Abstract
Context:
Coronary embolization is potentially a fatal sequela of endocarditis. Although the primary cause of acute coronary syndrome is atherosclerotic disease, it is imperative to consider septic embolism as an etiological factor.
Case Report:
Herein, we report a case of ventricular fibrillation and ST-segment depression myocardial infarction occurring in a patient who initially presented with fever and increased urinary frequency. Coronary angiography revealed new 99% occlusion of the left main coronary artery (LMCA). Transesophageal echocardiography showed bioprosthetic aortic valve with an abscess and vegetation. Histologic examination of the embolectomy specimen confirmed the presence of thrombus and Enterococcus faecalis bacteria. Subsequently, the patient was discharged to the skilled nursing facility in a stable condition where he completed 6 weeks of intravenous ampicillin.
Conclusion:
We present a rare case of LMCA embolism due to prosthetic valve endocarditis. The present report also highlights the diagnostic and therapeutic challenges associated with such patients.
Keywords: Coronary artery embolism, enterococcus faecalis, myocardial infarction, prosthetic aortic valve endocarditis
Introduction
Systemic embolization is an unfortunate sequel of infective endocarditis (IE) that can occur despite an appropriate therapy. Cardiac embolization is seen in one-third to one-half of the patients, and the most common complication is heart failure[1] (more common in aortic valve IE than mitral valve). Coronary embolization is not uncommon, and micro-emboli are seen in up to two-third of patients at autopsy. Despite the high incidence of coronary embolism, clinically significant transmural infarcts are very rare with IE.
Case Report
A 69-year-old male presented to the Mount Sinai Saint Luke's Emergency Department with intermittent fever and increased urinary frequency for 1 week. His past medical history was significant for Streptococcus sanguinis tricuspid valve endocarditis, bioprosthetic aortic valve replacement, coronary artery disease (status of post-triple vessel coronary artery bypass grafting), paroxysmal atrial fibrillation (Afib), and type-2 diabetes mellitus. On physical examination, his vitals were notable for an irregular pulse of 112 beats/min, blood pressure of 136/77 mm Hg, respiratory rate of 18/min, rectal temperature of 98°F, and oxygen saturations of 98% on room air. Chest auscultation revealed pulmonary right basilar crackles. There was a cardiac grade 2/6 ejection systolic murmur 6 cm of water at 45° position. Splinter hemorrhages or Osler's nodes were absent.
Laboratory studies were significant for glucose 204 mg/dL and troponin-I 0.05 ng/mL (normal <0.034 ng/mL). Complete blood count, lactic acid, and creatine phosphokinase were within normal limits. Urinalysis was positive for leukocyte esterase and pyuria with 35–50 white blood cells/high-power field. Electrocardiogram (ECG) on admission showed sinus rhythm with first degree AV block and frequent premature atrial complexes. The patient was administered one dose of levofloxacin after drawing blood cultures which came back positive for Gram-positive cocci. On the next day, his antibiotics were changed to vancomycin and gentamicin for suspected endocarditis.
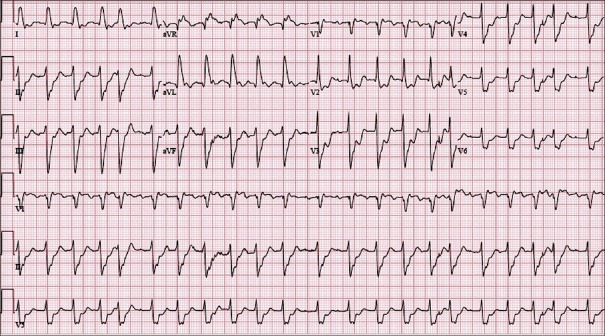
On day 1 of admission, the patient developed acute pulmonary edema and hypoxia following an episode of sub-sternal crushing chest pain. Repeat ECG showed Afib with rapid ventricular response and ST-depressions in leads II, aVF, and V2–V6[Figure 1]. He was managed with nitroglycerine, furosemide, noninvasive positive pressure ventilation, and was transferred to Cardiac Care Unit. Immediate trans-thoracic echocardiogram (TTE) did not show any vegetation or aortic insufficiency. His next troponin-I came back to 10.19 ng/mL and CK-MB was 163.8 ng/mL (0.5–4.7 ng/mL). He was treated for non-ST elevation myocardial infarction with intravenous heparin, aspirin, clopidogrel, statin, and a beta blocker. The patient could not tolerate transesophageal echocardiography (TEE) and had a repeat TTE, which showed inferior and lateral akinesis, moderate systolic dysfunction, and probable vegetation on the noncoronary cusp of aortic valve.
Figure 1.
Electrocardiogram demonstrating atrial fibrillation with rapid ventricular response and ST-depressions in leads II, aVF, and V2–V6
On day 3 of admission, blood cultures grew Enterococcus faecalis. Vancomycin was stopped, and ampicillin was started along with gentamicin. His troponin-I level peaked at 172.09 ng/mL. A presumptive diagnosis of Enterococcal endocarditis of prosthetic aortic valve with embolic myocardial infarction from vegetation was established. Eventually, the patient underwent TEE. It showed moderately decreased left ventricular systolic function with an ejection fraction of 40%, regional wall motion abnormalities with mid and basal anterior and lateral akinesis, bioprosthetic aortic valve with an abscess (thickened intervalvular fibrosa), and small vegetation on the left coronary cusp. Coronary angiography revealed new 99% occlusion of the left main coronary artery (LMCA) and proximal left circumflex artery, chronic total occlusion of ostial left anterior descending artery (LAD) and right coronary artery, patent saphenous vein graft to posterior descending artery, and patent left internal mammary artery graft to the LAD artery. No intervention was done. The patient improved clinically on medical management and stayed hemodynamically stable.
On day 9 of admission, the patient underwent revision of aortic valve replacement, drainage of annular abscess, and LMCA embolectomy. His aortic valve as well as the embolic debris was removed from LMCA grew E. faecalis. Subsequently, he was discharged to the skilled nursing facility in a stable condition where he completed 6 weeks of intravenous ampicillin.
Discussion
Prosthetic valve endocarditis (PVE) is a serious and potentially life-threatening infection. The type of valve does not impact the development of PVE.[1] PVE develops in 1–4% of patients during the 1st year following valve replacement, and in approximately 1% per year thereafter.[1] Staphylococcus aureus is the leading cause of PVE followed by coagulase-negative staphylococci.[2] PVE developing within 2 months of surgery is called early PVE. It is usually hospital-acquired and common pathogens are coagulase-negative Staphylococcus and S. aureus. PVE developing 12 months after surgery is termed as late PVE, which is usually community-acquired and common pathogens include Streptococcal species and S. aureus. Enterococcus faecalis is a nonmotile, facultative anaerobe with plasmid-encoded hemolysin called cytolysin, which is important for pathogenesis in animal models of infection.[3] Enterococcal species are the third leading cause of native valve endocarditis causing 5–10% of the early PVE and 8–12% of late PVE cases.[4] Enterococcal endocarditis has been reported in patients with systemic lupus erythematosus, heroin addicts, following legal abortion and complicating colonoscopy in Heyde's syndrome.
Only six cases have been reported of coronary embolism from IE resulting in sudden cardiac death secondary to LMCA occlusion, left ventricular rupture, and LMCA embolism after abortion.[5] Most embolic events occur to LAD artery and arise from the mitral valve vegetation.[6] Coronary embolism secondary to Enterococcal endocarditis has been reported with papillary muscle rupture due to circumflex artery occlusion arising from native aortic valve vegetation.[7] LMCA embolism from vegetative material is extremely rare, and fatal reports have been described with native aortic valve and mitral valve endocarditis,[8,9] and none of them were conclusively Enterococcal.
Management of septic coronary emboli has not been well-studied. Use of thrombolytics has been largely unfavorable due to increased risk of intracerebral hemorrhage which is mainly due to mycotic aneurysms and cerebral infarcts, which are sequels of IE.[10] Percutaneous transluminal coronary angioplasty carries a risk of re-occlusion due to a mobile embolus, risk of distal embolization, and development of mycotic aneurysm at the balloon dilation site. Furthermore, inserting a stent in bacteremic patients is also controversial due to the risk of seeding of the stent. Percutaneous embolectomy has also been attempted in the past.[11] Continuous daily antiplatelet therapy before hospitalization for IE has shown to decrease embolic events.[12] Good prognosis can be achieved with surgery in patients with native valve endocarditis and PVE, who have moderate to severe heart failure and in patients with late PVE.[13] Surgical embolectomy is an option in patients who need valve surgery. Patients with IE and large vegetation have lower mortality and embolic events if an approach with early surgical intervention is undertaken.[14] In our patient, previous coronary artery bypass graft with good coronary flow resulted in a good prognosis despite occlusion of LMCA by the vegetation.
Conclusion
To our research, this is the first case of LMCA embolism resulting from PVE with E. faecalis. Embolic coronary occlusion should be included in the differential diagnosis of chest pain and increased troponin levels in patients with confirmed or suspected IE because the therapeutic implications are complex and usual measures such as thrombolysis may be dangerous.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Millaire A, Van Belle E, de Groote P, Leroy O, Ducloux G. Obstruction of the left main coronary ostium due to an aortic vegetation: Survival after early surgery. Clin Infect Dis. 1996;22:192–3. doi: 10.1093/clinids/22.1.192. [DOI] [PubMed] [Google Scholar]
- 2.Wang A, Athan E, Pappas PA, Fowler VG, Jr, Olaison L, Paré C, et al. Contemporary clinical profile and outcome of prosthetic valve endocarditis. JAMA. 2007;297:1354–61. doi: 10.1001/jama.297.12.1354. [DOI] [PubMed] [Google Scholar]
- 3.Chow JW, Thal LA, Perri MB, Vazquez JA, Donabedian SM, Clewell DB, et al. Plasmid-associated hemolysin and aggregation substance production contribute to virulence in experimental Enterococcal endocarditis. Antimicrob Agents Chemother. 1993;37:2474–7. doi: 10.1128/aac.37.11.2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001;345:1318–30. doi: 10.1056/NEJMra010082. [DOI] [PubMed] [Google Scholar]
- 5.Carpenter V, Jansson G, Magnusson K, Savela M, Carlsson H, Högberg U. Enterococcal endocarditis following legal abortion. Lakartidningen. 1988;85:2657–8. [PubMed] [Google Scholar]
- 6.Tayama E, Chihara S, Fukunaga S, Akashi H, Aoyagi S, Mizoguchi K. Embolic myocardial infarction and left ventricular rupture due to mitral valve endocarditis. Ann Thorac Cardiovasc Surg. 2007;13:206–8. [PubMed] [Google Scholar]
- 7.Najib MQ, Lee HR, DeValeria PA, Vinales KL, Surapaneni P, Chaliki HP. Anterolateral papillary muscle rupture: An unusual complication of septic coronary embolism. Eur J Echocardiogr. 2011;12:E10. doi: 10.1093/ejechocard/jeq117. [DOI] [PubMed] [Google Scholar]
- 8.Caraballo V. Fatal myocardial infarction resulting from coronary artery septic embolism after abortion: Unusual cause and complication of endocarditis. Ann Emerg Med. 1997;29:175–7. doi: 10.1016/s0196-0644(97)70325-1. [DOI] [PubMed] [Google Scholar]
- 9.Shamsham F, Safi AM, Pomerenko I, Salciccioli L, Feit A, Clark LT, et al. Fatal left main coronary artery embolism from aortic valve endocarditis following cardiac catheterization. Catheter Cardiovasc Interv. 2000;50:74–7. doi: 10.1002/(sici)1522-726x(200005)50:1<74::aid-ccd16>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 10.Hunter AJ, Girard DE. Thrombolytics in infectious endocarditis associated myocardial infarction. J Emerg Med. 2001;21:401–6. doi: 10.1016/s0736-4679(01)00416-4. [DOI] [PubMed] [Google Scholar]
- 11.Glazier JJ, McGinnity JG, Spears JR. Coronary embolism complicating aortic valve endocarditis: Treatment with placement of an intracoronary stent. Clin Cardiol. 1997;20:885–8. doi: 10.1002/clc.4960201018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anavekar NS, Tleyjeh IM, Anavekar NS, Mirzoyev Z, Steckelberg JM, Haddad C, et al. Impact of prior antiplatelet therapy on risk of embolism in infective endocarditis. Clin Infect Dis. 2007;44:1180–6. doi: 10.1086/513197. [DOI] [PubMed] [Google Scholar]
- 13.Richardson JV, Karp RB, Kirklin JW, Dismukes WE. Treatment of infective endocarditis: A 10-year comparative analysis. Circulation. 1978;58:589–97. doi: 10.1161/01.cir.58.4.589. [DOI] [PubMed] [Google Scholar]
- 14.Kang DH, Kim YJ, Kim SH, Sun BJ, Kim DH, Yun SC, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366:2466–73. doi: 10.1056/NEJMoa1112843. [DOI] [PubMed] [Google Scholar]