Figure 2. Potential mechanisms for the causal role of Lp(a) and OxPL in AS.
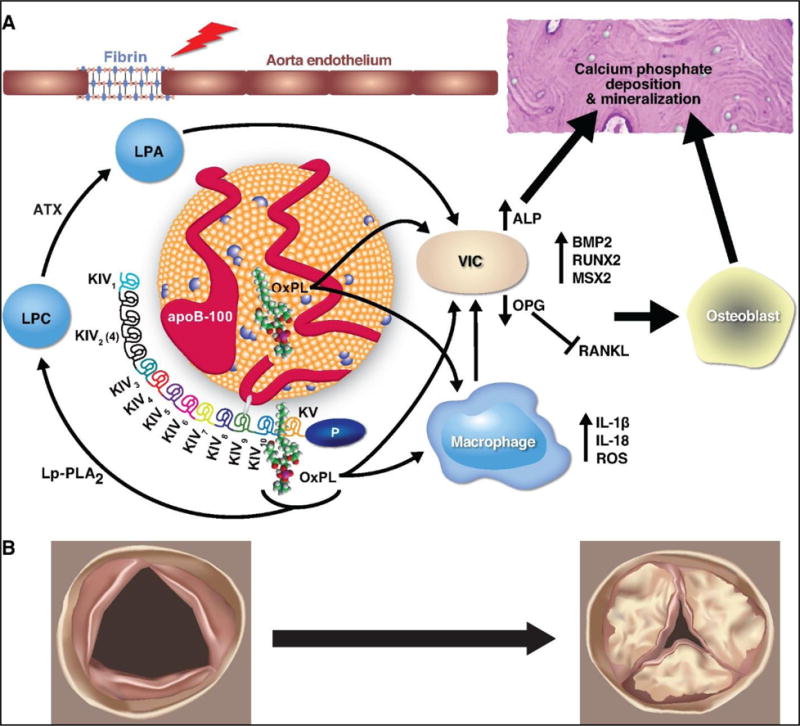
(A) Molecular changes involved in progression of AS. Fibrin is exposed at sites of aorta endothelial injury (depicted by lightning bolt) and can bind to Lp(a), leading to its retention in the valve. Pro-inflammatory lipids on Lp(a), such as OxPL, can promote calcification and bone formation via VIC directly or via up-regulation of ROS and pro-inflammatory cytokines in macrophages. (B) Anatomic changes with progression of a normal valve (left) to a severely stenotic valve (right).
Abbreviations: ATX = autotaxin; Lp-PLA2 = Lipoprotein-associated phospholipase A2; LPC = lysophosphatidylcholine; LPA = lysophosphatidic acid; OxPL = oxidized phospholipids; Lp(a) = lipoprotein(a); ROS = reactive oxygen species; VIC = vascular interstitial cell; ALP = alkaline phosphatase
