Abstract
The superficial medial collateral ligament (sMCL) and associated knee structures are the most commonly injured structures of the knee. Most isolated sMCL tears are treated nonoperatively. Several studies have described different algorithms for treatment of sMCL lesions, as well as different types of techniques, both in the acute and in chronic settings. The purpose of this article was to detail our anatomic sMCL augmentation technique using semitendinosus and gracilis tendon autografts.
Superficial medial collateral ligament (sMCL) tears represent more than one-third of knee injuries.1 Most sMCL tears are treated nonoperatively. However, some require surgical intervention in the acute setting or when nonoperative treatment fails.2 Several surgical techniques have been described for reconstruction and augmentation of sMCL lesions. Most authors now agree that anatomical restoration of the sMCL is the key point in re-establishing native knee biomechanics.3
The posteromedial knee complex is composed of the sMCL, the posterior oblique ligament (POL), and the deep medial collateral ligament (MCL).4 These structures are the primary and secondary static stabilizers against valgus stress, and for external and internal rotational stability.4, 5 Anatomic and biomechanical studies have been performed to examine the insertion sites and the functionality of the individual components of the medial structures of the knee to ultimately develop an anatomical augmentation technique.6, 7 The purpose of this study was to describe an anatomic augmentation technique for the sMCL with semitendinosus and gracilis tendon autografts.
Objective Diagnosis
Stress radiographs are essential for the objective diagnosis of sMCL lesions.8 Bilateral valgus stress radiographs should be performed at 20° of knee flexion. Medial gapping should be measured by taking the shortest distance between the subchondral bone surface of the most distal aspect of the medial femoral condyle and the corresponding medial tibial plateau. The results of the uninjured knee and the injured knee should then be compared.2
The current diagnostic algorithm of the senior author (R.F.L.) for a complete lesion of the sMCL is a difference of 3.2-mm gapping at 20° of knee flexion. The criterion for a complete tear of all structures of the posteromedial complex is a difference of 9.8-mm gapping at 20° of knee flexion.9, 10, 11, 12 Magnetic resonance imaging (MRI) is useful to diagnose acute medial knee lesions, to determine the location of the damaged structures and to assess concurrent injuries.
Indications
Acute isolated grade III sMCL tears are typically initially treated nonoperatively. In addition, combined anterior cruciate ligament (ACL) and sMCL injuries are usually treated first nonoperatively with rehabilitation, focusing on letting the sMCL injury heal, followed by ACL reconstruction. Surgical management of acute sMCL injuries is indicated when there are multiligament injuries or knee dislocation involving the sMCL.2, 13
For chronic grade III MCL injuries, surgery is indicated when functional rotatory or side-to-side instability persists despite conservative therapy, including bracing and a rehabilitation program for at least 6 weeks after injury. Patients with valgus malalignment should undergo a distal femoral osteotomy before sMCL reconstruction because of increased stress placed on the graft due to the malalignment. Valgus malalignment is identified when the mechanical axis lies lateral to the apex of the lateral tibial eminence. In this situation, preoperative planning aims to shift the mechanical axis to pass through the apex of the medial tibial eminence. If an osteotomy was performed, sMCL reconstruction is only indicated if instability continues after healing of the osteotomy and participation in a rehabilitation program.2, 13
Surgical Technique
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table (Video 1). After induction of general anesthesia, a bilateral knee examination is performed to evaluate the degree of ligamentous instability. A well-padded high-thigh tourniquet is subsequently placed on the operative leg and then it is placed into a leg holder (Mizuho OSI, Union City, CA), whereas the contralateral knee is placed into an abduction stirrup (Birkova Product LLC, Gothenburg, NE). The foot of the operating table is then lowered, allowing for the surgeon to freely manipulate the knee as needed (Fig 1).
Fig 1.
Patient positioning on the operating table. The surgical limb (left) is placed into leg holder allowing the surgeon to freely manipulate the knee during the procedure. Nonoperating limb is kept on a well-padded abduction stirrup.
Technique
A skin incision is made on the anteromedial aspect of the knee and centered over the joint line. Proximally, the incision is performed between the adductor tubercle (AT) and the medial aspect of the patella, and extending distally over the midportion of the tibia approximately 7 to 8 cm distal to the joint line.3, 6, 7 In cases of concomitant ACL or posterior cruciate ligament injury, this approach facilitates the creation of the tibial tunnels for cruciate ligament reconstruction. Care must be taken to avoid the saphenous nerve, which courses 5 cm posteriorly to the AT.13 Blunt dissection is performed down to the sartorial fascia, which should be left intact, and the pes anserinus tendons are identified. Watchful inspection must be done to precisely identify all injured structures. In chronic cases, where the anatomy may be distorted, this inspection can be challenging. After isolating the semitendinosus and the gracilis tendons and releasing them from adhesions, an open-ended hamstring stripper (Smith & Nephew, Andover, MA) is used to detach them proximally, while preserving their distal insertions (Fig 2).
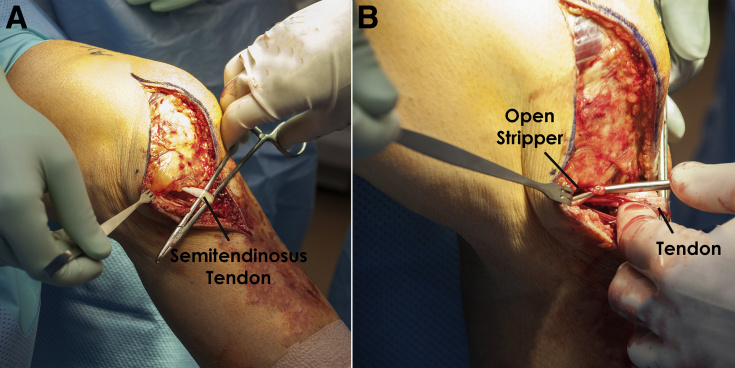
Fig 2.
Left knee image showing (A) identification and isolation of the semitendinosus tendon and (B) the harvest of the semitendinosus tendon with an open-ended hamstring striper, while preserving the tibial insertion. The same steps are repeated for the harvest of the gracilis tendon.
Ideally, a remnant of the distal insertion of the sMCL is identified 6 or 7 cm distal to the joint line on the posterior aspect of the medial tibia.3, 4, 6, 7 The use of a spinal needle marking the medial joint line and a ruler helps the surgeon to identify this point (Fig 3). After measuring the distance, 2 double-loaded suture anchors (Mitek, Westwood, MA) are then fixed. The first is placed as far posterior as possible, on the posteromedial aspect of the tibia. The second anchor is placed slightly anterior and proximal to the first one in order to avoid convergence and allow room to suture the hamstrings in between them (Fig 4). Both grafts are then sutured to the tibia at this location (keeping their distal insertion) along with any remnant tissue of the sMCL (Fig 5). A small incision is then made in line with the sartorial fascia fibers to create a passage through which the semitendinosus and the gracilis grafts are passed.
Fig 3.
Intraoperative image of left knee showing the joint line marked with a spinal needle and a ruler used to identify the distal tibial attachment of the superficial medial collateral ligament, 6 cm distal to the joint line.
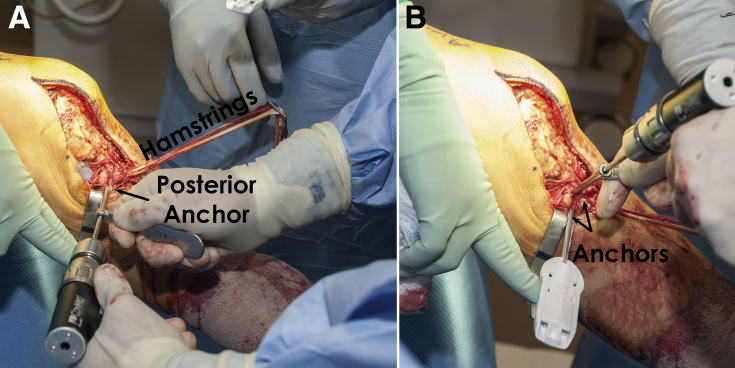
Fig 4.
Intraoperative image of a left knee showing the correct placement of (A) first tibial distal suture anchor at the posteromedial crest of the tibia and (B) second tibial distal suture anchor slightly anterior and superior to the first one. Note that both anchors are placed in a converging direction around the posteromedial aspect of the tibia in a way that the grafts (as well as any superficial medial collateral ligament remnant) will remain between them.
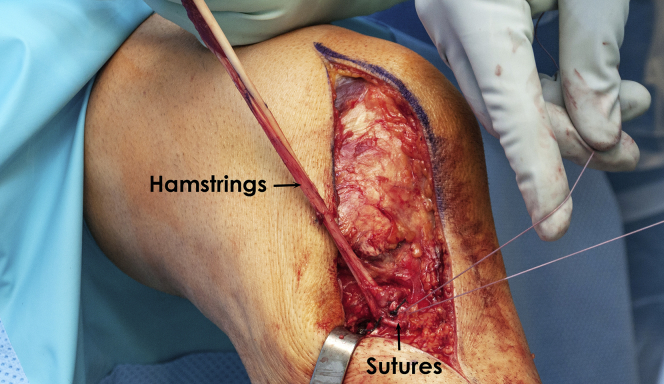
Fig 5.
The distal tibial fixation of the superficial medial collateral ligament (sMCL) augmentation reconstruction is complete. Note that both hamstrings are tied together between the 2 suture anchors previously placed in the posteromedial aspect of the tibia. Any identified sMCL remnant should be tied along with the sutures.
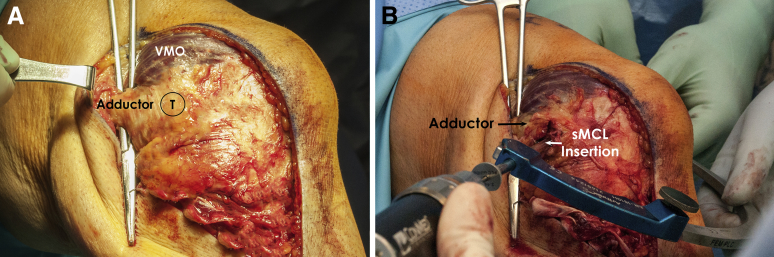
Attention is then turned to the proximal aspect of the reconstruction. It is important to initially locate the adductor magnus tendon (AMT), because it will guide the surgeon to find the AT and ultimately all the important landmarks in the medial aspect of the knee. To isolate the AMT, the surgeon should follow the medial aspect of the vastus medialis obliquus and bluntly dissect the interval between this muscle and the AMT (Fig 6A). After isolating the AMT, it becomes easier to follow it and locate the AT. If the surgeon still has difficulty in locating the tubercle, he can apply traction to the tendon and follow its path by palpation. Of note, the AT constitutes the most reliable surgical landmark for the senior author (R.F.L.). To locate the femoral insertion of the sMCL, the surgeon should first identify the medial epicondyle, which is located 12.6 mm distal and 8.3 mm anterior to the AT.4 The sMCL insertion can then be identified 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle.4
Fig 6.
Intraoperative pictures of a left knee showing (A) identification of the adductor magnus tendon following the medial border of the vastus medialis obliquus (VMO) muscle and (B) passage of a guide pin into the proximal attachment site of the superficial medial collateral ligament (sMCL) on the femur. It is recommended to use an aiming device to make sure that the exit point will be located slightly anterior and proximal relative to the entry point to avoid damaging the trochlea or collision with other tunnels in multiligament cases.
Once the femoral attachment of the sMCL is found, sharp dissection is performed down to the bone to clear the area from soft tissues. An eyelet pin is placed at this point with an aiming guide (Arthrex, Naples, FL) exiting anterior and proximal, to avoid the trochlea and tunnel convergence in multiligament cases (Fig 6B). A 7-mm tunnel is then over-reamed (Reamer, Arthrex) to a depth of 35 mm to create a socket and a passing suture is placed to facilitate later grafts passage. The semitendinosus and the gracilis grafts are then marked 30 mm proximal to the distance between their distal insertion and the entrance of the tunnel (Fig 7A). A whipstitched suture is applied over the mark and the excess length of the grafts are amputated (Fig 7B).
Fig 7.
Intraoperative images of a left knee showing (A) marking of the graft with a surgical pen 3 cm beyond its distance to the entrance of the tunnel (this mark will guide the further whipstitching) and (B) amputation of the excess of grafts. The sutures placed into the grafts will be transported to the lateral side of the knee with the aid of a passing suture previously left into the tunnel.
Both grafts are then pulled into the femoral tunnel using the passing suture previously left in place, and the knee is positioned at 20° of flexion with neutral rotation. At this position, the surgeon applies a gentle varus force reduction and a 7 × 25 mm bioabsorbable screw (Arthrex) is used to fix the graft in place, whereas the assistant applies traction to the suture.
For the purpose of reproducing the proximal tibial attachment of the sMCL, a third double-loaded suture anchor (Mitek) is inserted 12 mm distal to the joint line, directly over the most anterodistal attachment of the anterior arm of the semimembranosus, securing the graft to the proximal tibial attachment of the sMCL. To accurately place this last anchor, it is advisable to use the same previously described measuring technique, making use of a spinal needle to define the joint line. Once the anchor is placed, the sutures are tied to the grafts with the knee positioned at 20° of flexion and neutral rotation. No varus force is needed at this time. A schematic illustration of this procedure is shown in Figure 8.
Fig 8.
Final aspect of the superficial medial collateral ligament (sMCL) augmentation technique. The proximal tibial suture anchor reproduces the proximal attachment of the sMCL on the tibia, 12 mm below the joint line. The distal tibial attachment is reconstructed with 2 double-loaded suture anchors. Any remnant of the native sMCL should be tied along with the hamstrings, which remain attached distally. (VMO, vastus medialis obliquus.)
(Adapted with permission from Wijdicks et al.6)
Once fixation is complete, the knee is flexed to determine the “safe zone” range of movement, which can be initiated on postoperative day 1. It is important that the sMCL graft is able to be fully flexed with no excessive tension through a full range of knee motion.
Postoperative Rehabilitation
As one of the main concerns after this surgery is the prevention of arthrofibrosis, a rehabilitation protocol based on early mobilization should be adopted. A supervised postoperative rehabilitation should begin on day 1 with knee motion within the safe zone for the first 2 weeks after surgery.13 Quadriceps strengthening exercises and patellar mobilization are also recommended. After the first 2 weeks range of movement should be allowed as tolerated. Weightbearing should begin after 6 weeks, with training on how to avoid pivoting to prevent graft stretching. Excessively stressing of the joint should be avoided to decrease the risk of effusions. At 16 to 20 weeks, further lower extremity strength training and proprioception exercises should be initiated, depending on whether the patient had an isolated or multiligament reconstruction. Return to sports and other activities will be based on functional tests and valgus stress radiographs.14 Pearls and pitfall to performing this surgical procedure are listed in Table 1.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| • Anteromedial incision in cases of combined medial and cruciate ligaments injury makes it easier to drill the tunnels. • Distal suture anchors should be placed as far posterior as possible on the posteromedial corner of the tibia. • Identifying the adductor tubercle tendon helps locate bony prominences in the medial aspect of femoral condyle. • Femoral fixation should be performed at 20° while applying a gentle varus force. |
• Making the incision too posterior can put the saphenous nerve at risk. • Not applying varus stress when securing the graft to the femur can result in residual uncorrected laxity. • Failure to initiate a prompt rehabilitation program after surgery increases the risk of arthrofibrosis. |
Discussion
This sMCL augmentation technique using semitendinosus and gracilis tendon autograft has been reported to restore near native medial stability of the knee.3, 6
In regard to diagnosis, stress radiographs should be used in all patients with a clinical suspicion of a medial side injury. LaPrade et al.8 reported that the amount of medial compartment gapping can be quantified on valgus stress radiographs for medial knee injuries in the acute and chronic settings. In addition, the use of MRI is recommended to diagnose the location of the damaged structures and any concomitant lesions. Yao et al.15 reported an accuracy of 87% in diagnosing medial knee injuries with MRI. In a prospective study, Miller et al.16 reported a 45% incidence of lateral compartment bone bruises with an isolated injury of the MCL.
Other reconstruction techniques have been reported. Kim et al.17 and Lind et al.18 reported on the use of semitendinosus autograft leaving the pes anserinus insertion intact. The graft is subsequently secured at the femoral insertion of the sMCL, and the free end of the remaining tendon is used to reconstruct the POL. The technique by Kim et al.17 loops the free end around the direct head of the semimembranosus. The method used by Lind et al.18 involved drilling a tibial tunnel (posterior and lateral to the semimembranosus insertion) to pull the graft. Both techniques have been reported to restore normal or near-normal medial laxity 2 years after surgery.
When there is a side-to-side difference between 3.2 and 9.8 mm gapping in stress radiographs, an augmentation procedure can be performed. However, when a complete tear of all structures of the posteromedial complex is suspected (>9.8 mm difference) or severe rotational instability exists, the POL should be reconstructed in addition to the sMCL.
LaPrade and Wijdicks3 reported good results with both augmentation and reconstruction techniques of sMCL lesions. Both techniques have been shown to restore normal laxity of the joint in the most tested conditions.3, 6 Long-term studies should be performed to ensure the maintenance of the restoration, stability, and functionality of the knee. We encourage other groups to test the validity of this technique to assess for long-term results.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.F.L. receives support from Arthrex; Ossur; Siemans; Smith & Nephew; Health East, Norway; and a National Institutes of Health R13 grant for biologics.
Supplementary Data
Demonstration of anatomic augmentation of superficial medial collateral ligament (sMCL) with semitendinosus and gracilis tendon autograft. With the patient placed supine on the operating table, an examination under anesthesia is performed. A hockey stick shaped incision is made on the anteromedial aspect of the knee and centered over the joint line. Proximally, the incision is performed between the adductor tubercle (AT) and the medial aspect of the patella, and is extended distally over the midportion of the tibia, approximately 7 to 8 cm distal to the joint line. Blunt dissection is performed down to the sartorial fascia. The semitendinosus and the gracilis tendons are harvested, being cautious to preserve their distal insertions. Ideally, a remnant of the distal insertion of the sMCL is found, located 6 cm distal to the joint line on the posterior aspect of the medial tibia. Two double-loaded suture anchors are fixed to this point, near the posteromedial angle of the tibia, and both tendons are secured to the distal tibial sMCL attachment site, along with any remnant sMCL tissue. Next, the adductor magnus tendon is located and the AT is used as a landmark. To locate the femoral insertion of the sMCL, first identify the medial epicondyle, which is located 12.6 mm distal and 8.3 mm anterior to the AT. The sMCL insertion can then be located 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. The insertion site is cleaned of soft tissue. An eyelet pin is placed at the femoral insertion point with an aiming guide exiting anterolaterally and proximal, to avoid the trochlea and tunnel convergence in multiligament cases. A 7-mm tunnel is then reamed over the eyelet pin to a depth of 35 mm to create a closed socket and a passing suture is placed. The semitendinosus and the gracilis grafts are then passed under the fibers of the sartorial fascia. The semitendinosus and the gracilis grafts are then measured and marked along a 30-mm length to fit the socket. The grafts are then whipstitched according to the surgical pen marking and the excess graft is amputated. The end of the graft is then pulled into the femoral tunnel using the passing suture. With the knee positioned at 20° of flexion and neutral rotation, a gentle varus force is applied and a 7 × 23 mm bioabsorbable interference screw is used to fix the graft in place while the assistant applies traction to the suture laterally. After secure fixation is confirmed and valgus stability is assessed, the proximal tibial attachment of the graft is reproduced. To reproduce the proximal tibial attachment of the sMCL, the medial joint line is identified with a spinal needle and a third anchor is inserted 12 mm distal to the joint line, directly over the most anterodistal attachment of the anterior arm of the semimembranosus, securing the graft to the proximal tibial attachment of the sMCL. This patient also underwent concurrent posterior cruciate ligament reconstruction, and the anteromedial incision was extended distally to ream the posterior cruciate ligament tibial tunnel. After graft fixation, a complete knee examination is performed to verify the stability of the augmentation reconstruction. The wound is then closed and the operation is completed.
References
- 1.Bollen S. Epidemiology of knee injuries: Diagnosis and triage. Br J Sports Med. 2000;34:227–228. doi: 10.1136/bjsm.34.3.227-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.LaPrade R.F., Wijdicks C.A. The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther. 2012;42:221–233. doi: 10.2519/jospt.2012.3624. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R.F., Wijdicks C.A. Surgical technique: Development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. 2012;470:806–814. doi: 10.1007/s11999-011-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 5.Griffith C.J., LaPrade R.F., Johansen S., Armitage B., Wijdicks C., Engebretsen L. Medial knee injury: Part 1, static function of the individual components of the main medial knee structures. Am J Sports Med. 2009;37:1762–1770. doi: 10.1177/0363546509333852. [DOI] [PubMed] [Google Scholar]
- 6.Wijdicks C.A., Michalski M.P., Rasmussen M.T. Superficial medial collateral ligament anatomic augmented repair versus anatomic reconstruction: An in vitro biomechanical analysis. Am J Sports Med. 2013;41:2858–2866. doi: 10.1177/0363546513503289. [DOI] [PubMed] [Google Scholar]
- 7.Deo S., Getgood A. A technique of superficial medial collateral ligament reconstruction using an adjustable-loop suspensory fixation device. Arthrosc Tech. 2015;3:e261–e265. doi: 10.1016/j.eats.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LaPrade R.F., Bernhardson A.S., Griffith C.J., Macalena J.A., Wijdicks C.A. Correlation of valgus stress radiographs with medial knee ligament injuries: An in vitro biomechanical study. Am J Sports Med. 2010;38:330–338. doi: 10.1177/0363546509349347. [DOI] [PubMed] [Google Scholar]
- 9.Hughston J.C. Acute knee injuries in athletes. Clin Orthop. 1962;23:114–133. [PubMed] [Google Scholar]
- 10.LaPrade R.F., Terry G.C. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25:433–438. doi: 10.1177/036354659702500403. [DOI] [PubMed] [Google Scholar]
- 11.Phisitkul P., James S.L., Wolf B.R., Amendola A. MCL injuries of the knee: Current concepts review. Iowa Orthop J. 2006;26:77–90. [PMC free article] [PubMed] [Google Scholar]
- 12.Deo J.D., Hosey R.G. Medial and lateral collateral injuries: Prognosis and treatment. Prim Care. 2004;31:957–975. doi: 10.1016/j.pop.2004.07.005. ix. [DOI] [PubMed] [Google Scholar]
- 13.Wijdicks C.A., Griffith C.J., Johansen S., Engebretsen L., LaPrade R.F. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92:1266–1280. doi: 10.2106/JBJS.I.01229. [DOI] [PubMed] [Google Scholar]
- 14.Bahk M.S., Cosgarea A.J. Physical examination and imaging of the lateral collateral ligament and posterolateral corner of the knee. Sports Med Arthrosc. 2006;14:12–19. doi: 10.1097/00132585-200603000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Yao L., Dungan D., Seeger L.L. MR imaging of tibial collateral ligament injury: Comparison with clinical examination. Skeletal Radiol. 1994;23:521–524. doi: 10.1007/BF00223082. [DOI] [PubMed] [Google Scholar]
- 16.Miller M.D., Osborne J.R., Gordon W.T., Hinkin D.T., Brinker M.R. The natural history of bone bruises. A prospective study of magnetic resonance imaging-detected trabecular microfractures in patients with isolated medial collateral ligament injuries. Am J Sports Med. 1998;26:15–19. doi: 10.1177/03635465980260011001. [DOI] [PubMed] [Google Scholar]
- 17.Kim S.J., Lee D.H., Kim T.E., Choi N.H. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br. 2008;90:1323–1327. doi: 10.1302/0301-620X.90B10.20781. [DOI] [PubMed] [Google Scholar]
- 18.Lind M., Jakobsen B.W., Lund B., Hansen M.S., Abdalla O., Christiansen S.E. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med. 2009;37:1116–1122. doi: 10.1177/0363546509332498. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demonstration of anatomic augmentation of superficial medial collateral ligament (sMCL) with semitendinosus and gracilis tendon autograft. With the patient placed supine on the operating table, an examination under anesthesia is performed. A hockey stick shaped incision is made on the anteromedial aspect of the knee and centered over the joint line. Proximally, the incision is performed between the adductor tubercle (AT) and the medial aspect of the patella, and is extended distally over the midportion of the tibia, approximately 7 to 8 cm distal to the joint line. Blunt dissection is performed down to the sartorial fascia. The semitendinosus and the gracilis tendons are harvested, being cautious to preserve their distal insertions. Ideally, a remnant of the distal insertion of the sMCL is found, located 6 cm distal to the joint line on the posterior aspect of the medial tibia. Two double-loaded suture anchors are fixed to this point, near the posteromedial angle of the tibia, and both tendons are secured to the distal tibial sMCL attachment site, along with any remnant sMCL tissue. Next, the adductor magnus tendon is located and the AT is used as a landmark. To locate the femoral insertion of the sMCL, first identify the medial epicondyle, which is located 12.6 mm distal and 8.3 mm anterior to the AT. The sMCL insertion can then be located 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. The insertion site is cleaned of soft tissue. An eyelet pin is placed at the femoral insertion point with an aiming guide exiting anterolaterally and proximal, to avoid the trochlea and tunnel convergence in multiligament cases. A 7-mm tunnel is then reamed over the eyelet pin to a depth of 35 mm to create a closed socket and a passing suture is placed. The semitendinosus and the gracilis grafts are then passed under the fibers of the sartorial fascia. The semitendinosus and the gracilis grafts are then measured and marked along a 30-mm length to fit the socket. The grafts are then whipstitched according to the surgical pen marking and the excess graft is amputated. The end of the graft is then pulled into the femoral tunnel using the passing suture. With the knee positioned at 20° of flexion and neutral rotation, a gentle varus force is applied and a 7 × 23 mm bioabsorbable interference screw is used to fix the graft in place while the assistant applies traction to the suture laterally. After secure fixation is confirmed and valgus stability is assessed, the proximal tibial attachment of the graft is reproduced. To reproduce the proximal tibial attachment of the sMCL, the medial joint line is identified with a spinal needle and a third anchor is inserted 12 mm distal to the joint line, directly over the most anterodistal attachment of the anterior arm of the semimembranosus, securing the graft to the proximal tibial attachment of the sMCL. This patient also underwent concurrent posterior cruciate ligament reconstruction, and the anteromedial incision was extended distally to ream the posterior cruciate ligament tibial tunnel. After graft fixation, a complete knee examination is performed to verify the stability of the augmentation reconstruction. The wound is then closed and the operation is completed.