Abstract
Adolescent and Young Adult (AYA) cancer survivors manage an array of health-related issues. Survivorship Care Plans (SCPs) have the potential to empower these young survivors by providing information regarding treatment summary, late-effects of cancer therapies, healthy lifestyle guidance, coping with work-life-health balance, and follow-up care. However, current mHealth infrastructure used to deliver SCPs has been limited in terms of flexibility, engagement, and reusability. The objective of this study is to develop an ontology-driven survivor engagement framework to facilitate rapid development of mobile apps that are targeted, extensible, and engaging. The major components include ontology models, patient engagement features, and behavioral intervention technologies. We apply the proposed framework to characterize individual building blocks (“survivor digilegos”), which form the basis for mHealth tools that address user needs across the cancer care continuum. Results indicate that the framework (a) allows identification of AYA survivorship components, (b) facilitates infusion of engagement elements, and (c) integrates behavior change constructs into the design architecture of survivorship applications. Implications for design of patient-engaging chronic disease management solutions are discussed.
Keywords: Cancer survivor, Healthy lifestyle, Patient engagement, mHealth, Ontology
Introduction
The term “cancer survivor” refers to an individual who has been touched by cancer, right from the time of diagnosis, beyond the treatment, through the balance of one’s life [1]. The definition also includes family members, friends, and caregivers in addition to the patient, given the way cancer to a loved one can affect their lives. Recent estimates suggest that there are 14.5 million cancer survivors in the United States (US), and the projected numbers indicate a five million increase in the next decade [2]. Worldwide estimates of cancer survivors were 28.7 million in 2008 [3]. However, this reflects only the individuals within five years of diagnosis. In 2006, the Institute of Medicine’s landmark report on cancer survivorship highlighted key gaps in the existing care delivery infrastructure and provided several important recommendations for quality survivorship care to this growing population [4]. Cancer survivorship broadly refers to cancer-related physical and psychological issues, lifestyle after treatment such as returning to work, follow-up care, and prevention of secondary malignancies. Survivorship Care Plans (SCPs) provision to every patient is seen as a major step forward in facilitating the care transition from specialists to primary care physicians. These plans can form a communication bridge between physicians and survivors to ensure care quality and continuity, and also act as engagement tools that empower patients to self-manage care.
However, developing a SCP is complex, and a single form cannot address the changing needs of the survivors. The SCPs need to be comprehensive, yet uniquely patient-specific depending on type of primary cancer, age of diagnosis, current age, age-specific late effects of cancer, availability of familial support. In the global context, other aspects including, but not limited to, health beliefs, religious beliefs, and cultural context need to be considered when developing an SCP [5]. Particularly, Adolescent and Young Adult (AYA) cancer survivors’ needs demand special attention given the unique circumstances surrounding their survivorship and ever-changing scenarios of life [6]. An AYA survivor’s context of survivorship is dynamic given their transition from adolescence to adulthood, physiological and psychological growth, self-identity, separation from parents/family, career pursuits, and involvement in intimate relationships [7]. Therefore, engaging an AYA cancer survivor in health management involves the design of a multi-component solution, where the modules comprising the solution can be used across the care continuum based on patient-specific personalization attributes. Harnessing contemporary technology platforms such as online social media, mHealth applications allow us to generate cancer survivor engagement tools that are cost-effective, ubiquitous, and scalable. In this paper, we provide a novel methodological framework to enable the design of comprehensive and personalized mHealth solutions to engage AYA cancer survivors in healthy living. The framework utilizes ontology to integrate the Patient Engagement Framework (PEF) [8] and Behavioral Intervention Technology (BIT) Model [9] to develop survivor digilegos, which we consider as building blocks of mHealth solutions for AYA survivorship. The unique features of these digilegos are their reusability and customization abilities according to the survivor care context. These digilegos can be put together to build mHealth solutions that are flexible and extensible, yet comprehensive.
Research shows the use of ontology for the design of mHealth applications with a patient-centered focus, specifically for the purpose of self-monitoring [10–12]. Ontologies are suitable for storing and retrieving semantic information, or expressive knowledge, in machine-readable format [13].This information in the ontology can be used to evoke rule-based machine intelligence and decision-making provided through intrinsic reasoning capabilities and querying [14, 15]. Subsequently, PEF acts as a bridging tool to identify opportunities that can help translate the knowledge abstracted within the survivorship ontological representation to engagement elements of a consumer-centered application. Finally, the BIT model allows us to conceive and instantiate the survivor digilegos as technological constituents of the intended mHealth solution. In the next sections of the paper, we describe the framework components along with illustrative examples demonstrating its application to the domain of AYA cancer survivorship. Specifically, we focus on facilitating the development of mobile apps that engage AYA cancer survivors in follow-up care and healthy living through the digilego components.
Methods
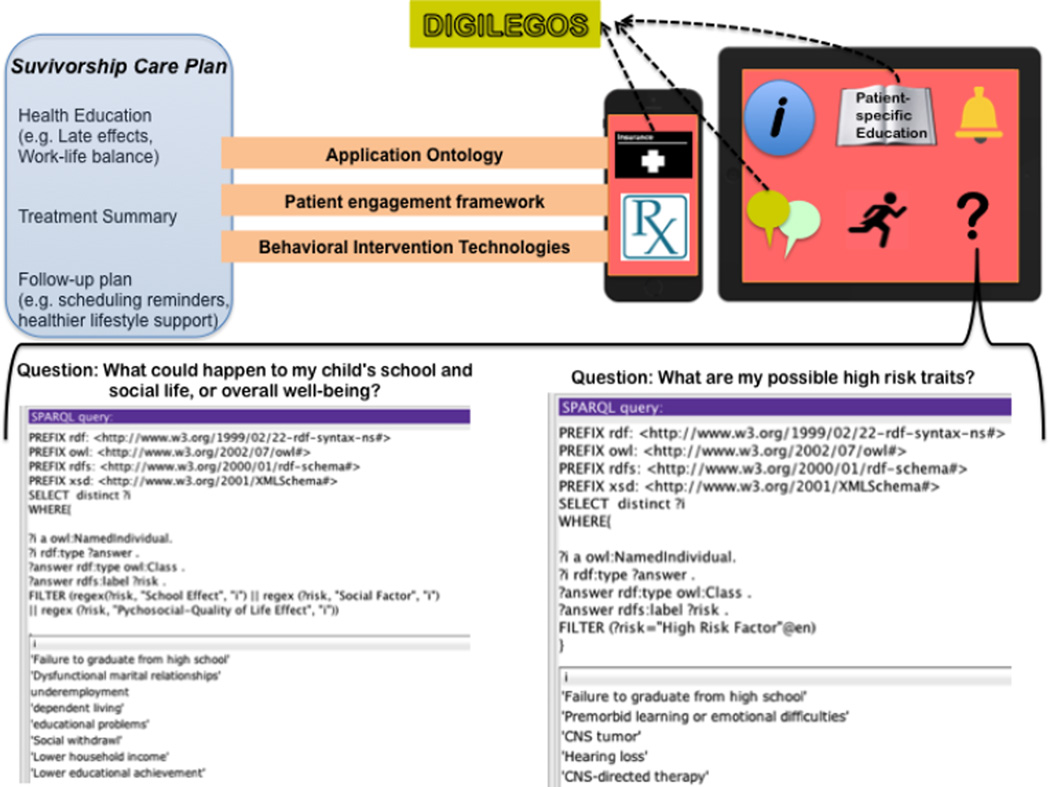
Figure 1 provides a high level representation of our proposed survivor engagement framework. The three main components are (1) Ontology Modeling, (2) Engagement Elements and Opportunities, and (3) Digilegos development using the BIT model.
Figure 1.
Proposed Survivor Engagement Framework for Development of Personalized mHealth Solution
Ontology Modeling
We constructed an application ontology called "Profile Ontology for Cancer Survivors" (POCS) to model and store knowledge of the patient's after-treatment care plan. The model was sourced from Long-Term Follow-Up (LTFU) guidelines put together for AYA survivors by the Children’s Oncology Group. The current draft of the POCS was built on top of the Friend of a Friend (FOAF) ontology model [16], which supported basic profile information of users and agents and also provided a template for associated documents, specifically the cancer survivor plan and its related information. The initial iteration of POCS was authored using Web Ontology Language (OWL), which is a W3C standard ontology language that supports standard knowledge representation and semantic reasoning [17], and was edited with Protégé, which is an open-source, commonly used ontology editor [18].
Engagement Elements
PEF has been developed by Healthcare Information and Management Systems Society (HIMSS) through cumulative layering of five phases- “inform me,” “engage me,” “empower me,” “partner with me,” and “support my e-community.” A total of nine features have been specified at the highest engagement level, including ‘information and way-finding’, ‘e-tools’, ‘forms’, ‘patient-specific education’, ‘patient access and use’, ‘patient-generated data’, ‘interoperable records’, ‘collaborative care and community support’ [8]. This framework was used in our study to sketch the functionality of mHealth infrastructure that potentially facilitates the adoption of SCPs, self-management, goal setting and reinforcement, peer support, and patient-provider communication. A mapping process was conducted too identify the engagement features that could be used to operationalize the POCS ontology classes. The ontological representations derived in the previous step allowed us to understand the characteristics of the information that should be delivered to the user through PEF features. We also specified the level of intended survivor engagement to characterize granularity and complexity of the system features.
Digilegos Development
We used the BIT model to conceptualize digilegos (which are individual and reusable ontology-driven mHealth components) to delineate the operational aims, identify behavior change strategies (where applicable), define user interactions, and outline technical aspects for real-time implementation [9]. The BIT model was originally proposed to develop behavioral interventions, however all digilegos did not have a behavioral component associated with them. For the non-behavioral ones, we still used the BIT model to ensure workflow alignment and smoother interfacing among all the digilegos. Certain digilegos were conceived to be integrated with advanced query and reasoning capabilities of POCS (see Figure 1). In the next sections, we describe the application of the proposed framework to develop AYA survivor digilegos using illustrative examples. Such compartmentalized design architecture of the survivor digilegos allowed us to facilitate customization, harness machine-based querying, integrate engagement tactics, and adopt theory-driven techniques that ultimately enable the development of user-empowering flexible mHealth tools that can be used across the cancer care continuum. Further, the workflow for each of the components has been set toment levels,vors to better mange stress as partof ed the constr
Results and Discussion
Ontology Modeling
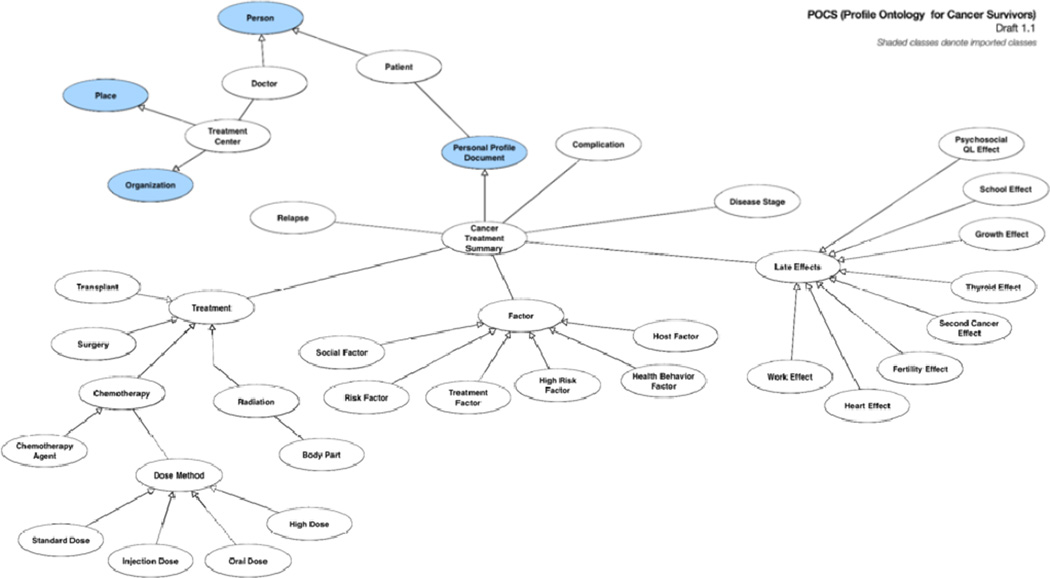
Figure 2 provides a general overview of POCS meta-level ontology. Information abstracted in POCS included end-user's personal information (e.g .marital status, age, gender), the patient's treatment information (complications, treatment type, follow-up schedules, late effects, etc.), and details of personal primary physician and related medical professionals. Initial metrics of our current draft include 58 classes and subclasses, 57 object properties, and 33 data properties. Rule-based intelligence and querying has been used to extract specific answers for survivors’ questions posted in lay vocabulary. Examples of questions include “what could happen to my child's school and social life, or overall well-being)?” and “What are my possible high risk traits?” A SPARQL query was used to approximate the question to obtain possible outcomes based on the information represented in the ontology. The integration pipeline for such ontology-driven queries in the proposed mHealth design framework is as follows. Intended steps include: (1) A custom web server application to host the live version of POCS and publish a private interface that will allow our application to query the ontology (2) A separate client-based application ontology that is based on POCS may reside on the application to store personalized information of the user and the user’s cancer survivor care information from the hosted POCS knowledge base.
Figure 2.
Profile Ontology for Adolescent and Young Adult Cancer Survivors
Identification of Engagement Elements
A total of five survivor engagement features were identified using PEF. Given the implementation and domain constraints, the engagement features fell under different phases of PEF. Table 1 provides a list of features and phases that were chosen as part of this step. Most engagement elements identified using the framework are in Level II. This mapping process allowed us to gain insights into the attainable level of survivor engagement, features to be incorporated, and reusable information classes across the features. Few engagement features that have been listed in Table 1 may be pertinent to only certain AYA user groups depending on their gender, age, and cancer type. Examples of such features include the fertility tracker, pregnancy tracker, late effect symptom checker, and lifestyle tips. The PEF framework is intended to guide healthcare organizations in developing and strengthening their patient engagement strategies. Our proposed survivor engagement framework is motivated by the need to support technology development efforts of consumer-centered apps by non-hospital entities. Therefore, certain advanced features listed in the PEF may not be applicable to our study limiting the scope of the engagement elements to Phase II. Such advanced features require constant data sharing with health institutions.
Table 1.
Engagement Features and Ontology Relations
| Engagement phase | Features | Related ontology classes |
|---|---|---|
Engage (Level II)
|
Information and Way finding |
Treatment center; Doctor; Late effects |
Engage (Level II)
|
e-Tools | Health behavior factor; Patient; Personal Profile; Risk factor; Social Factor |
| Create synergy and extend reach (Level V)
|
Patient- specific education |
Factor; Late effect; Treatment |
Engage (Level II)
|
Interactive forms |
Patient; Personal Profile; Treatment summary |
| Create synergy and extend reach (Level V)
|
Community support |
Patient; Social factor; Treatment Center; Doctor |
Digilego Development
A total of 11 survivor digilegos were conceived based on the engagement features selected using PEF. The individual components cover a variety of survivorship content and engage AYA survivors in care management. For example, “targeted health tips” provide patient-specific education to the survivor taking into consideration their current life scenario from the “personal profile” (e.g. age, gender, marital status). Our POCS ontology model forms the crux for the “late effect summarization” digilego to personalize content delivery that is cancer-specific, age-specific, and treatment-specific in nature. Table 2 provides an overview of the digilegos and the nature of content provided to the survivor. The overarching operational intention is to promote self-management of cancer care and survivorship among adolescents and young adults. Examples of the sub-goals for each component include increasing positive health behaviors such as physical activity, promoting social well-being through online community, facilitating accessibility to care summary and payment logistics, increasing knowledge levels pertaining to late effects specific to certain life events (such as planning for parenthood), and promoting adherence to a follow-up care regimen. The operational intention for each digilego is unique depending on the content specialty. The usage intention is the same across all components where the aim is to engage survivors in self-management of their health. Henceforth, social media features, a responsive question corner using ontology-driven methods that can process lay vocabulary, and personalization features have been integrated to the design framework of digilegos to promote user engagement.
Table 2.
Survivor Digilegos and their content specifics
| Survivor Digilegos |
Content specialty |
|---|---|
| Insurance information | |
| Health behavioral trackers | |
| Treatment summary | |
| Personalized late effects summarization |
|
| Follow-up care scheduling | |
| Personal profile | |
| Targeted health tips, education | |
| Transition assistance | |
| Lifestyle tips; Care reminders | |
| Social Hub | |
| Question corner |
Several behavior change techniques have been integrated with 7 out of the 11 digilegos shown in Table 2. Based on their proposed functionality, the theoretical underpinnings range from education to provide information on health-behavior links, general encouragement through feedback and self-monitoring via e-health tools such as health behavioral trackers, social support through the social hub and community interactions, follow-up prompts to promote self-monitoring behavior, and integration of relapse prevention and stress management tactics for transition assistance and work-life balance [19]. Mapping these strategies to digilego elements is straight-forward, given the clear formulation of the intentions of each component and strategy using the BIT model. For instance, “Social Hub” has been mapped to the social support strategy. Similarly, digilegos such as “Late Effects”, “Patient-specific education” have been designed to provide education on consequences, barriers, and benefits of in self-monitoring and management of cancer survivorship. Further, the instantiation criteria for each of the digilegos have been defined in terms of the interaction features and workflow. Notifications, logs, and information delivery are the most used interaction elements. For example, “Work-Life Balance” has interaction features, which include notifications to deliver daily reminders and information delivery mechanisms to provide multimedia educational content to AYA survivors. Similarly, logs have been assigned to “Personal profile”, messaging elements and visualizations to “Social Hub” to provide users with (a) communication tools to interact with peer and care providers, and (b) consolidated feedback to users on their social engagement levels. Event-based and time-based workflow criteria have been used to derive personalization effects. For instance, consider a change in education level where the user indicates entering college from high school, event-based criteria are used to deliver appropriate lifestyle tips and transition assistance guidelines that are pertinent to their life in college. Similarly, another event-based workflow is defined for “Late effects” and “Behavioral trackers”, where age-specific customizations will come to effect depending on the changes in life scenarios. In summary, a cluster of digilegos have been conceived, defined, and characterized using the BIT model to facilitate survivor engagement in cancer survivorship care. The use of ontology has facilitated the identification of abstract survivorship concepts and their interconnections to provide both general and personalized information. PEF and BIT models have provided a way to map and integrate user engagement attributes and theory-driven behavior change strategies.
A feature level comparison of the survivor digilegos and existing consumer apps available for AYA survivorship guidance is shown below in Table 3. We considered two apps, AYA Healthy Survivorship [20] and Cancer LateFX [21], developed by Cancer Alliance of Texas and Akron Children’s Hospital respectively. Both the apps derive their content from the same LTFU guidelines we used in the study. AYA Healthy Survivorship app focuses on healthy lifestyle promotion while the Cancer LateFX app offers content on late effect management of childhood cancer treatments. Social support features, behavioral goal trackers, profile information and treatment summary management are made available in both the apps and our digilegos. While a subset of features delivering patient education, lifestyle tips, care reminders, and a question corner were also found in both the apps, context-specific personalization (e.g. transition assistance) and ontology-driven reasoning capabilities have not been integrated into the existing apps. In summary, the use of detailed ontologies along with the PEF framework and BIT model has allowed rapid construction of survivor digilegos, which facilitate behavior change, consumer engagement, and optimal technology use for self-management of survivorship care among AYA survivors.
Table 3.
Quick comparison of features in existing consumer apps and the Survivor Digilegos
| Apps | Survivor Digilegos |
|---|---|
| AYA healthy survivorship |
|
| Cancer LateFX |
Limitations and Future Work
The POCS model described in the paper has been created with manual identification of classes. However, a scalable ontology generation will be made possible with the implementation of automated (or semi-automated) natural language processing methods. The use of external sources (e.g. the National Cancer Institute Thesaurus Ontology) allows us to generate comprehensive ontological models. PEF used in the proposed model is aimed at health institutions to develop solutions that are patient engaging. However, the framework is not completely suitable to identify engagement features for technology solutions that solely involve health consumers (e.g. AYA cancer survivors). Future research should focus on consumer engagement taxonomy and a framework that allows technology developers (1) to choose the appropriate level of complexity to model system features, and (2) to identify smoother ontology-to-end user knowledge transfer and query loops. Finally, the digilegos described in this paper have not yet been operationalized. Future research should implement and evaluate the digilegos in terms of user acceptance, reusability, and technology effectiveness. As part of the next steps, we aim at developing a mobile application comprising the survivor digilegos that will interface with POCS using OWL-based API libraries.
Conclusion
Cancer survivorship is a lifelong endeavor for cancer patients, their families, and caregivers. Better survivorship care is vital to enhance the quality of life during and after cancer treatments. With advancements in early detection and treatment protocols, the number of cancer survivors is on the rise around the globe. The proposed survivor engagement framework is a foundational step that will help influence the development of mobile applications with reusable and customizable components as per the needs of the cancer survivors across the care continuum. While the proposed framework is aimed at cancer survivorship, certain digilegos can be used to develop mobile solutions for management of any chronic disease (e.g. diabetes, cardiovascular health) that requires patient engagement and self-care. Use of informatics-driven methods, behavior change theories, and patient-centered design approaches can help us develop scalable and cost-effective mHealth products that can be deployed globally.
Acknowledgments
This research is partially supported by the National Library of Medicine of the National Institutes of Health under Award Number R01LM011829 to Dr. Cui Tao
References
- 1.National Cancer Institute. Office of Cancer Survivorship. [Last accessed 12/13/2014]; http://cancercontrol.cancer.gov/ocs/statistics/definitions.html.
- 2.DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, Alteri R, Robbins AS, Jemal A. Cancer treatment and survivorship statistics. Cancer J Clin. 2014;64(4):252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 3.Global survivorship statistics. [Last accessed 12/13/2014]; http://www.iarc.fr/index.php. [Google Scholar]
- 4.Hewitt M, Greenfield S, Stovall E, editors. From cancer patient to cancer survivor: lost in transition. National Academies Press; 2005. [Google Scholar]
- 5.Errico KM, Rowden D. Experiences of Breast Cancer Survivor Advocates and Advocates in Countries with Limited Resources: A Shared Journey in Breast Cancer Advocacy. The breast journal. 2006;12(s1):S111–S116. doi: 10.1111/j.1075-122X.2006.00208.x. [DOI] [PubMed] [Google Scholar]
- 6.Casillas J, Kahn KL, Doose M, Landier W, Bhatia S, Hernandez J, Zeltzer LK. Transitioning childhood cancer survivors to adult-centered healthcare: insights from parents, adolescent, and young adult survivors. Psycho-Oncology. 2010;19(9):982–990. doi: 10.1002/pon.1650. [DOI] [PubMed] [Google Scholar]
- 7.Pratt-Chapman M, Willis A, Bretsch J, Patiemo SR. Improving Cancer Survivorship for Adolescents and Young Adults. Journal of Oncology Navigation & Survivorship. 2013;4(1) [Google Scholar]
- 8.Patient Engagement Framework. [Last accessed 12/21/2014]; www.himss.org/ResourceLibrary/genResourceDetailPDF.aspx?ItemNumber=28305. [Google Scholar]
- 9.Mohr DC, Schueller SM, Montague E, Burns MN, Rashidi P. The Behavioral Intervention Technology Model: An Integrated Conceptual and Technological Framework for eHealth and mHealth Interventions. Journal of Medical Internet Research. 2014;16(6):e146. doi: 10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Villarreal V, Fontecha J, Hervas R, Bravo J. Mobile and ubiquitous architecture for the medical control of chronic diseases through the use of intelligent devices: Using the architecture for patients with diabetes. Future Gener. Comput. Syst. 2014;34:161–175. [Google Scholar]
- 11.Docksteader L, Benlamri R. Mobile Ontology-based Reasoning and Feedback health monitoring system; Digital Information Management, 2008. ICDIM 2008. Third International Conference on. IEEE; 2008. pp. 876–880. [Google Scholar]
- 12.Docksteader L, Benlamri R. MORF: A mobile health-monitoring platform. IT Prof. 2010;12(3):0018–0025. [Google Scholar]
- 13.Kim H-Y, Park H-A, Min YH, Jeon E. Development of an Obesity Management Ontology Based on the Nursing Process for the Mobile-Device Domain. J. Med. Internet Res. 2013;15(7):e130. doi: 10.2196/jmir.2512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skillen K-L, Chen L, Nugent CD, Donnelly MP, Burns W, Solheim I. Ontological user modelling and semantic rule-based reasoning for personalisation of Help-On-Demand services in pervasive environments. Future Gener. Comput. Syst. 2014;34:97–109. [Google Scholar]
- 15.Bickmore TW, Schulman D, Sidner CL. A reusable framework for health counseling dialogue systems based on a behavioral medicine ontology. Journal of biomedical informatics. 2011;44(2):183–197. doi: 10.1016/j.jbi.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The FOAF Project. [Last accessed 12/21/2014]; http://www.foaf-project.org/ [Google Scholar]
- 17.OWL API. [Last accessed 12/21/2014]; http://owlapi.sourceforge.net/ [Google Scholar]
- 18.Protégé. [Last accessed 12/21/2014]; http://protege.stanford.edu/ [Google Scholar]
- 19.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychology. 2008;27(3):379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 20.AYA Healthy Survivorship. [Last accessed 12/22/2014]; https://itunes.apple.com/us/app/aya-healthy-survivorship/id513642187. [Google Scholar]
- 21.CancerLateFX. [Last accessed 12/22/2014]; https://itunes.apple.com/us/app/cancerlatefx/id725634267?mt=8. [Google Scholar]