Abstract
This single center cohort study aimed to test the hypothesis that use of a cryopreserved arterial allograft could avoid the maturation or healing process of a new vascular access and to evaluate the patency of this technique compared with that of vascular access using a prosthetic graft. Between April 2012 and March 2013, 20 patients underwent an upper arm vascular access using a cryopreserved arterial allograft for failed or failing vascular accesses and 53 using a prosthetic graft were included in this study. The mean duration of catheter dependence, calculated as the time interval from upper arm access placement to removal of the tunneled central catheter after successful cannulation of the access, was significantly longer for accesses using a prosthetic graft than a cryopreserved arterial allograft (34.4 ± 11.39 days vs. 4.9 ± 8.5 days, P < 0.001). In the allograft group, use of vascular access started within 7 days in 16 patients (80%), as soon as from the day of surgery in 10 patients. Primary (unassisted; P = 0.314) and cumulative (assisted; P = 0.673) access survivals were similar in the two groups. There were no postoperative complications related to the use of a cryopreserved iliac arterial allograft except for one patient who experienced wound hematoma. In conclusion, upper arm vascular access using a cryopreserved arterial allograft may permit immediate hemodialysis without the maturation or healing process, resulting in access survival comparable to that of an access using a prosthetic graft.
Keywords: Allografts, Cryopreservation, Renal Insufficiency, Vascular Access Devices
Graphical Abstract
INTRODUCTION
Morbidity and mortality in end-stage renal disease (ESRD) patients undergoing hemodialysis have been associated with dialysis efficiency (1). International guidelines recommend an autogenous arteriovenous fistula (AVF), created in the arm, for safe and long-term vascular access (1,2,3). However, short- and long-term AVF dysfunction, including failed maturation, vein thrombotic occlusion, aneurysmal changes, and infection, are the major causes of morbidity and hospitalization in hemodialysis patients. Indeed, the primary patency rate of AVFs at 2 years was recently estimated to be less than 60% (4). Pooled data for the DOQI analysis suggested that the primary patency rate of arteriovenous prosthetic dialysis grafts (AVGs) was approximately 50% at 1 year, although other studies have reported primary patency rates as low as 23% at 1 year and 4% at 2 years (5). Therefore, salvaging a failed or failing vascular access can also prevent the need for use of a central venous catheter or a new prosthetic vascular access. However, urgent dialysis via a temporary central venous catheter is required and may be life-saving for chronic hemodialysis patients with a non-salvageable, failed or failing vascular access. Although various techniques have been reported to reduce temporary hemodialysis catheter-related complications, mechanical and infectious complications related to the insertion of temporary hemodialysis catheter can be fatal (6). Cryopreserved cadaveric vascular allografts offer the potential advantage of decreased infection (7) and could be used as an effective alternative to salvage a failed or failing vascular access in an infected graft environment.
This single center cohort study assessed the ability of a cryopreserved iliac arterial allograft from a deceased donor to act as a vascular conduit in patients with failed or failing vascular access, non-salvageable by any surgical or endovascular revision procedures. This study also evaluated the ability of this technique to permit immediate hemodialysis without the use of a central venous catheter. In addition, primary (unassisted) and cumulative (assisted) access survivals were compared in patients undergoing vascular access using a cryopreserved arterial allograft and a prosthetic graft.
MATERIALS AND METHODS
Study design and patient population
Between April 2012 and March 2013, 386 vascular accesses were created to enable hemodialysis at our institution. Of these 386 operations, 20 (5.2%) established an upper arm vascular access using a cryopreserved iliac arterial allograft from a deceased donor. Patients were included in this group if they 1) had ESRD treated chronically by hemodialysis, 2) provided informed consent, 3) had no option for salvaging dysfunctional vascular access and no adequate potential future access site, and 4) were not candidates for renal transplantation. ABO blood type compatibility was not considered in the inclusion criteria. No tissue matching was performed and no immunosuppression was given to the patients. To compare the patency of this technique, patients with an upper arm vascular access using a prosthetic graft during the same study period were included as a control group. In addition, the demographic and clinical characteristics of the deceased donors and the duration of cryopreservation were obtained from the Korean Network for Organ Sharing (KONOS). Potential risk factors, clinical characteristics, and treatment outcomes had been recorded prospectively in an Excel database (Microsoft Corp., Redmond, WA, USA) and were analyzed retrospectively as part of this study.
Procurement of vascular tissues from deceased donors and cryopreservation techniques
This study employed human arterial tissues from deceased multi-organ donors. All procedures for vascular tissue procurement and processing were in compliance with Korean legislation (Law 5858/1999 and Law 11976/2013) and conformed to the ethical and safety concerns for therapeutic use.
The aorto-iliac arterial allograft was obtained aseptically from each anonymized donor diagnosed with brain death during the course of multi-organ procurement. The aorto-iliac arterial allograft was washed with saline solution and stored at 4°C. For cryopreservation, washed arterial allografts were immersed in cryopreservation solution, consisting of 90% culture medium (RPMI 1640) and 10% dimethylsulfoxide (DMSO) in a cryostorage bag (Medi-Rution, Gyeonggi-do, Korea) at 20°C (8). The bag was sealed in a laminar flow cabinet. Programmed cryopreservation was performed in a Controlled Rate Freezing System (Model 14S-B®, SY-LAB Geräte GmbH, Neupurkersdorf, Austria), as described (9). The protocol consisted of a slow, programmed cooling at a mean rate of 1°C/min, to −70°C. The bag was immediately transferred to the gas phase of a liquid nitrogen compartment, followed by rapid cooling to −196°C. The defrost protocol was a two-stage rewarming process (9), consisting of slow warming by transferring the bag from the nitrogen gas phase to room temperature (20°C) over 30 minutes, followed by rapid warming by immersing the bag in a water bath at 40°C until the contents were completely defrosted. The cryoprotectant liquid was gradually removed in four 3-minute steps by immersion in tapering concentrations of DMSO (10%, 5%, 0%, and 0%) at 4°C.
Surgical technique
Before surgery, all patients provided written informed consent. Selected patients underwent preoperative duplex scanning or venography. In the allograft group, all operations were performed at the site of the previously placed vascular access under local anesthesia. Upper arm hemodialysis vascular access grafts required exposure of the axillary vein and brachial artery in the axilla and antecubital fossa, respectively. In the prosthetic graft group, the tapered 4- to 6-mm expanded polytetrafluoroethylene (PTFE) prosthetic graft, tunneled subcutaneously in a straight configuration, was anastomosed to the vein and artery end-to-side using 6-0 Prolene. In the allograft group, the cryopreserved aorto-iliac arterial allograft was thawed (9). To adequately modify the diameter and length of the cryopreserved arterial allograft, the common and/or external iliac arterial segments were isolated and tributaries were ligated. To lengthen the vascular conduit, both arterial segments were anastomosed continuously with each other end-to-end using 6-0 Prolene. The cryopreserved arterial allograft, tunneled subcutaneously in a straight configuration, was anastomosed to the vein and artery end-to-side using 6-0 Prolene. Duplex investigation and surveillance were performed only when dialysis was poor.
Definitions and statistical analyses
A successful hemodialysis was defined as a graft that had used successfully for at least three dialysis sessions. These patients were prospectively evaluated from the time of access placement until cumulative access failure to determine: 1) duration of catheter dependence from access placement to successful cannulation of the vascular access, 2) primary (unassisted) access survival, 3) cumulative (assisted) access survival, and 4) total number of interventions during the life of the access (10). Primary access failure was defined as an access never usable for dialysis. The duration of catheter dependence was calculated as the time interval from upper arm access placement to removal of the tunneled central catheter after successful cannulation of the access. Primary (unassisted) access survival was calculated from the access placement to the first intervention required to maintain its patency for dialysis. Cumulative (assisted) access survival was calculated from the access placement to permanent failure, regardless of the number of interventions for the maintenance of its patency.
The patients' demographic and clinical characteristics were analyzed using the Mann-Whitney U test, Pearson's χ2 test, or Fisher's exact test, as appropriate. Primary (unassisted) and cumulative (assisted) access survivals, stratified by graft materials (prosthetic graft or cryopreserved iliac arterial allograft), were plotted using the Kaplan-Meier method, with patient follow-up censored for death, renal transplant, or transfer to a nonparticipating dialysis unit. Access survival in the two groups was compared using the log-rank test. All statistical analyses were performed using SPSS software (version 18.0; SPSS, Chicago, IL, USA), with P values ≤ 0.05 considered statistically significant.
Ethics statement
The study protocol was approved by the institutional review board of Asan Medical Center (IRB No.: 2012-0557). Informed consent was confirmed by the board.
RESULTS
Patient population
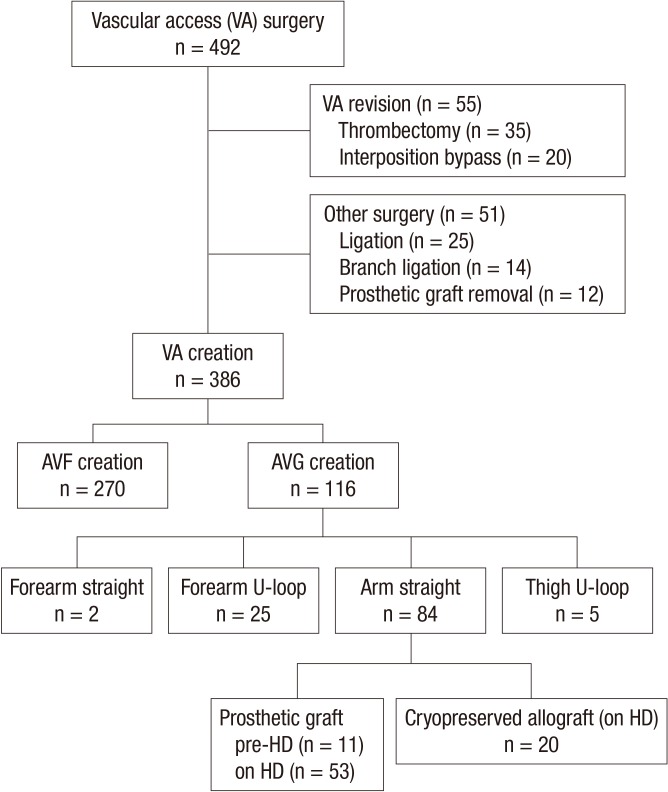
Of the 386 hemodialysis patients who underwent vascular access placement, 20 (5.2%) received an upper arm vascular access of a cryopreserved iliac arterial allograft (allograft group) and 53 (13.7%) underwent upper arm vascular access using an expanded PTFE prosthetic graft (prosthetic graft group) (Fig. 1).
Fig. 1.
Flow chart of patient inclusion. AVF, arteriovenous fistula; AVG, arteriovenous graft; HD, hemodialysis; pre-HD, access placement before initiation of hemodialysis; on HD, access placement after initiation of hemodialysis.
Demographic and clinical characteristics
Table 1 summarizes the demographic and clinical characteristics of these two patient groups. The percentage of males was significantly higher in the prosthetic graft than in the allograft group (P = 0.001). However, age and other atherosclerosis risk factors were similar in the two groups. Primary access failure did not occur in either group. In the allograft group, the causes of a failed or failing previous vascular access included venous stenosis followed by thrombosis in ten patients (50.0%), diffuse aneurysmal dilation with thrombosis in six (30.0%), and gross vascular access graft infection in four (20.0%). The mean baseline diameters of the vascular conduit on the arterial (6.2 ± 0.7 mm, P < 0.001) and venous (7.1 ± 1.6 mm, P < 0.001) sides in the allograft group were significantly greater than those in the prosthetic graft group, with all of the latter receiving vascular access using tapered 4- to 6-mm prosthetic grafts.
Table 1. Baseline characteristics of the study population.
| Parameters | Total | Prosthetic graft | Arterial allograft* | P value |
|---|---|---|---|---|
| No. of patients | 73 | 53 | 20 | |
| Mean age, yr | 67.8 ± 11.7 | 68.9 ± 12.1 | 65.1 ± 10.7 | 0.119 |
| Male sex | 57 (78.1) | 47 (88.7) | 10 (50.0) | 0.001 |
| BMI, kg/m2 | 22.3 ± 3.2 | 22.4 ± 3.3 | 21.9 ± 2.9 | 0.634 |
| Risk factors | ||||
| DM | 45 (61.6) | 32 (60.4) | 13 (65.0) | 0.717 |
| Hypertension | 62 (84.9) | 46 (86.8) | 16 (80.0) | 0.479 |
| Smoking | 4 (5.5) | 3 (5.7) | 1 (5.0) | 1.000 |
| Hyperlipidemia† | 143.5 ± 37.1 | 145.0 ± 36.0 | 139.4 ± 40.6 | 0.404 |
| CAD | 13 (17.8) | 10 (18.9) | 3 (15.0) | 1.000 |
| Diameter of vascular conduit, mm | ||||
| Artery side | 4.6 ± 1.0 | 4.0 ± 0.0 | 6.2 ± 0.7 | < 0.001 |
| Vein side | 6.3 ± 0.9 | 6.0 ± 0.0 | 7.1 ± 1.6 | < 0.001 |
| Clinical factors | ||||
| CV catheter‡ | 7 (9.6) | 6 (11.3) | 1 (5.0) | 0.665 |
| Time to use, day§ | 26.1 ± 17.0 | 34.4 ± 11.39 | 4.9 ± 8.5 | < 0.001 |
| Intervention∥ | 1.1 ± 1.2 | 1.1 ± 1.2 | 1.1 ± 1.3 | 0.735 |
| Antiplatelet use | 36 (49.3) | 26 (49.1) | 10 (50.0) | 0.943 |
| Follow-up, mon | 18.6 ± 8.6 | 18.4 ± 8.8 | 18.8 ± 8.3 | 0.862 |
Continuous data are expressed as mean ± SD, and categorical data as numbers (%).
BMI, body mass index; DM, diabetes mellitus; CAD, coronary artery disease; CV catheter, ipsilateral central venous catheter.
*Cryopreserved iliac arterial allograft from deceased donor; †Total cholesterol level > 200 mg/Dl;
‡Use of an ipsilateral central venous catheter for hemodialysis at the time of access placement; §Mean duration of catheter dependence until successful cannulation of the upper arm access; ‖Total rate of interventions for the life of the access.
At the time of access placement, there was no definite stenosis or occlusion of the central vein and use of an ipsilateral central venous catheter for hemodialysis did not differ in the two groups (P = 0.665) (Table 1). The mean duration of catheter dependence was significantly longer in the prosthetic graft than in the allograft group (34.4 ± 11.39 days vs. 4.9 ± 8.5 days, P < 0.001). In the allograft group, use of vascular access started within 7 days in 16 patients (80.0%), as soon as from the day of surgery in 10 patients, versus none within 7 days in the prosthetic graft group. The mean duration of patient follow-up in these two groups was similar (18.4 ± 8.8 months vs. 18.8 ± 8.3 months, P = 0.862). Table 2 summarizes the demographic and clinical characteristics, as well as the causes of brain death, of the multi-organ deceased donors in this study.
Table 2. Baseline characteristics of the deceased donors.
| Parameters | No. (%) of deceased donors (n = 20) |
|---|---|
| Mean age, yr | 39.6 ± 11.4 |
| Male sex | 12 (60.0) |
| BMI, kg/m2 | 23.2 ± 3.8 |
| Risk factors | |
| DM | 1 (5.0) |
| Hypertension | 3 (15.0) |
| Causes of brain death | |
| Multiple trauma | 13 (65.0) |
| ICH | 4 (20.0) |
| Hypoxic damage | 3 (15.0) |
| Duration of cryopreservation, day* | 197.8 ± 212.7 |
Continuous data are expressed as mean ± SD, and categorical data as numbers (%).
BMI, body mass index; DM, diabetes mellitus; ICH, spontaneous intracerebral hemorrhage.
*Duration from arterial procurement to use as a vascular conduit
Pathologic findings of the allograft and matured vein
Histologic evaluation of the allograft from a malfunctioned upper arm vascular access using a cryopreserved arterial allograft revealed fibrous intimal thickening with myxoid degeneration, fragmentation and calcification of internal elastic lamella, and widening of interlamellar spaces. The media showed degenerative changes such as fibrosis, hyalinization, extracellular deposition of mucoid materials and extensive thinning, fragmentation and loss of elastic fibers. Infiltration of inflammatory cells into adventitia was rarely seen (Fig. 2A and B). These findings were similar to the matured vein from a malfunctioned autogenous AVF that revealed extensive fibrous intimal thickening with myxoid degeneration and degenerative changes of the media including fibrosis, hyalinization and calcification (Fig. 2C).
Fig. 2.
Pathologic findings of the allograft and matured vein. (A) Histologic evaluation of the allograft from a malfunctioned upper arm vascular access shows fibrosis and hyalinization of media and fibrous intimal thickening (H & E, × 100). (B) Elastic staining of the allograft reveals fragmentation of internal elastic lamella, widening of interlamellar spaces and extensive loss of elastic framework in media (Elastic van Gieson, × 100). (C) Histologic evaluation of the matured vein from a malfunctioned autogenous arteriovenous fistula shows extensive fibrous intimal thickening with myxoid degeneration and luminal occlusion (H & E, × 40).
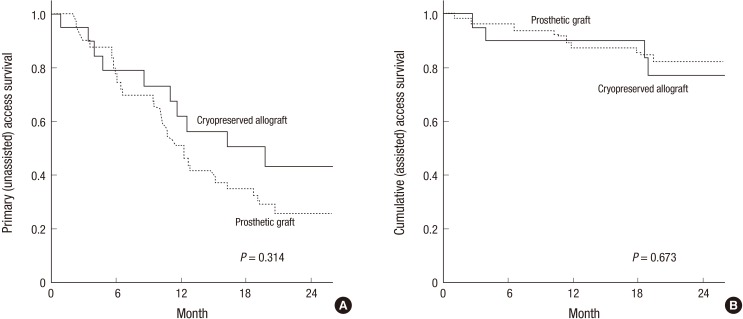
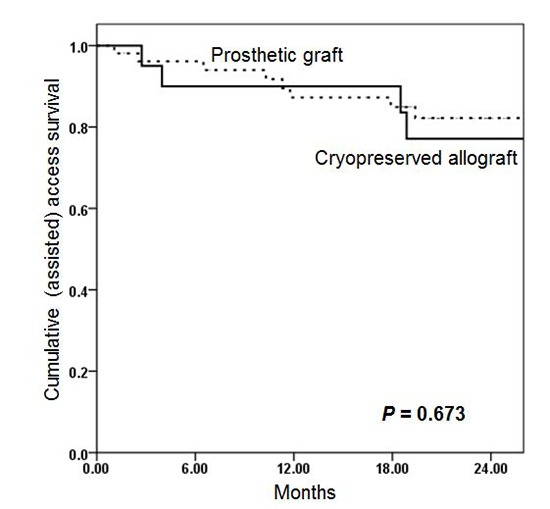
Kaplan-Meier estimates of primary and cumulative access survivals
Kaplan-Meier analysis showed that primary (unassisted, P = 0.314) and cumulative (assisted, P = 0.673) access survivals were similar in the two groups (Fig. 3). The total rate of interventions (from its creation to permanent failure) was similar in the prosthetic graft and allograft groups (1.1 ± 1.2 times vs. 1.1 ± 1.3 times, P = 0.735). In the allograft group, absolute treatment effect, hazard ratio, and P-value for primary (unassisted) access survival and cumulative (assisted) access survival could not be calculated because of the small number of patients, resulting in unreliable estimates. There were no postoperative complications, such as steal phenomenon, related to the use of a cryopreserved iliac arterial allograft except for one patient who experienced wound hematoma. In the four patients with recent gross vascular access graft infection, none experienced recurrent infection after placement of vascular access using a cryopreserved arterial allograft.
Fig. 3.
Kaplan-Meier estimates of primary and cumulative access survivals. (A) Primary (unassisted) and (B) cumulative (assisted) access survival of upper arm vascular accesses using cryopreserved iliac arterial allografts and prosthetic grafts.
DISCUSSION
Successful hemodialysis procedures for ESRD patients receiving chronic renal replacement therapy require functional vascular access (5). However, studies have reported rates of primary nonfunction or failure to mature as high as 50%, and the maturation process of a new AVF is time-consuming. Although relatively easy to place and ready to use, AVGs have a substantial complication rate. Implantation of a prosthetic graft also requires healing process for optimal hemodialysis. Hence, salvaging a failed or failing vascular access to prolong its patency is as important as its initial creation (1). However, use of a central venous catheter is unavoidable in chronic hemodialysis patients with non-salvageable, failed or failing vascular access. Compared with vascular access for hemodialysis, central venous catheters have been associated with reduced blood flow, increased rates of local and systemic infections, development of central venous stenosis and thrombosis, and increased morbidity and mortality rates (11). Therefore, use of a central venous catheter for hemodialysis should be avoided if possible, except as a temporary measure or for patients with short life expectancy (5).
Arterial allografts were the first widely used vessel grafts (12), but are no longer used clinically because their chronic rejection can result in arterial wall dilation and rupture, making them unsuitable for long-term arterial replacement in vascular surgery (13). This rejection process induces intense remodeling of the arterial wall, with medial destruction being the main consequence of chronic rejection in arterial allografts. Arterial walls become unable to counter the force exerted by the blood. This can result in thinning of the media, dislocation of the elastic lamellae, progressive destruction of smooth muscle cells, and infiltration of inflammatory cells into the adventitia (13). Therefore, medial cell loss, matrix degeneration, and adventitial inflammation indicate immune injury and response in arterial allografts (13).
Two strategies have been adopted to reduce these arterial changes during rejection: reducing the immunologic response of the host and reducing allograft antigenicity, mainly by tanning (13). Although animal experiments suggest that a low-maintenance dose of cyclosporine prevents aneurysmal changes in arterial allografts, cyclosporine can also induce potentially serious adverse effects in elderly and critically ill patients (14). Cryopreservation can reduce allograft antigenicity by decellularization, but the optimal cryopreservation methods have not yet been determined (13,14). Allograft decellularization results in the qualitative and quantitative preservation of the medial elastin network, as well as suppressing adventitial inflammatory cell infiltration into allografts (13,14,15,16,17). In this study, although histologic evaluation showed significant degenerative changes in the cryopreserved arterial allograft, these findings were comparable to those of the matured vein and there were also similar clinical outcomes compared with the prosthetic graft. For the determination of the optimal cryopreservation method and histologic changes of the cryopreserved arterial allograft, further studies on larger cohorts are warranted.
Several limitations should be noted. First, it was performed at a single center, and there was not adjustment for baseline differences between the two groups. The choice to use a cryopreserved arterial allograft and the timing to first use a vascular access were decided without randomization by the vascular surgeon and the nephrologist, respectively. Furthermore, the mean diameters of the vascular conduit on the arterial and venous sides in the allograft group were significantly greater than those in the prosthetic graft group; the use of a larger vascular conduit may impair optimal performance of the vascular access because of the diverging size discrepancy between native vessels and the conduit. However, we could not obtain a smaller arterial allograft, such as femoral or popliteal arterial allograft, from the deceased donors. Second, the number of patients in the allograft group was relatively small, not allowing evaluation of absolute treatment effect, hazard ratio, and P-values for primary (unassisted) and cumulative (assisted) access survival. Third, because the immediately usable PTFE graft (a polyetherurethaneurea vascular access prosthetic graft) is not available in Korea (18), we could not compare our results with this type of PTFE graft. Moreover, we could not compare costs in the two groups because the costs of cryopreserved arterial allograft have not yet been determined in our institution. We did not consider ABO blood type compatibility in the inclusion criteria because of our study design. Although there has been controversy over the impact of ABO blood type compatibility, some authors reported that use of the cryopreserved allograft with donor-recipient ABO compatibility for peripheral arterial bypass had significantly better patency rate (19,20). We did not evaluate whether the cryopreserved arterial allograft affected the prognosis of future renal transplantation. It is known that the use of cryopreserved cadaveric vascular allografts for vascular access leads to broad allosensitization as measured by panel reactive antibody assay; cryopreserved cadaveric vascular allografts should not be used for vascular access in potential renal transplant recipients (7). Although cryopreserved arterial allografts could be more resistant to infection than prosthetic grafts, we could not recommend their routine use for vascular access in all patients undergoing dialysis because they may be considerably more expensive than prosthetic grafts according to other studies (17) and access survival was not significantly superior to that of an access using a prosthetic graft in this study.
In conclusion, use of a cryopreserved arterial allograft may allow immediate hemodialysis without the use of a central venous catheter in patients with a failed or failing vascular access, with access survival not inferior to that of an upper arm vascular access using a prosthetic graft. Cryopreserved arterial allografts may be a safe temporizing measure to help eradicate infection in certain clinical circumstances, such as in an infected graft environment, and could permit subsequent use of a prosthetic graft if necessary.
Footnotes
Funding: This study was supported by a grant (grant number 2012-0557) from the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea.
DISCLOSURE: No potential conflicts of interest relevant to this article were reported.
AUTHOR CONTRIBUTION: Conception and design: Ha TY, Kim YH, Chang JW, Cho YP. Acquisition of data: Ha TY, Kim YH, Chang JW, Han Y, Kwon H, Kwon TW, Cho YP. Analysis and interpretation of data: Ha TY, Kim YH, Chang JW, Park Y, Han DJ, Cho YP, Lee SG. Writing or revision of the manuscript: Ha TY, Kim YH, Chang JW, Park Y, Cho YP. Final approval: all authors.
References
- 1.Caroli A, Manini S, Antiga L, Passera K, Ene-Iordache B, Rota S, Remuzzi G, Bode A, Leermakers J, van de Vosse FN, et al. Validation of a patient-specific hemodynamic computational model for surgical planning of vascular access in hemodialysis patients. Kidney Int. 2013;84:1237–1245. doi: 10.1038/ki.2013.188. [DOI] [PubMed] [Google Scholar]
- 2.Sidawy AN, Spergel LM, Besarab A, Allon M, Jennings WC, Padberg FT, Jr, Murad MH, Montori VM, O'Hare AM, Calligaro KD, et al. The Society for Vascular Surgery: clinical practice guidelines for the surgical placement and maintenance of arteriovenous hemodialysis access. J Vasc Surg. 2008;48:2S–25S. doi: 10.1016/j.jvs.2008.08.042. [DOI] [PubMed] [Google Scholar]
- 3.Long B, Brichart N, Lermusiaux P, Turmel-Rodrigues L, Artru B, Boutin JM, Pengloan J, Bertrand P, Bruyère F. Management of perianastomotic stenosis of direct wrist autogenous radial-cephalic arteriovenous accesses for dialysis. J Vasc Surg. 2011;53:108–114. doi: 10.1016/j.jvs.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Rooijens PP, Tordoir JH, Stijnen T, Burgmans JP. Smet de AA, Yo TI. Radiocephalic wrist arteriovenous fistula for hemodialysis: meta-analysis indicates a high primary failure rate. Eur J Vasc Endovasc Surg. 2004;28:583–589. doi: 10.1016/j.ejvs.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Roy-Chaudhury P, Sukhatme VP, Cheung AK. Hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. J Am Soc Nephrol. 2006;17:1112–1127. doi: 10.1681/ASN.2005050615. [DOI] [PubMed] [Google Scholar]
- 6.Clark EG, Barsuk JH. Temporary hemodialysis catheters: recent advances. Kidney Int. 2014;86:888–895. doi: 10.1038/ki.2014.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benedetto B, Lipkowitz G, Madden R, Kurbanov A, Hull D, Miller M, Bow L. Use of cryopreserved cadaveric vein allograft for hemodialysis access precludes kidney transplantation because of allosensitization. J Vasc Surg. 2001;34:139–142. doi: 10.1067/mva.2001.114206. [DOI] [PubMed] [Google Scholar]
- 8.Kim HO, Kim J, Jin HL. Evaluation of domestic cryostorage blood bags. Korean J Blood Transfus. 2006;17:48–53. [Google Scholar]
- 9.Pegg DE, Wusteman MC, Boylan S. Fractures in cryopreserved elastic arteries. Cryobiology. 1997;34:183–192. doi: 10.1006/cryo.1996.1997. [DOI] [PubMed] [Google Scholar]
- 10.Lee T, Barker J, Allon M. Comparison of survival of upper arm arteriovenous fistulas and grafts after failed forearm fistula. J Am Soc Nephrol. 2007;18:1936–1941. doi: 10.1681/ASN.2006101119. [DOI] [PubMed] [Google Scholar]
- 11.Asif A, Cherla G, Merrill D, Cipleu CD, Briones P, Pennell P. Conversion of tunneled hemodialysis catheter-consigned patients to arteriovenous fistula. Kidney Int. 2005;67:2399–2406. doi: 10.1111/j.1523-1755.2005.00347.x. [DOI] [PubMed] [Google Scholar]
- 12.Szilagyi DE, McDonald RT, Smith RF, Whitcomb JG, Whitcomb JG. Biologic fate of human arterial homografts. AMA Arch Surg. 1957;75:506–527. doi: 10.1001/archsurg.1957.01280160016003. [DOI] [PubMed] [Google Scholar]
- 13.Allaire E, Guettier C, Bruneval P, Plissonnier D, Michel JB. Cell-free arterial grafts: morphologic characteristics of aortic isografts, allografts, and xenografts in rats. J Vasc Surg. 1994;19:446–456. doi: 10.1016/s0741-5214(94)70071-0. [DOI] [PubMed] [Google Scholar]
- 14.Schmitz-Rixen T, Megerman J, Colvin RB, Williams AM, Abbott WM. Immunosuppressive treatment of aortic allografts. J Vasc Surg. 1988;7:82–92. [PubMed] [Google Scholar]
- 15.Bia D, Pessana F, Armentano R, Pérez H, Graf S, Zócalo Y, Saldías M, Perez N, Alvarez O, Silva W, et al. Cryopreservation procedure does not modify human carotid homografts mechanical properties: an isobaric and dynamic analysis. Cell Tissue Bank. 2006;7:183–194. doi: 10.1007/s10561-005-0655-0. [DOI] [PubMed] [Google Scholar]
- 16.Kieffer E, Gomes D, Chiche L, Fléron MH, Koskas F, Bahnini A. Allograft replacement for infrarenal aortic graft infection: early and late results in 179 patients. J Vasc Surg. 2004;39:1009–1017. doi: 10.1016/j.jvs.2003.12.040. [DOI] [PubMed] [Google Scholar]
- 17.Madden RL, Lipkowitz GS, Browne BJ, Kurbanov A. A comparison of cryopreserved vein allografts and prosthetic grafts for hemodialysis access. Ann Vasc Surg. 2005;19:686–691. doi: 10.1007/s10016-005-6621-2. [DOI] [PubMed] [Google Scholar]
- 18.Kakkos SK, Andrzejewski T, Haddad JA, Haddad GK, Reddy DJ, Nypaver TJ, Scully MM, Schmid DL. Equivalent secondary patency rates of upper extremity Vectra Vascular Access Grafts and transposed brachial-basilic fistulas with aggressive access surveillance and endovascular treatment. J Vasc Surg. 2008;47:407–414. doi: 10.1016/j.jvs.2007.09.061. [DOI] [PubMed] [Google Scholar]
- 19.Walker PJ, Mitchell RS, McFadden PM, James DR, Mehigan JT. Early experience with cryopreserved saphenous vein allografts as a conduit for complex limb-salvage procedures. J Vasc Surg. 1993;18:561–569. [PubMed] [Google Scholar]
- 20.Zehr BP, Niblick CJ, Downey H, Ladowski JS. Limb salvage with CryoVein cadaver saphenous vein allografts used for peripheral arterial bypass: role of blood compatibility. Ann Vasc Surg. 2011;25:177–181. doi: 10.1016/j.avsg.2010.07.020. [DOI] [PubMed] [Google Scholar]