | 2.497 | 0.001 |
Postop: Post operation; MFT: Mechanical femoro-tibial; PSB: Patient specific blocks.
Figure 5.
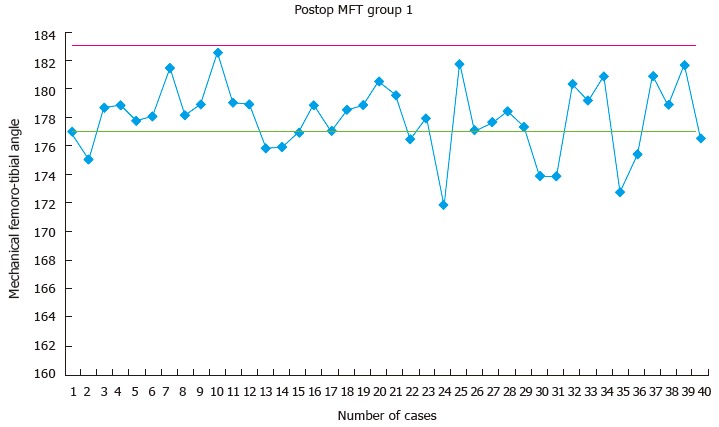
Scatter diagram depicting the distribution of the post-operative mechanical femoro-tibial angle (mechanical femoro-tibial angle) in the patient specific block group (group 1). MFT: Mechanical femoro-tibial angle.
Figure 6.
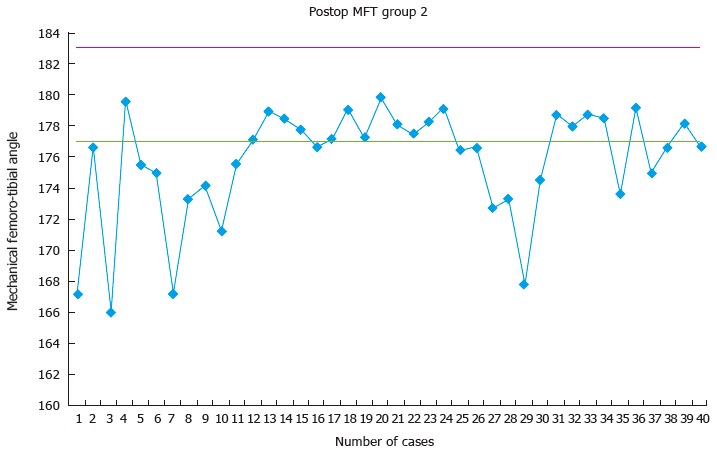
Scatter diagram depicting the distribution of the post-operative mechanical femoro-tibial angle (mechanical femoro-tibial angle) in the conventional instrument group (group 2). MFT: Mechanical femoro-tibial angle.
DISCUSSION
The number of TKA annually is increasing every year, but the main concern for a surgeon and patient undergoing primary TKA remains long-term survival of the implant. Also, the increased morbidity, healthcare cost and complications associated with revision surgery have further guided the arthroplasty surgeons to strive for longer implant survival. One of the most important factors contributing to implant survival is accurate mechanical alignment. Various techniques like computer navigation, PSI, etc., have been introduced to achieve precise mechanical alignment in TKA.
The importance of accurate postoperative mechanical alignment of lower limb for the successful outcome of TKA has been accepted widely and supported by several studies. As early as in 1977, Lotke et al[21] reported the importance of accurate implant positioning in the long term survival of knee implants. These findings were further corroborated by Ritter et al[2] who demonstrated an increased failure rate for knees in varus. Sharkey et al[3] concluded that most of the revisions which were performed within the first two years of primary surgery were due to errors in surgical technique. This background knowledge prompted the development and introduction of PSI with the aim of improving post-operative mechanical alignment while bypassing the drawbacks of CAS. Improvement in mechanical alignment with the use of PSI in TKA was first reported by Hafez et al[22] on cadaveric knees and plastic bones. Similar results were obtained from a study done by Ng et al[4] where they compared 569 TKA done with PSI to 155 TKA done with conventional instruments and found decreased a number of outliers with PSI. The numbers of outliers with any technique used in TKA remains an important observation and indicate the efficacy of that technique. We also found decreased outliers with the use of PSI, in our study. Heyse et al[23] and Renson et al[24] also noticed decreased the number of outliers with PSI (13%) compared to conventional jig (29%).
However, some authors found contradictory results in their studies. Abane et al[25] compared 70 TKA done with PSI to an equal number of TKA done with CI and could not find any significant improvement in the post operative MA with the use PSI over CI. Klatt et al[26] reported 4 patients operated with PSI showed malalignment in mechanical axis. From their small case series, they opined that this emerging technology ignores conventional principles of TKA and the software used unreliable at present. Chen et al[16] in their study of 60 patients found increased outliers with the use of PSI. Parratte et al[27] suggested that more refinement needed to be done in PSI to have better control of the tibial rotation. The inferior results in these studies could have been due to the evolving technology of PSI at the time of these studies, the associated learning curve and different designs of the cutting jig used in the studies[16,25,26].
The other point of discussion in the use of PSI is the radiological method used for pre-operative planning. This technology utilizes advanced imaging techniques like magnetic resonance imaging (MRI) and CT scan to reproduce a 3D model of the patient’s bone which is in turn used to create jigs which are used intra-operatively either to directly take bone cuts or to guide the insertion of pins. The debate regarding the best imaging modality is ongoing. In a systematic review of the use of CT vs MRI in PSI showed a decreased number of outliers in the CT group (12.5%) as compared to MRI (16.9%) group[28]. There are various advantages of the CT-based PSI over MRI-based (Table 2). The CT scan is associated with decreased cost and imaging times[28]. Moreover, it can be easily performed in patients with cardiac pacemakers and metallic implant in situ. The widespread availability of the CT scan in a developing country, also make it accessible to a larger profile of surgeons and patients. Even in high volume center, there is usually a single MRI machine which can further increase the waiting period of the patient. The accuracy of the CT-based PSI as compared to the MRI-based PSI have been found to be comparable[29,30]. The only disadvantage of the CT scan based PSI is the possibility of increased radiation exposure as compared to MRI. This has further been circumvented by the use of focused scans of the hip, knee and ankle, which further decreases the dosage of radiation to 5MSv, which is comparable to the background radiation or approximately 70 chest X-rays[31]. In the present study, CT-based PSI technique was used and found to provide a satisfactory outcome.
Table 2.
Comparison of computerized tomography based and magnetic resonance imaging based patient specific blocks
| Computerized tomography based blocks | Magnetic resonance imaging based blocks | |
| Time for study | Lesser (approximately 5 min) | Longer (approximately 45 min) |
| Cost | Economical | Costlier |
| Radiation exposure | Uses ionizing radiation. But focused hip-knee-ankle computerized tomography scanogram reduces exposure to 5 mSv (equal to yearly background exposure) | Does not use ionizing radiation |
| Availability | Easily available | Not available at all centers |
| Patient turn over | Useful for high patient turnover centers | Not suitable for high patient turnover center |
| Contraindication | Can be used in patient with any metal prosthesis in situ | Cannot be used in patient with metal prosthesis or cardiac pacemaker in situ |
| Based on | Bony landmarks | Cartilage |
| Accuracy | Comparable | Comparable |
| Initial infrastructure set up cost | Lower as compared to MRI | High, non affordable for low volume centres |
| Claustrophobia | No contraindication | Can not be performed in claustrophobic patients |
MRI: Magnetic resonance imaging.
In the present study, we found more accurate alignment in TKA done by PSI compared to CI, with a statistically significant improvement in MFT angle in PSI group (P = 0.001). The number of outliers was also decreased with the use of PSI. The mean MFT angle measured postoperatively in group 1 was 178.23° and in group 2 it was 175.73°. The preoperative planning done in PSI group was the main reason for achieving accurate MA postoperatively. The CT scannogram of lower limb done preoperatively gives thorough information of actual bony anatomy of knee and limb alignment. The patient specific blocks thus produced fit to patient’s bony anatomy accurately and thus lead to proper pin positioning and accurate bone cuts intraoperatively. Proper pin positioning, and accurate bone cuts can be attributed as the reasons for the improvement in mechanical alignment in TKA with PSI.
PSI avoids manual error involved in pin position with conventional instruments. The accuracy of the valgus cut angle depends on an accurate entry point and the snug fit of the intra-medullary alignment rod in the femoral canal. These two factors are circumvented by the use of PSI and hence may be responsible for better achievement of the distal femoral valgus angle. Moreover, the positioning of the extra-medullary alignment rod for the tibia depends on the surgeon’s perception of centralizing the rod at the center of the ankle. This is subject to error due to the surgeon (difference in perception of the alignment) and also due to patient factors like excessive fat and soft tissue around the ankle, etc. With the use of PSI, both these factors are decided pre-operatively during planning and hence the manual error is minimized.
There were certain shortcomings of the present study. The study was not a randomized controlled trial. Our sample size was also small, but it can be considered a representative study and further studies should be done to define the exact efficacy of PSI in improving the overall mechanical axis.
Considering the current trends of joint replacement and also due to a consistent increase in the life expectancy of the population, there is going to be an exponential growth in the number of total knee arthroplasty being done. The focus is shifting to increase the long-term survival of the artificial joints in a cost efficient manner, to decrease the financial and health burden of revision surgery. PSI technology is a step in this direction as it helps in improving the postoperative mechanical axis and also improve the operating room efficiency. This study defines that the PSI technology helps in significantly improving the postoperative mechanical alignment as compared to conventional technology and has future potential to provide long-term benefits to patients.
COMMENTS
Background
The zeal to achieve improved patient outcomes and longer implant survival has opened new avenues in the field of total knee arthroplasty. Patient specific jigs hold promise in achieving both these.
Research frontiers
Patient specific blocks have recently caught the attention of researchers with multiple studies showing good results. These blocks can be manufactured on the basis of the patient’s magnetic resonance imaging (MRI) and computer tomography (CT) scan. It is of interest to see whether CT based jigs can achieve good results in the post operative outcomes and alignment of patients undergoing total knee arthroplasty.
Innovations and breakthroughs
The authors confirm that CT based blocks can achieve accurate restoration of the post operative mechanical axis and good post operative pain relief and rehabilitation. The CT scan based blocks hold some inherent advantages over the MRI based jigs and these have also been discussed in the present study.
Applications
CT based patient specific blocks hold promise for the future in the quest to improve implant longevity in total knee arthroplasty.
Peer-review
This manuscript is well organized, and the results are acceptable.
Footnotes
Institutional review board statement: The study was approved by the IRB of the institution.
Informed consent statement: All the patients included in the study gave an informed consent for inclusion in the study.
Conflict-of-interest statement: No conflicts of interest to declare.
Data sharing statement: The authors are willing to share the data of the present study.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Peer-review started: January 14, 2016
First decision: February 29, 2016
Article in press: May 9, 2016
P- Reviewer: Camera A, Fujimoto E S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
References
- 1.Haritinian EG, Pimpalnerkar AL. Computer Assisted Total Knee Arthroplasty: Does it Make a Difference? Maedica (Buchar) 2013;8:176–181. [PMC free article] [PubMed] [Google Scholar]
- 2.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;(299):153–156. [PubMed] [Google Scholar]
- 3.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;(404):7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV. Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whiteside LA, Ohl MD. Tibial tubercle osteotomy for exposure of the difficult total knee arthroplasty. Clin Orthop Relat Res. 1990;(260):6–9. [PubMed] [Google Scholar]
- 6.Jerosch J, Peuker E, Philipps B, Filler T. Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc. 2002;10:194–197. doi: 10.1007/s00167-001-0271-x. [DOI] [PubMed] [Google Scholar]
- 7.Higuera CA, Deirmengian C. The new technologies in knee arthroplasty. J Clin Rheumatol. 2012;18:345–348. doi: 10.1097/RHU.0b013e3182724079. [DOI] [PubMed] [Google Scholar]
- 8.Tibesku CO, Innocenti B, Wong P, Salehi A, Labey L. Can CT-based patient-matched instrumentation achieve consistent rotational alignment in knee arthroplasty? Arch Orthop Trauma Surg. 2012;132:171–177. doi: 10.1007/s00402-011-1406-2. [DOI] [PubMed] [Google Scholar]
- 9.Bardakos N, Cil A, Thompson B, Stocks G. Mechanical axis cannot be restored in total knee arthroplasty with a fixed valgus resection angle: a radiographic study. J Arthroplasty. 2007;22:85–89. [Google Scholar]
- 10.Hinarejos P, Corrales M, Matamalas A, Bisbe E, Cáceres E. Computer-assisted surgery can reduce blood loss after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2009;17:356–360. doi: 10.1007/s00167-008-0683-y. [DOI] [PubMed] [Google Scholar]
- 11.Moon YW, Han JH, Lee KH, Jang SW, Seo JG. Clinical Outcome of IM-Guided Total Knee Arthroplasty with Inappropriate Femoral Resection in Coronal Plane. Knee Surg Relat Res. 2013;25:19–24. doi: 10.5792/ksrr.2013.25.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schnurr C, Csécsei G, Eysel P, König DP. The effect of computer navigation on blood loss and transfusion rate in TKA. Orthopedics. 2010;33:474. doi: 10.3928/01477447-20100526-08. [DOI] [PubMed] [Google Scholar]
- 13.Bae DK, Song SJ. Computer assisted navigation in knee arthroplasty. Clin Orthop Surg. 2011;3:259–267. doi: 10.4055/cios.2011.3.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng T, Pan XY, Mao X, Zhang GY, Zhang XL. Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee. 2012;19:237–245. doi: 10.1016/j.knee.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 15.Hamilton WG, Parks NL, Saxena A. Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty. 2013;28:96–100. doi: 10.1016/j.arth.2013.04.049. [DOI] [PubMed] [Google Scholar]
- 16.Chen JY, Yeo SJ, Yew AK, Tay DK, Chia SL, Lo NN, Chin PL. The radiological outcomes of patient-specific instrumentation versus conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22:630–635. doi: 10.1007/s00167-013-2638-1. [DOI] [PubMed] [Google Scholar]
- 17.Barrack RL, Ruh EL, Williams BM, Ford AD, Foreman K, Nunley RM. Patient specific cutting blocks are currently of no proven value. J Bone Joint Surg Br. 2012;94:95–99. doi: 10.1302/0301-620X.94B11.30834. [DOI] [PubMed] [Google Scholar]
- 18.Stronach BM, Pelt CE, Erickson J, Peters CL. Patient-specific total knee arthroplasty required frequent surgeon-directed changes. Clin Orthop Relat Res. 2013;471:169–174. doi: 10.1007/s11999-012-2573-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scholes C, Sahni V, Lustig S, Parker DA, Coolican MR. Patient-specific instrumentation for total knee arthroplasty does not match the pre-operative plan as assessed by intra-operative computer-assisted navigation. Knee Surg Sports Traumatol Arthrosc. 2014;22:660–665. doi: 10.1007/s00167-013-2670-1. [DOI] [PubMed] [Google Scholar]
- 20.Vaishya R, Singh AP, Vaish A. Outcome of subvastus approach in elderly nonobese patients undergoing bilateral simultaneous total knee arthroplasty: A randomized controlled study. Indian J Orthop. 2013;47:430–431. doi: 10.4103/0019-5413.114948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77–79. [PubMed] [Google Scholar]
- 22.Hafez MA, Chelule KL, Seedhom BB, Sherman KP. Computer-assisted total knee arthroplasty using patient-specific templating. Clin Orthop Relat Res. 2006;444:184–192. doi: 10.1097/01.blo.0000201148.06454.ef. [DOI] [PubMed] [Google Scholar]
- 23.Heyse TJ, Tibesku CO. Improved femoral component rotation in TKA using patient-specific instrumentation. Knee. 2014;21:268–271. doi: 10.1016/j.knee.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Renson L, Poilvache P, Van den Wyngaert H. Improved alignment and operating room efficiency with patient-specific instrumentation for TKA. Knee. 2014;21:1216–1220. doi: 10.1016/j.knee.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Abane L, Anract P, Boisgard S, Descamps S, Courpied JP, Hamadouche M. A comparison of patient-specific and conventional instrumentation for total knee arthroplasty: a multicentre randomised controlled trial. Bone Joint J. 2015;97-B:56–63. doi: 10.1302/0301-620X.97B1.34440. [DOI] [PubMed] [Google Scholar]
- 26.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty. 2008;23:26–29. doi: 10.1016/j.arth.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 27.Parratte S, Blanc G, Boussemart T, Ollivier M, Le Corroller T, Argenson JN. Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc. 2013;21:2213–2219. doi: 10.1007/s00167-013-2623-8. [DOI] [PubMed] [Google Scholar]
- 28.Stirling P, Valsalan Mannambeth R, Soler A, Batta V, Malhotra RK, Kalairajah Y. Computerised tomography vs magnetic resonance imaging for modeling of patient-specific instrumentation in total knee arthroplasty. World J Orthop. 2015;6:290–297. doi: 10.5312/wjo.v6.i2.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cenni F, Timoncini A, Ensini A, Tamarri S, Belvedere C, D’Angeli V, Giannini S, Leardini A. Three-dimensional implant position and orientation after total knee replacement performed with patient-specific instrumentation systems. J Orthop Res. 2014;32:331–337. doi: 10.1002/jor.22513. [DOI] [PubMed] [Google Scholar]
- 30.Ensini A, Timoncini A, Cenni F, Belvedere C, Fusai F, Leardini A, Giannini S. Intra- and post-operative accuracy assessments of two different patient-specific instrumentation systems for total knee replacement. Knee Surg Sports Traumatol Arthrosc. 2014;22:621–629. doi: 10.1007/s00167-013-2667-9. [DOI] [PubMed] [Google Scholar]
- 31.Koch P. MyKnee system: a new vision in total knee replacement. Maitrise Orthopédique. 2011;2:32–35. Available from: http://orthopaedie-unfallchirurgie.universimed.com/artikel/myknee-system-new-vision-total-knee-replacement. [Google Scholar]


