Figure 2.
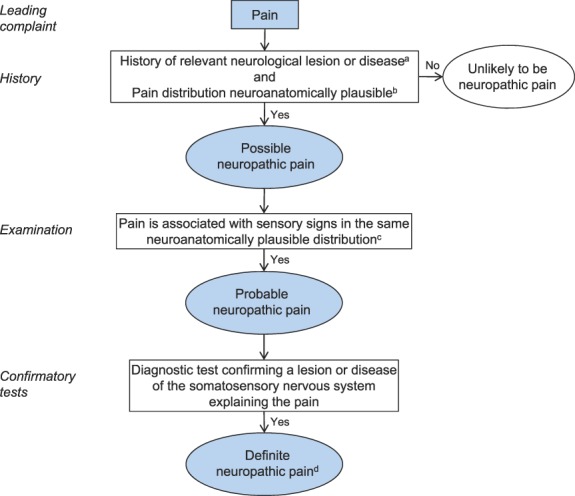
Flow chart of updated grading system for neuropathic pain. aHistory, including pain descriptors, the presence of nonpainful sensory symptoms, and aggravating and alleviating factors, suggestive of pain being related to a neurological lesion and not other causes such as inflammation or non-neural tissue damage. The suspected lesion or disease is reported to be associated with neuropathic pain, including a temporal and spatial relationship representative of the condition; includes paroxysmal pain in trigeminal neuralgia. bThe pain distribution reported by the patient is consistent with the suspected lesion or disease (Table 1). cThe area of sensory changes may extend beyond, be within, or overlap with the area of pain. Sensory loss is generally required but touch-evoked or thermal allodynia may be the only finding at bedside examination. Trigger phenomena in trigeminal neuralgia may be counted as sensory signs. In some cases, sensory signs may be difficult to demonstrate although the nature of the lesion or disease is confirmed; for these cases the level “probable” continues to be appropriate, if a diagnostic test confirms the lesion or disease of the somatosensory nervous system. dThe term “definite” in this context means “probable neuropathic pain with confirmatory tests” because the location and nature of the lesion or disease have been confirmed to be able to explain the pain. “Definite” neuropathic pain is a pain that is fully compatible with neuropathic pain, but it does not necessarily establish causality.
