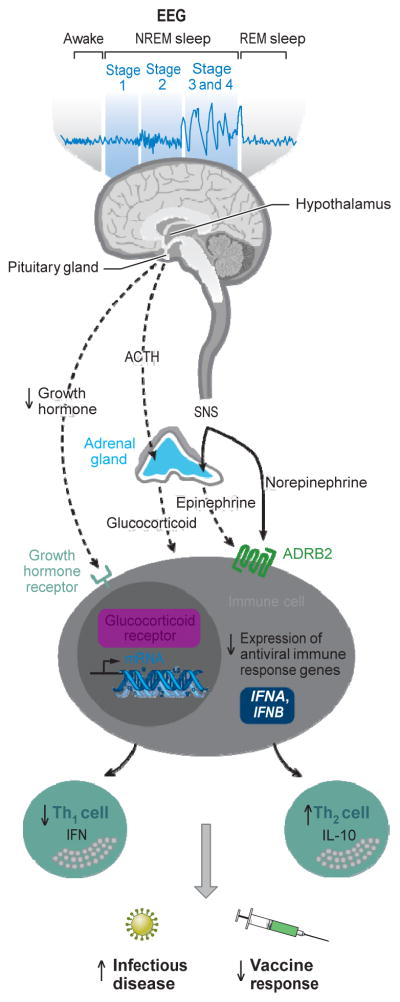
Figure 1.
Sleep disturbance and adaptive immunity. The hypothalamus-pituitary-adrenal axis distributes glucocorticoid hormones through the blood to regulate gene expression in virtually every cell of the body. Sleep disturbance results in hormone activation of the glucocorticoid receptor in leukocytes, which leads to a profound suppression antiviral gene programs [e.g., interferon regulatory factor (IRF)-mediated transcription of type I interferons (IFNs) such as the IFNA and IFNB genes]. Sleep disturbance also activates nerve fibers from the sympathetic nervous system (SNS) to release the neurotransmitter norepinephrine into primary and secondary lymphoid organs, all other major organ systems including the vasculature and perivascular tissues as well as many other peripheral tissues. SNS neural fibers can also stimulate the adrenal gland to release stored epinephrine into the systemic circulation. Both neuromediators stimulate leukocyte adrenergic receptors (e.g., ADRB2) to repress IRF-mediated antiviral IFN response gene (IRG) programs. Sleep also induces the release of growth hormone during the early part of the night, and this hormone acts to enhance the proliferation and differentiation of T cells as well as to promote type 1 cytokine activity; when sleep is disrupted, a reduced amount of growth hormone is released. Suppression of IRF-mediated IRG programs leads to a shift in Th1 to Th2 balance, with decreases in Th1 cell production of IFN and increases in Th2 cell production of interleukin-10 (IL-10). This suppression of adaptive immune response is thought to contribute to increased susceptibility to infectious disease and decreased response to vaccines. Abbreviations: ACTH, adrenocorticotropic hormone; EEG, electroencephalogram.