Fig. 3.
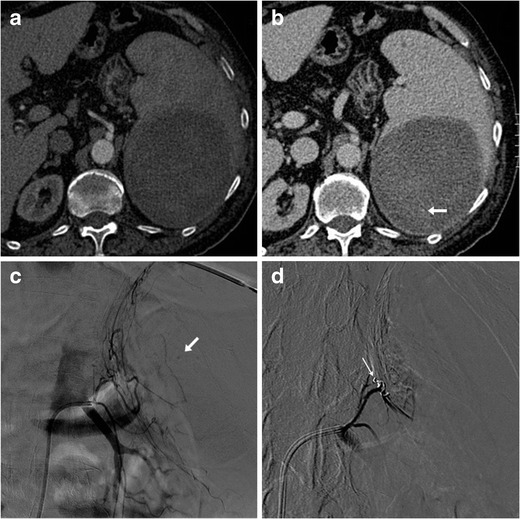
A 73-year-old male on anticoagulation suffered from spontaneous acute abdominal pain. His medical history included congestive heart failure, complete atrioventricular block treated with an implantable cardioverter-defibrillator, previous angioplasty and coronary stenting for acute myocardial infarction, and surgically treated colon carcinoma. Physical examination revealed hypotension and tender left hypocondrium. The international normalized ratio (INR) was 2.6; haemoglobin level was 6.5 g/dl. CT (a, b) revealed a large, roundish mixed attenuation intraparenchymal splenic haematoma without haemoperitoneum. Active bleeding was not evident during the arterial-phase acquisition (a). Faint contrast “blush” (arrow in b) was visible in the venous phase and confirmed at urgent arteriography as minimal bleeding originating from the left phrenic artery (arrow in c). Selective embolization with Spongostan and coil (thin arrow in d) was performed and allowed successful nonoperative management
