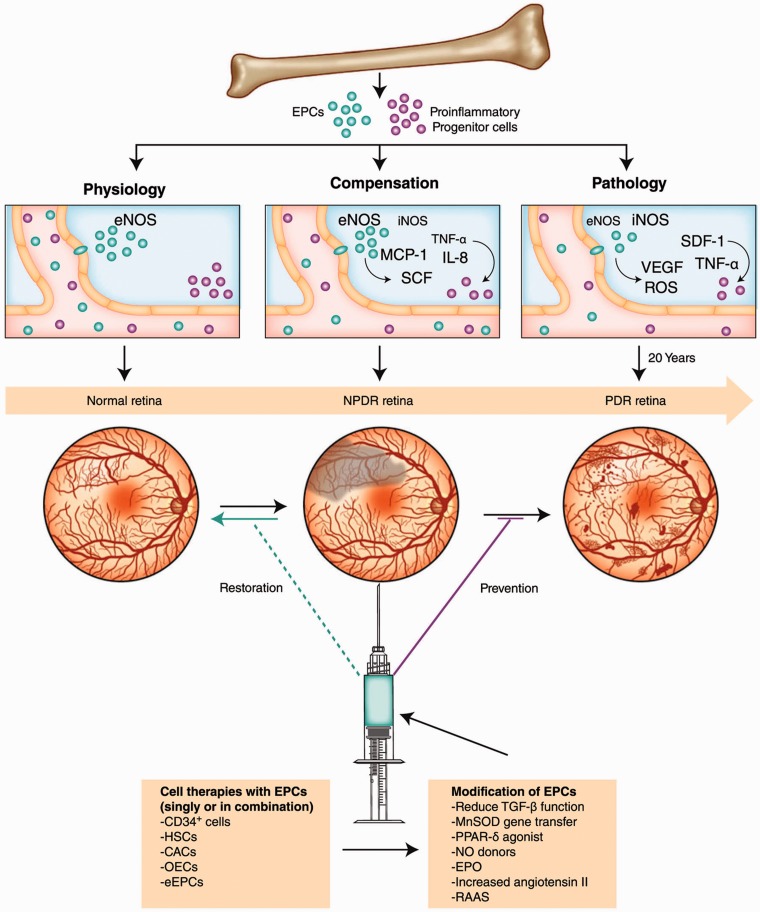
Figure 2.
Diabetic dysfunction in the BM mobilization of stem/progenitor cells and paracrine regulation of ischemic vascular repair. In normal conditions, factors released by ischemic/injured tissue cause mobilization of BM cells. In diabetes, there is reduced mobilization of BM cells into circulation. Cell therapy in diabetic retinopathy would ideally restore perfusion to areas of the retina that have undergone vasodegeneration associated with NPDR and would prevent the development of advanced disease, PDR
BM: bone marrow; CACs: circulating angiogenic cells; eEPCs: early endothelial progenitor cells; eNOS: endothelial nitric oxide synthase; EPCs: endothelial progenitor cells; EPO: erythropoietin; HSCs: hematopoietic stem cells; IL: interleukin; iNOS: inducible nitric oxide synthase; MCP-1: monocyte chemoattractant protein-1; MnSOD: manganese superoxide dismutase; NO: nitric oxide; NPDR: nonproliferative diabetic retinopathy; OECs: outgrowth endothelial cells; PDR: proliferative diabetic retinopathy; PPAR-δ: peroxisome proliferator-activated receptor-δ; RAAS: renin-angiotensin-aldosterone system; ROS: reactive oxygen species; SCF: stem cell factor; SDF-1: stromal cell–derived factor-1; TGF-β: transforming growth factor-β; TNF-α: tumor necrosis factor-α; VEGF: vascular endothelial growth factor. Reproduced with permission from Shaw et al.21 (A color version of this figure is available in the online journal.)