Abstract
AIM
To examine possible differences in clinical outcomes between sub-threshold micro-pulse diode laser photocoagulation (SDM) and traditional modified Early Treatment Diabetic Retinopathy Study (mETDRS) treatment protocol in diabetic macular edema (DME).
METHODS
A comprehensive literature search using the Cochrane Collaboration methodology to identify RCTs comparing SDM with mETDRS for DME. The participants were type I or type II diabetes mellitus with clinically significant macular edema treated by SDM from previously reported randomized controlled trials (RCTs). The primary outcome measures were the changes in the best corrected visual acuity (BCVA) and the central macular thickness (CMT) as measured by optical coherence tomography (OCT). The secondary outcomes were the contrast sensitivity and the damages of the retina.
RESULTS
Seven studies were identified and analyzed for comparing SDM (215 eyes) with mETDRS (210 eyes) for DME. There were no statistical differences in the BCVA after treatment between the SDM and mETDRS based on the follow-up: 3mo (MD, -0.02; 95% CI, -0.12 to 0.09; P=0.77), 6mo (MD, -0.02; 95% CI, -0.12 to 0.09; P=0.75), 12mo (MD, -0.05; 95% CI, -0.17 to 0.07; P=0.40). Likewise, there were no statistical differences in the CMT after treatment between the SDM and mETDRS in 3mo (MD, -9.92; 95% CI, -28.69 to 8.85; P=0.30), 6mo (MD, -11.37; 95% CI, -29.65 to 6.91; P=0.22), 12mo (MD, 8.44; 95% CI, -29.89 to 46.77; P=0.67). Three RCTs suggested that SDM laser results in good preservation of contrast sensitivity as mETDRS, in two different follow-up evaluations: 3mo (MD, 0.05; 95% CI, 0 to 0.09; P=0.04) and 6mo (MD, 0.02; 95% CI, -0.10 to 0.14; P=0.78). Two RCTs showed that the SDM laser treatment did less retinal damage than that mETDRS did (OR, 0.05; 95% CI, 0.02 to 0.13; P<0.01).
CONCLUSION
SDM laser photocoagulation shows an equally good effect on visual acuity, contrast sensitivity, and reduction of DME as compared to conventional mETDRS protocol with less retinal damage.
Keywords: sub-threshold, laser photocoagulation, diabetic macular edema
INTRODUCTION
Diabetic macular edema (DME) is the most common cause of vision loss in patients with diabetes mellitus[1]. The management of this disease has substantially changed due to the advancement in pharmacotherapy with intravitreal injections of corticosteroids and injections of anti-vascular endothelial growth factor (VEGF) in recent years[2]–[3]. However, the traditional laser treatment proposed by the Early Treatment Diabetic Retinopathy Study (ETDRS) is still be widely used for its effectivity, low cost and easy processing[4]–[5].
This conventional modified Early Treatment Diabetic Retinopathy Study (mETDRS) photocoagulation using argon-green (514 nm) or double frequency neodymium YAG (Nd: YAG; 532 nm) laser, with the end point of visible laser spots over the area of thickened retina. It still remains the most effective treatment as reducing the risk of severe visual loss in eyes with DME by 50%[6]. But the laser-induced severe destruction of retinal photoreceptors, progressive enlargement of laser retinal scars even including foveal atrophy, and development of choroidal neovascularization and subfoveal fibrosis still can't be ignored for its therapeutic mechanism[7]–[13]. So, less aggressive laser treatment strategies have been advocated for decade.
The state-of-the-art of sub-threshold micropulse laser treatment (SDM), has been shown to be effective in the treatment of DME in terms of best corrected visual acuity (BCVA), central macular thickness (CMT), and contrast sensitivity (CS)[14]–[17]. The treatment principle is that SDM allows a finer control of the photothermal effects induced at the level of the retinal pigment epithelium (RPE), to perform equally effective laser treatments with only sublethal thermal elevations, avoiding the excessive heat that could cause visible burns, tissue necrosis, and related collateral effects[18]–[22].
Is SDM as effective as conventional mETDRS laser photocoagulation with less retinal damage? More conclusive evidence is required to ascertain the benefits and potential detrimental effects of it. However, differences in selection criteria, study design, allocation protocol, standardization of outcome data, and follow-up have limited the researchers from drawing better conclusions.
To our knowledge, there has been no Meta-analysis of prospective randomized trials comparing the outcomes of SDM versus mETDRS in patients with DME. We performed a Meta-analysis of prospective, randomized, controlled trials studying SDM versus mETDRS for the management of DME. On this basis, the objective of this study is to determine whether SDM is worth being accepted by most of the retina specialists in treating DME when compared with mETDRS.
MATERIALS AND METHODS
This was a Meta-analysis of the existing randomized, controlled clinical trials, so, institutional review board approval was not necessary.
Search Strategy
We searched the Cochrane Central Register of Controlled Trials in The Cochrane Library, MEDLINE, Pubmed, EMBASE related to SDM. The reference lists of every primary article and previous systematic review were scrutinized for information about additional trials. We performed the final search on Jun 6, 2015. This study adhered to the tenets of the Declaration of Helsinki. No language restrictions were used in the electronic searches for trials. The following search strategy was used: INDEX TERMS (diabetic retinopathy OR diabetic retinopathies); OR TITLE-ABS-KEY (diabetic retinopathy); INDEX TERMS (macular edema OR cystoid macular edema); OR TITLE-ABS-KEY (macular edema OR macular oedema); TITLE-ABS-KEY (light coagulation OR photocoagulation*); INDEX TERMS light coagulation; TITLE-ABS-KEY (random* OR prospective study OR prospective studies OR randomized controlled trial*).
Inclusion Criteria
Only randomized controlled trials (RCTs) evaluating SDM and conventional mETDRS treatment in DME were included in this study. Non proliferative diabetic retinopathy (NPDR) patients with macular edema were included, with no restrictions on participant sex or ethnicity.
Exclusion Criteria
SDM protocol defines as using low duty cycle and long “off time” between pulses within the exposure envelope, with a long wavelength (810 nm-infrared wavelength). It does not include monopulse laser or retinal regeneration therapy[23]. It does not include long-pulse subthreshold transpupillary thermotherapy (TTT) neither[24]. Patients with proliferative retinopathy, significant media opacities precluding fundus evaluation and laser therapy, prior medical treatment (intravitreal/peribulbar steroids or anti-angiogenic drugs), prior laser treatment, macular pathology other than diabetic maculopathy, and ocular surgery within 6mo prior to screening were excluded. Patients with uncontrolled hypertension and renal failure requiring dialysis were also excluded from the study. Pediatric patients with the age ≤18y were excluded from the study.
Quality Assessment of Retrieved Articles
Two authors (Qiao G and Dai Y ) independently assessed all titles found by electronic and manual searches. The studies selected in the analysis were reviewed for risk of bias based on the methods recommended in the Cochrane Handbook for Systemic Reviews of Interventions. Studies included were assessed for methodological quality. Jadad scores on a scale of 0 to 5 were used to evaluate the quality of each trial. Each trial was assessed for 3 main aspects of its study design: randomization, masking, and participant withdrawals/dropouts. Trials with a score higher than 3 were considered being of high quality.
Outcome Measures
The primary outcome measures are changes in the BCVA and the CMT as measured by optical coherence tomography (OCT) 3, 6, and 12mo after laser therapy. The secondary outcomes are the CS and retinal damage (laser scars).
Data Extraction and Transform
Two independent reviewers (Chen XH and Chen ZL) extracted data from the included trials using a customized form. Follow-up times after the procedures were unitized in 3, 6 and 12mo. Figueira et al[25] afforded follow-up time of 4 and 12mo were approximated and included as 3 and 12mo. In the same way, Kumar et al[26] afforded follow-up time of 12 and 18wk were approximated and included as 3 and 6mo. The BCVA was unitized using the expression in ETDRS logMAR. The decimal visual acuity and ETDRS numbers of letters were converted to ETDRS logMAR. CS was unitized in log units. Figueira et al[25] afforded CS letters were converted to log units. In Lavinsky et al[27], only normal density data in SDM group was included in this study.
Statistical Analysis
The quantitative data were entered into Cochrane Review Manager (RevMan, software version 5.2.11, Copenhagen, Denmark: The Nordic Cochrane Center, The Cochrane Collaboration, 2014). Meta analysis was performed on the primary and secondary outcome measures. Summary estimates, including 95% confidence intervals (CIs), were calculated. For continuous outcomes data (e.g. BCVA, CMT), the means and standard deviations were used to calculate the estimated mean difference (MD) between groups. For dichotomous outcomes (e.g. number of eyes), the odds ratio (OR) was calculated. For analysis, a fixed-effects model was used for ≤3 studies and a random effects model was used for >3 studies. Statistical heterogeneity was tested using the Chi-square test and I2 statistics.
RESULTS
Search Results
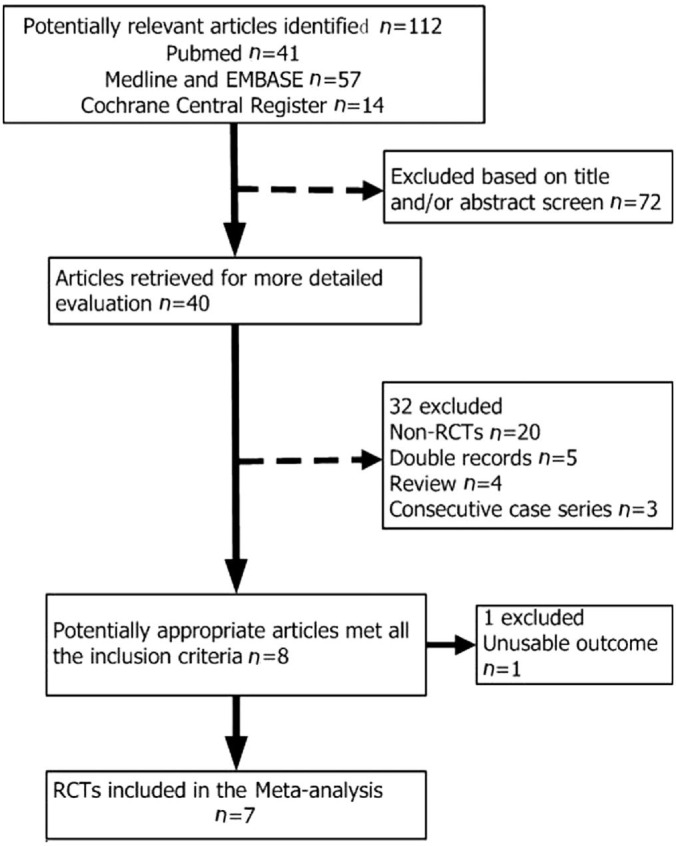
Our search strategy identified a total of 112 articles from electronic searches of PubMed, MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials. The flow chart of studies from the initial data to final included data is shown in Figure 1. Eight studies potentially met all of the predefined inclusion criteria but 7 randomized controlled trials published between 2004 and 2013 were included in this Meta-analysis finally for 1 study (Grigorian RA 2004)[18] afford unusable outcome.
Figure 1. Flow diagram of the literature search for studies on SDM vs mETDRS for DME.
RCTs: Randomized controlled trials.
Publication Bias
Publication bias was explored by searching for asymmetry in the funnel plot.
Baseline Characteristics
A total of 379 participants with 467 eyes in the 7 included trials published from 8 countries from 2004 to 2013 were enrolled in this Meta-analysis. Two hundred and fifteen eyes were treated using SDM and 210 eyes were treated using ETDRS protocol with green laser. The main characteristics and quality scores of the included trials were shown in Table 1. The mean age of patients ranged from 49.8 to 62.8y. Three of the 7 trials got random number from random number table, the others were unclear. Three trials referred to double blind and the methods were appropriate. One trial lost 6 eyes (6/123) to follow-up, 1 trial lost 3 eyes (3/23), 5 trials had 100% completeness of follow-up; 3 trials followed up to 12mo, 3 trials did 6mo, 1 trail did 18wk (4.5mo). One study got 2 points by Jadad scoring scale, 3 studies got 3 points, the other 3 studies got 4 points.
Table 1. Characteristics and quality of included trials evaluating SDM or mETDRS for DME.
| Study1 | Country | FU (mo) | Pts/Eyes (n) |
x±s (a, range) |
Allocation concealme | Masking of Pts | Masking of outcome assessor | Loss to FU (eyes) | Quality score | |
| SDM | mETDRS | |||||||||
| Laursen 2004[38] | Denmark | 6 | 16/23 | 61.0 (13) (39-89) | 61.0 (13) (39-89) | Y | NA | NA | 3 | 2 |
| Figueira 2009[25] | Portugal/England | 12 | 53/84 | 59.8±9.9 | 61.1±9.9 | Y | NA | NA | 0 | 3 |
| Kumar 2010[26] | India | 24.5 | 20/30 | 50.93±6.6 | 49.8±6.2 | Y | Y | NA | 0 | 4 |
| Vujosevic 2010[37] | Italy | 12 | 50/62 | 62.8±10.1 (31-81) | 62.1±9.4 (45-77) | Y | NA | NA | 0 | 3 |
| Lavinsky 2011[27] | Brazil | 12 | 123/123 | 362.0±7.4 | 61.8 (7.0) | Y | Y | Y | 6 | 4 |
| Venkatesh 2011[36] | India | 6 | 33/46 | NA | NA | Y | NA | NA | 0 | 3 |
| Xie 2013[35] | China | 6 | 84/99 | 58±9.3 | 56±5.9 | Y | Y | Y | 0 | 4 |
FU: Follow-up; Y: Yes; NA: Not available; Pts: Patients. 1First author and year; 212wk; 3Normal density of SDM group.
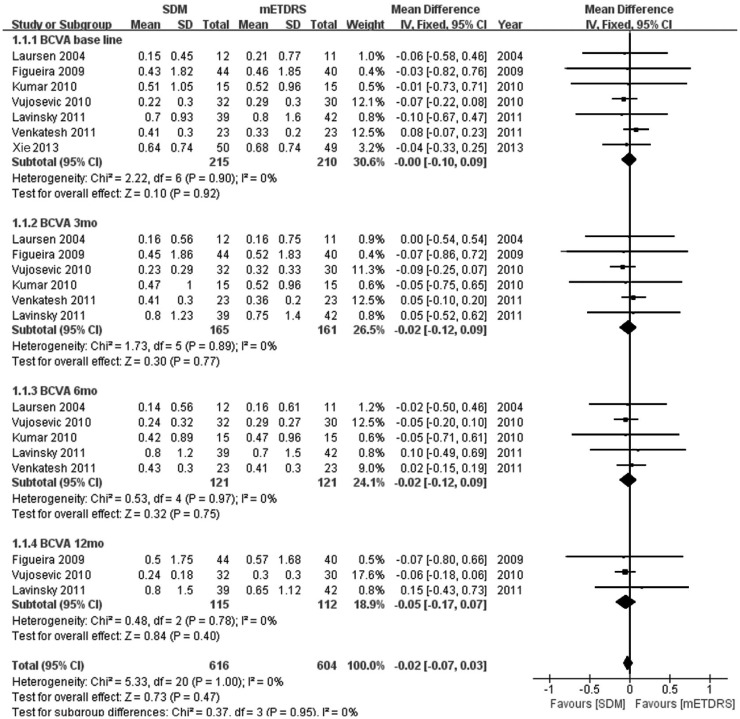
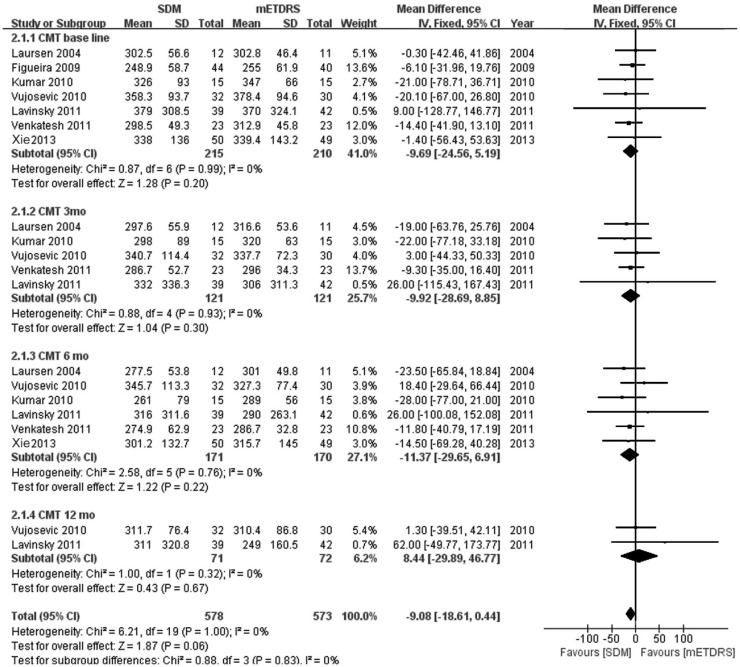
There was no statistical difference in the BCVA before treatment between the SDM and mETDRS groups (MD, 0; 95% CI, -0.1 to 0.09; P=0.92), and no heterogeneity was identified (I2=0%; P=0.90), as shown in Figure 2 (BCVA baseline). Likewise, there was no evidence of a difference in the CMT before treatment between the SDM and ETDRS groups (MD, -9.69; 95% CI, -24.56 to 5.19; P=0.20), and no heterogeneity was identified (I2=0%; P=0.99), as shown in Figure 3 (CMT baseline).
Figure 2. The BCVA after treatment between the SDM and mETDRS groups in different follow-ups.
Figure 3. The CMT after treatment between the SDM and mETDRS groups in different follow-ups.
Outcome Characteristics
Best corrected visual acuity and central macular thickness
Six RCTs include follow-ups to 3mo after therapy, and 5 RCTs include follow-ups to 6mo, and 3 RCTs include follow-ups to 12mo. There was no statistical difference in the BCVA after treatment between the SDM and mETDRS groups in different follow-ups: 3mo (MD, -0.02; 95% CI, -0.12 to 0.09; P=0.77), 6mo (MD, -0.02; 95% CI, -0.12 to 0.09; P=0.75), 12mo (MD, -0.05; 95% CI, -0.17 to 0.07; P=0.40); and no heterogeneity was identified: 3mo (I2=0%; P=0.89), 6mo (I2=0%; P=0.97), 12mo (I2 =0%; P=0.78), as shown in Figure 2 (BCVA 3mo, 6mo, 12mo).
Likewise, there was no difference in the CMT after treatment between the SDM and ETDRS groups in different follow-ups. Five RCTs afforded data of follow-up in 3mo (MD, -9.92; 95% CI, -28.69 to 8.85; P=0.30) and 6 RCTs afforded data of follow-up in 6mo (MD, -11.37; 95% CI, -29.65 to 6.91; P=0.22), 2 RCTs afforded data of follow-up in 12mo (MD, 8.44; 95% CI, -29.89 to 46.77; P=0.67); and no heterogeneity was identified: 3mo (I2=0%; P=0.93), 6mo (I2=0%; P=0.76), 12mo (I2=0%; P=0.32), as shown in Figure 3 (CMT 3mo, 6mo, 12mo).
Contrast sensitivity and laser scars
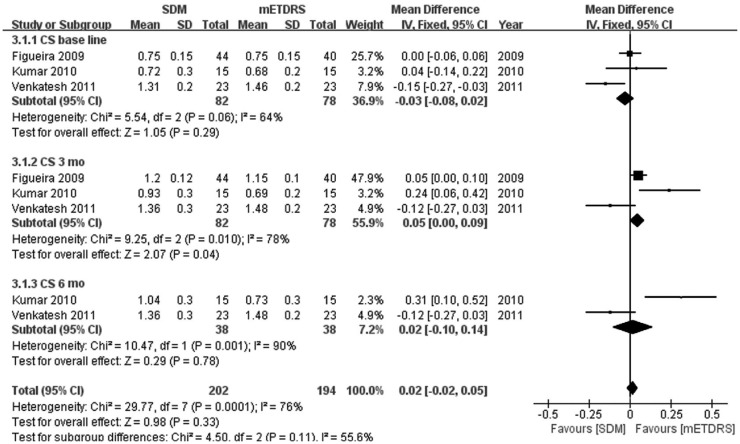
Three RCTs suggested that SDM laser results in good preservation of CS as compared to mETDRS: 3mo (MD, 0.05; 95% CI, 0 to 0.09; P=0.04), 6mo (MD, 0.02; 95% CI, -0.10 to 0.14; P=0.78), as shown in Figure 4 (CS 3mo, 6mo).
Figure 4. The CS after treatment between the SDM and mETDRS groups in different follow-ups.
Sensitivity analysis using homogeneous trials was performed because of a significant heterogeneity (I2=76%).
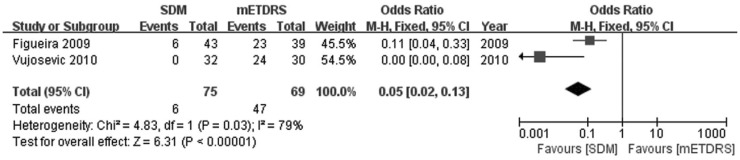
In the studied data, every RCT referred the less damage or laser scars in SDM group but there were only 2 RCTs recorded retinal laser scars in two groups and there were differences in the laser scars after treatment between the SDM and ETDRS groups (OR, 0.05; 95% CI, 0.02 to 0.13; P<0.01), as shown in Figure 5.
Figure 5. The retinal laser scars after treatment between the SDM and mETDRS groups.
Sensitivity analysis using homogeneous trials was performed because of a significant heterogeneity (I2=79%).
There were high heterogeneity in pool data of CS and laser scars since the included RCTs were less than 3. But every RCT showed that SDM laser treatment did not have any change on fundus autofluo-rescence (FAF) and this showed (at least) non-clinically visible damage of the retina.
Publication Bias
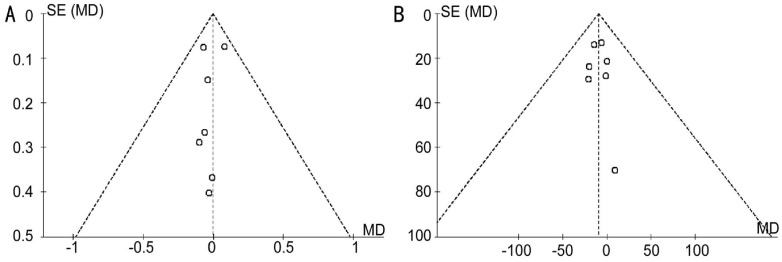
A funnel plot adopted for the primary outcome of BCVA and CMT are shown in Figure 6A and 6B, respectively. Based on a visual analysis of the funnel plot, the approximate symmetry indicates low publication bias.
Figure 6. The funnel plot of the literature search for the studies of SDM vs mETDRS for DME.
A shows the BCVA and B shows the CMT before treatment. Effect estimates of individual studies (MD) are scattered against the precision of the study SE (MD). The approximate symmetry of both funnel plots indicates low publication bias. MD: Mean difference; SE: Standard error.
DISCUSSION
Treatment of DME has always been a challenge. Recently, other treatments for DME have been reported, e.g. pars plana vitrectomy (PPV), pharmacotherapy with intravitreal injections of corticosteroids and injections of anti-vascular endothelial growth factor. But there are some disadvantages to PPV or intravitreal injections, such as severe complications of postoperative rhegmatogenous retinal detachment, infective endophthalmitis, and cataract, or expesive cost[4],[5],[28]–[30]. Conventional mETDRS laser treatment, cited at the beginning of this article, is still the major treatment for DME in most developing country. In order to avoid the major complications from the mETDRS macular laser treatment we have mentioned (such as severe destruction of retinal photoreceptors, enlargement of laser retinal scars, choroidal neovascularization, subfoveal fibrosis, and macular scotomas)[7],[9],[11],[31]–[32], SDM has been proposed as less aggressive treatment strategies. From the first description in 1997 by Friberg and Karatza[33] to the latest report in 2014 by Othman et al[21], SDM photocoagulation has gone through a slow one-decade-long evolution.
Luttrull and Dorin[34] summarized how SDM works without laser-induced retinal damage. SDM is a kind of selective treatment of the RPE. Laser-induced damage is confined to the RPE layer with microsecond-duration pulses and is initially visible on fluorescein angiography (FFA). Therefore there is little or no damage to the photoreceptors and the inner retina theoretically. The micropulse mode treatment aims in delivering laser energy in “micropulses” rather than in a continuous way. Even if at the same laser spot, the duration is the same as the mETDRS (continuous) laser. The micropulse laser uses low duty cycle (the frequency of the train of micropulses) and long “off time” between pulses within the exposure envelope (low repetition rate), therefore produces and maintains less thermal retinal damage and small retinal laser lesions all the time[35]–[38]. Moreover, using a longer wavelength (810 nm-infrared wavelength) in the above mentioned micropulse mode, photothermal laser effects could be applied selectively to the RPE (the source of potent extracellular factors), with less or no thermal retinal damage. Sivaprasad and Dorin[39] had also reviewed the principles, treatment modalities, and clinical outcomes of SDM photocoagulation. The SDM has negligible damage per treatment, and the potential of ongoing PRN treatments, applicable where needed at an affordable cost, rather than where possible (no previous and cumulative burns).
In this research we compared the outcomes of SDM and mETRDS for management of DME from 7 RCTs using Meta-analysis. All data indicate SDM is effective in preserving eyesight and reducing DME after treatment in early, middle and late follow-up. No statistical difference was identified in the BCVA of DME patients between the SDM and mERDS during the follow-ups: 3mo (MD, -0.02; 95% CI, -0.12 to 0.09; P=0.77), 6mo (MD, -0.02; 95% CI, -0.12 to 0.09; P=0.75), and 12mo (MD, -0.05; 95% CI, -0.17 to 0.07; P=0.40). Likewise, there was no statistically significant difference in CMT between the SDM and mERDS in 3mo (MD, -9.92; 95% CI, -28.69 to 8.85; P=0.30), 6mo (MD, -11.37; 95% CI, -29.65 to 6.91; P=0.22), and 12mo (MD, 8.44; 95% CI, -29.89 to 46.77; P=0.67).
This study also indicates that SDM laser photocoagulation showed good preservation of CS as compared to mETDRS, for the follow-ups: 3mo (MD, 0.05; 95% CI, 0 to 0.09; P=0.04), 6mo (MD, 0.02; 95% CI, -0.10 to 0.14 P=0.78). Furthermore, SDM laser showed less or no retinal damage. It is different in the retina damage (laser scars) after treatment between the SDM and mETDRS groups (OR, 0.05; 95% CI, 0.02 to 0.13; P<0.01).
But, before we draw a conclusion that SDM was better than mETDRS for DME therapy, several limitations should be taken into account when considering the results of this Meta-analysis. First, the small numbers of cases per trial (range, 23-123) and in total gave these analyses low power, especially for events with low incidence rates. Nevertheless, this Meta-analysis provided more powerful evidence than the individual reports alone. Second, this Meta-analysis was restricted to data from the published articles, and it was possible that a bias was introduced if the studies had small or reverse effects but were not accepted for publication. Third, 7 RCTs were included for this Meta-analysis, and each trial was included in one or more outcome measures. However, different follow-up time and different data expression of outcome measures made us have to unitize the follow-up and convert data expression, and information lost couldn't be avoided in these procedures. So, long-term RCTs with standardized outcome measures are needed to provide more reliable evidence. Finally, regarding the quality of the evidence, 4/7 of the prospective randomized controlled trials included were subject to performance and detection bias because of their lack of patient and doctor masking; however, attrition bias was relatively low.
Another question should be considered before we draw a conclusion. Why has SDM photocoagulation not yet been adopted by the majority of the retina specialists for decades? Sivaprasad and Dorin[39] thought there were three points hindered the SDM to be widely accepted. First, the evolution of SDM is slow and long. Second, the appropriate laser dosing is still unclear of SDM. Third, new promising intravitreal anti-inflammatory and anti-VEGF pharmacological agents spring up in years, which attracted attentions of retina specialists. As for the appropriate laser dosing, only one RCT (Lavinsky et al[27]) had discussed and suggested low-intensity/high-density treatments can provide statistically significant superior functional performances than mETDRS photocoagulation. So, with the appropriate laser dosing specified, SDM may provide a safe, efficient, affordable and long-term sustainable choice for DME.
Given all these considerations, SDM laser photocoagulation is as good as mETDRS in protection of visual acuity, CS, and reduction of macular edema. Moreover, it is better than mETDRS for little or no retinal damage.
Acknowledgments
Conflicts of Interest: Qiao G, None; Guo HK, None; Dai Y, None; Wang XL, None; Meng QL, None; Li H, None; Chen XH, None; Chen ZL, None.
REFERENCES
- 1.Mitchell P, Wong TY. Diabetic Macular Edema Treatment Guideline Working Group. Management paradigms for diabetic macular edema. Am J Ophthalmol. 2014;157(3):505–513.e1-8. doi: 10.1016/j.ajo.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 2.Boyer DS, Hopkins JJ, Sorof J, Ehrlich JS. Anti-vascular endothelial growth factor therapy for diabetic macular edema. Ther Adv Endocrinol Metab. 2013;4(6):151–169. doi: 10.1177/2042018813512360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arévalo JF, Fernández CF, Mendoza AJ, García RA, Arévalo FA. Intravitreal triamcinolone combined with grid laser photocoagulation for patients with cystoid macular edema and advanced diabetic retinopathy: pilot study. Arch Soc Esp Oftalmol. 2013;88(10):373–379. doi: 10.1016/j.oftal.2013.01.020. [DOI] [PubMed] [Google Scholar]
- 4.Stein JD, Newman-Casey PA, Kim DD, Nwanyanwu KH, Johnson MW, Hutton DW. Cost-effectiveness of various interventions for newly diagnosed diabetic macular edema. Ophthalmology. 2013;120(9):1835–1842. doi: 10.1016/j.ophtha.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar B, Gupta SK, Saxena R, Srivastava S. Current trends in the pharmacotherapy of diabetic retinopathy. J Postgrad Med. 2012;58(2):132–139. doi: 10.4103/0022-3859.97176. [DOI] [PubMed] [Google Scholar]
- 6.Writing Committee for the Diabetic Retinopathy Clinical Research Network. Fong DS, Strauber SF, Aiello LP, Beck RW, Callanan DG, Danis RP, et al. Comparison of the modified Early Treatment Diabetic Retinopathy Study and mild macular grid laser photocoagulation strategies for diabetic macular edema. Arch Ophthalmol. 2007;125(4):469–480. doi: 10.1001/archopht.125.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chew EY, Benson WE, Remaley NA, Lindley AA, Burton TC, Csaky K, Williams GA, Ferris FL., 3rd Results after lens extraction in patients with diabetic retinopathy: early treatment diabetic retinopathy study report number 25. Arch Ophthalmol. 1999;117(12):1600–1606. doi: 10.1001/archopht.117.12.1600. [DOI] [PubMed] [Google Scholar]
- 8.Fong DS, Barton FB, Bresnick GH. Impaired color vision associated with diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report No. 15. Am J Ophthalmol. 1999;128(5):612–617. doi: 10.1016/s0002-9394(99)00227-5. [DOI] [PubMed] [Google Scholar]
- 9.Fong DS, Ferris FL, 3rd, Davis MD, Chew EY. Causes of severe visual loss in the early treatment diabetic retinopathy study: ETDRS report no. 24. Early Treatment Diabetic Retinopathy Study Research Group. Am J Ophthalmol. 1999;127(2):137–141. doi: 10.1016/s0002-9394(98)00309-2. [DOI] [PubMed] [Google Scholar]
- 10.Davis MD, Fisher MR, Gangnon RE, Barton F, Aiello LM, Chew EY, Ferris FL, 3rd, Knatterud GL. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss: Early Treatment Diabetic Retinopathy Study Report #18. Invest Ophthalmol Vis Sci. 1998;39(2):233–252. [PubMed] [Google Scholar]
- 11.Fong DS, Segal PP, Myers F, Ferris FL, Hubbard LD, Davis MD. Subretinal fibrosis in diabetic macular edema. ETDRS report 23. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1997;115(7):873–877. doi: 10.1001/archopht.1997.01100160043006. [DOI] [PubMed] [Google Scholar]
- 12.Lai Y, Gao R, Wu D. The study on changes of macular light sensitivity before and after photocoagulation for diabetic macular edema. Zhonghua Yan Ke Za Zhi. 1996;32(5):362–365. [PubMed] [Google Scholar]
- 13.Ladas ID, Theodossiadis GP. Long-term effectiveness of modified grid laser photocoagulation for diffuse diabetic macular edema. Acta Ophthalmol (Copenh) 1993;71(3):393–397. doi: 10.1111/j.1755-3768.1993.tb07154.x. [DOI] [PubMed] [Google Scholar]
- 14.Takatsuna Y, Yamamoto S, Nakamura Y, Tatsumi T, Arai M, Mitamura Y. Long-term therapeutic efficacy of the subthreshold micropulse diode laser photocoagulation for diabetic macular edema. Jpn J Ophthalmol. 2011;55(4):365–369. doi: 10.1007/s10384-011-0033-3. [DOI] [PubMed] [Google Scholar]
- 15.Ohkoshi K, Yamaguchi T. Subthreshold micropulse diode laser photocoagulation for diabetic macular edema in Japanese patients. Am J Ophthalmol. 2010;149(1):133–139. doi: 10.1016/j.ajo.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Nakamura Y, Mitamura Y, Ogata K, Arai M, Takatsuna Y, Yamamoto S. Functional and morphological changes of macula after subthreshold micropulse diode laser photocoagulation for diabetic macular oedema. Eye (Lond) 2010;24(5):784–788. doi: 10.1038/eye.2009.207. [DOI] [PubMed] [Google Scholar]
- 17.Sivaprasad S, Sandhu R, Tandon A, Sayed-Ahmed K, McHugh DA. Subthreshold micropulse diode laser photocoagulation for clinically significant diabetic macular oedema: a three-year follow up. Clin Experiment Ophthalmol. 2007;35(7):640–644. doi: 10.1111/j.1442-9071.2007.01566.x. [DOI] [PubMed] [Google Scholar]
- 18.Grigorian RA, Zaribin MA, Brimacombe M, Tutela A, Roy M, Bhagat N. Comparison of subthreshold micropulse diode laser photocoagulation with conventional laser photocoagulation for clinically significant macular edema in diabetic patients. IOVS. 2004;45:4067. [Google Scholar]
- 19.Inagaki K, Ohkoshi K, Ohde S. Spectral-domain optical coherence tomography imaging of retinal changes after conventional multicolor laser, subthreshold micropulse diode laser, or pattern scanning laser therapy in Japanese with macular edema. Retina. 2012;32(8):1592–1600. doi: 10.1097/IAE.0b013e3182445386. [DOI] [PubMed] [Google Scholar]
- 20.Ohkoshi K, Tsuiki E, Kitaoka T, Yamaguchi T. Visualization of subthreshold micropulse diode laser photocoagulation by scanning laser ophthalmoscopy in the retro mode. Am J Ophthalmol. 2010;150(6):856–862. doi: 10.1016/j.ajo.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 21.Othman IS, Eissa SA, Kotb MS, Sadek SH. Subthreshold diode-laser micropulse photocoagulation as a primary and secondary line of treatment in management of diabetic macular edema. Clin Ophthalmol. 2014;8:653–659. doi: 10.2147/OPTH.S59669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friberg TR. Infrared micropulsed laser treatment for diabetic macular edema-subthreshold versus threshold lesions. Semin Ophthalmol. 2001;16(1):19–24. doi: 10.1076/soph.16.1.19.4217. [DOI] [PubMed] [Google Scholar]
- 23.Casson RJ, Raymond G, Newland HS, Gilhotra JS, Gray TL. Pilot randomized trial of a nanopulse retinal laser versus conventional photocoagulation for the treatment of diabetic macular oedema. Clin Experiment Ophthalmol. 2012;40(6):604–610. doi: 10.1111/j.1442-9071.2012.02756.x. [DOI] [PubMed] [Google Scholar]
- 24.Squirrell DM, Stewart AW, Joondeph BC, Danesh-Meyer HV, McGhee CN, Donaldson ML. Large-spot subthreshold infrared laser to treat diabetic macular edema. Retina. 2008;28(4):615–621. doi: 10.1097/IAE.0b013e31815ee567. [DOI] [PubMed] [Google Scholar]
- 25.Figueira J, Khan J, Nunes S, Sivaprasad S, Rosa A, de Abreu JF, Cunha-Vaz JG, Chong NV. Prospective randomised controlled trial comparing sub-threshold micropulse diode laser photocoagulation and conventional green laser for clinically significant diabetic macular oedema. Br J Ophthalmol. 2009;93(10):1341–1344. doi: 10.1136/bjo.2008.146712. [DOI] [PubMed] [Google Scholar]
- 26.Kumar V, Ghosh B, Mehta DK, Goel N. Functional outcome of subthreshold versus threshold diode laser photocoagulation in diabetic macular oedema. Eye (Lond) 2010;24(9):1459–1465. doi: 10.1038/eye.2010.53. [DOI] [PubMed] [Google Scholar]
- 27.Lavinsky D, Cardillo JA, Melo LA, Jr, Dare A, Farah ME, Belfort R., Jr Randomized clinical trial evaluating mETDRS versus normal or high-density micropulse photocoagulation for diabetic macular edema. Invest Ophthalmol Vis Sci. 2011;52(7):4314–4323. doi: 10.1167/iovs.10-6828. [DOI] [PubMed] [Google Scholar]
- 28.Soheilian M, Garfami KH, Ramezani A, Yaseri M, Peyman GA. Two-year results of a randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus laser in diabetic macular edema. Retina. 2012;32(2):314–321. doi: 10.1097/IAE.0b013e31822f55de. [DOI] [PubMed] [Google Scholar]
- 29.Yilmaz T, Cordero-Coma M, Gallagher MJ, Teasley LA. Systematic review of intravitreal bevacizumab injection for treatment of primary diabetic macular oedema. Acta Ophthalmol. 2011;89(8):709–717. doi: 10.1111/j.1755-3768.2010.01918.x. [DOI] [PubMed] [Google Scholar]
- 30.Wahab S, Ahmed J. Management of cataract with macular oedema due to diabetes mellitus type-II and hypertension with grid laser prior to surgery and intra-vitreal bevacizumab (Avastin) peroperatively. J Pak Med Assoc. 2010;60(10):836–839. [PubMed] [Google Scholar]
- 31.Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial. Arch Ophthalmol. 1998;116(7):874–886. doi: 10.1001/archopht.116.7.874. [DOI] [PubMed] [Google Scholar]
- 32.Ferris F. Early photocoagulation in patients with either type I or type II diabetes. Trans Am Ophthalmol Soc. 1996;94:505–537. [PMC free article] [PubMed] [Google Scholar]
- 33.Friberg TR, Karatza EC. The treatment of macular disease using a micropulsed and continuous wave 810-nm diode laser. Ophthalmology. 1997;104(12):2030–2038. doi: 10.1016/s0161-6420(97)30061-x. [DOI] [PubMed] [Google Scholar]
- 34.Luttrull JK, Dorin G. Subthreshold diode micropulse laser photocoagulation (SDM) as invisible retinal phototherapy for diabetic macular edema: a review. Curr Diabetes Rev. 2012;8(4):274–284. doi: 10.2174/157339912800840523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xie TY, Guo QQ, Wang Y, Wang Q, Chen XY. Randomized, controlled clinical trial comparison of SDM laser versus argon ion laser in diabetic macular edema. Int Eye Sci. 2013;(12):2370–2372. [Google Scholar]
- 36.Venkatesh P, Ramanjulu R, Azad R, Vohra R, Garg S. Subthreshold micropulse diode laser and double frequency neodymium: YAG laser in treatment of diabetic macular edema: a prospective, randomized study using multifocal electroretinography. Photomed Laser Surg. 2011;29(11):727–733. doi: 10.1089/pho.2010.2830. [DOI] [PubMed] [Google Scholar]
- 37.Vujosevic S, Bottega E, Casciano M, Pilotto E, Convento E, Midena E. Microperimetry and fundus autofluorescence in diabetic macular edema: subthreshold micropulse diode laser versus modified early treatment diabetic retinopathy study laser photocoagulation. Retina. 2010;30(6):908–916. doi: 10.1097/IAE.0b013e3181c96986. [DOI] [PubMed] [Google Scholar]
- 38.Laursen ML, Moeller F, Sander B, Sjoelie AK. Subthreshold micropulse diode laser treatment in diabetic macular oedema. Br J Ophthalmol. 2004;88(9):1173–1179. doi: 10.1136/bjo.2003.040949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sivaprasad S, Dorin G. Subthreshold diode laser micropulse photocoagulation for the treatment of diabetic macular edema. Expert Rev Med Devices. 2012;9(2):189–197. doi: 10.1586/erd.12.1. [DOI] [PubMed] [Google Scholar]