Figure 8.
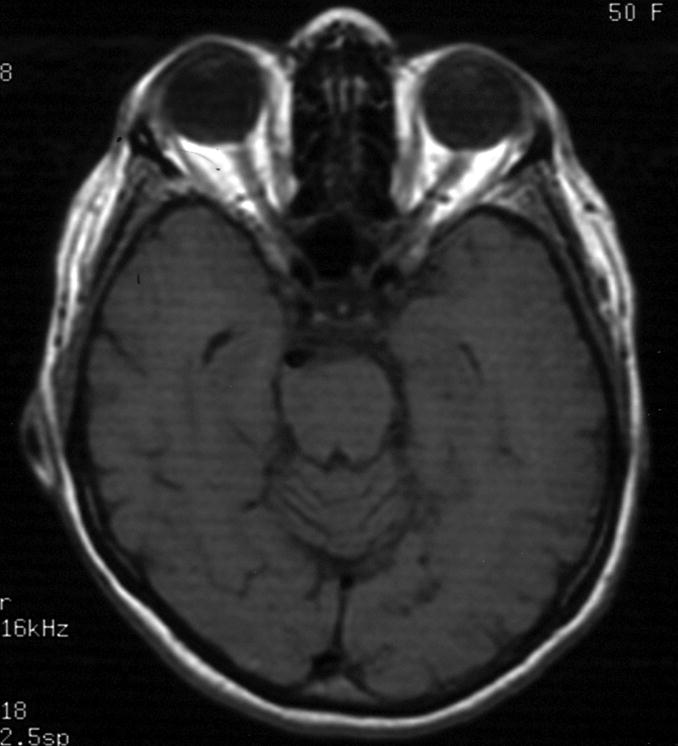
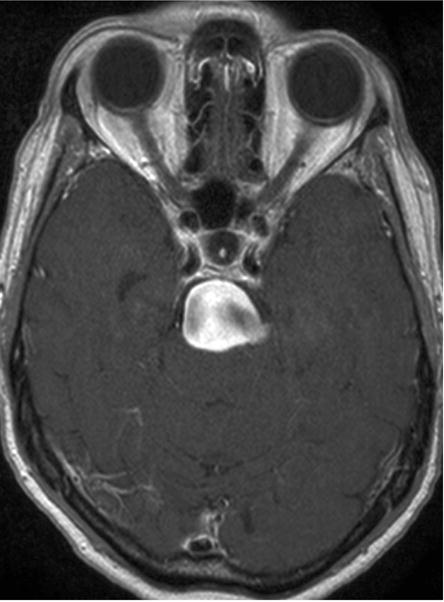
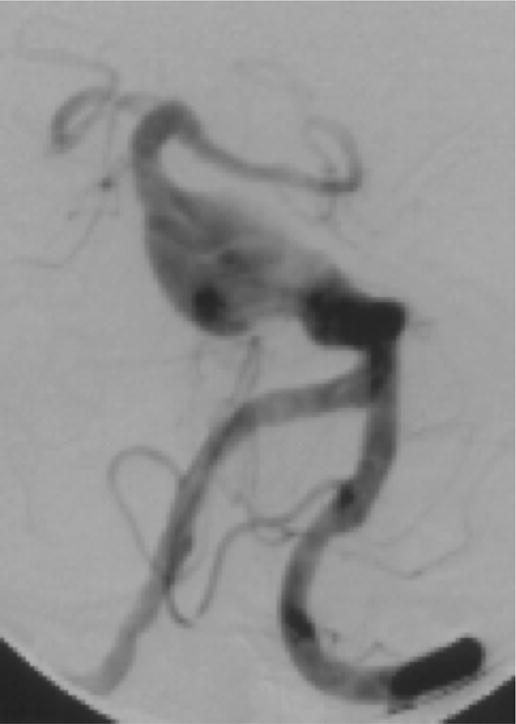

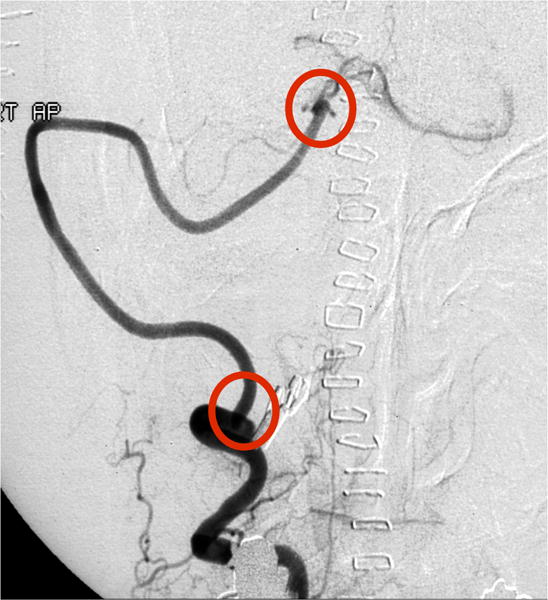
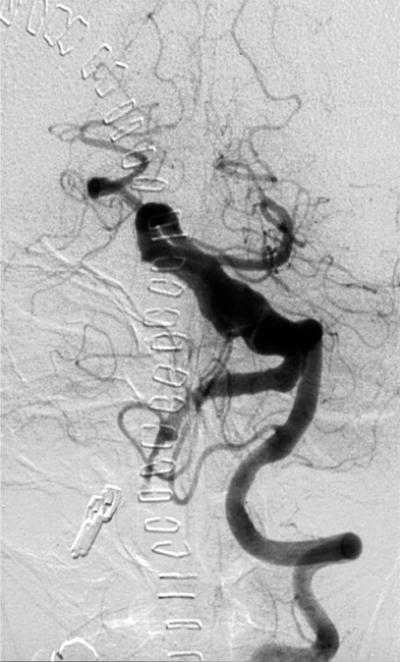
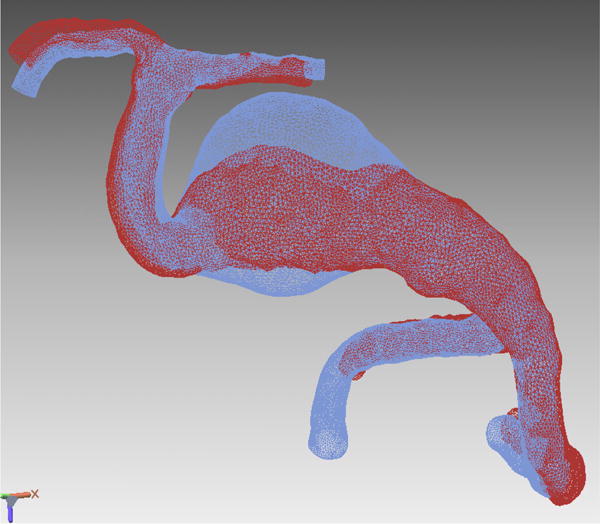
Case example of Phase 2 surgical management. (A) This 51-year-old woman initially presented with mild symptoms from mild basilar dilatation and tortuosity (axial magnetic resonance imaging, T1-weighted image), and was observed for 3 years. (B) During those years, her aneurysm grew and her symptoms became severe (axial magnetic resonance imaging, T1-weighted image with gadolinium; and (C) left vertebral artery digital subtraction angiogram, anteroposterior view). (D) The combined subtemporal-far lateral approach enabled a wide suboccipital craniectomy and duroplasty for posterior fossa relaxation, as seen on axial postoperative CT scan. (E) The postoperative angiogram (right VA angiogram, anteroposterior view) demonstrated patency of the right V3VA-SCA bypass, occlusion of the distal right VA, and filling of the basilar quadrification. (F) The left VA angiogram (anteroposterior view) demonstrated significant thrombosis of aneurysm lumen, (G) shown with superimposed luminal aneurysm volumes pre- (blue) and post-operatively (red) generated with CE-MRA techniques. Although endovascular occlusion of the left VA was intended postoperatively, it was deferred due to her excellent clinical and angiographic outcomes. Her symptoms progressed and the aneurysm enlarged 6 months later, prompting left VA coiling that caused a fatal thrombosis of the basilar trunk.
