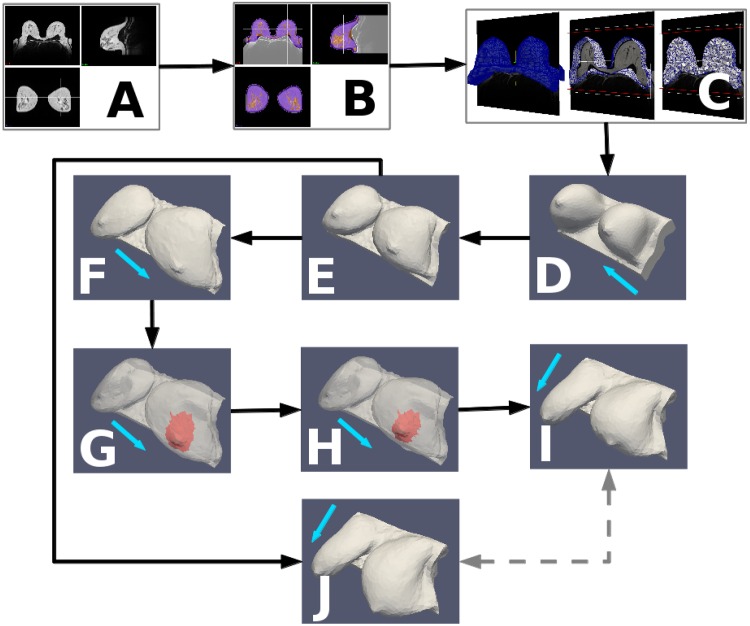
Fig 2. Pipeline of the computational procedure of the surgical simulator.
The prone MRI (A) is segmented into tissue types (B) and a labelled volumetric mesh is created, which forms the basis of the biomechanical model (C). From the prone configuration of the model (D), the unloaded state is computed (E), from which re-application of gravity simulates the supine (F) and upright (J) configurations prior to surgery. Surgical planning, to specify the resected surgical “wound” (shown in red), is performed in the supine pose (G) and results in a cosmetic outcome prediction (H) which is transformed into the upright configuration (I) for presentation to the user. The pre- (J) and post- (I) surgical simulations can then be compared (dashed arrows) to reveal the predicted deformation of the breast due to surgery. The blue arrows indicate the direction of gravity: (D) from posterior to anterior (i.e. prone), (F,G,H) from anterior to posterior (i.e. supine) and (I,J) superior to inferior (i.e. upright). Note in G and H, the breast skin is shown transparent to visualise the excision region located inside the breast model (see also the adopted surgical plans in the Results section).