Abstract
Purpose
Little research has examined how prostate cancer patients’ and their spouses’ appraisals of illness and quality of life (QOL) interact with one another. This study examined the interdependent relationships between their appraisals of illness and QOL, and if their perceived dyadic communication mediated these relationships.
Methods
We used the Actor-Partner Interdependence Mediation Model (APIMeM) approach to conduct a secondary analysis of longitudinal data from 124 prostate cancer patient-spouse dyads. We examined actor effects (each person’s influence on his/her own outcomes) and partner effects (each person’s influence on his/her partner’s outcomes). Appraisals of illness, perceived dyadic communication, and QOL were measured using Appraisal of Illness scale, Lewis Mutuality and Interpersonal Sensitivity Scale, and Functional Assessment of Chronic Illness Therapy general scale, respectively. Analyses controlled for effects of prostate cancer symptoms and demographic factors.
Results
Among actor effects, spouses with more negative appraisals at baseline perceived worse dyadic communication 4-months later (p<.05) and worse QOL 8-months later (p<.001). Patients and spouses who perceived more dyadic communication at 4 months had better QOL at 8 months (p<.01). Among partner effects, there was only weak evidence for an association between patient perceived dyadic communication at 4-months and better spouse QOL at 8 months follow-up (p=.05). No mediation effects were found.
Conclusions
Patients’ and spouses’ appraisals of the illness and their dyadic communication were associated with their long-term QOL. Interventions that reduce negative appraisals of illness and promote dyadic communication may improve QOL for both patients with prostate cancer and their spouses.
Keywords: appraisal, perceived dyadic communication, quality of life, prostate cancer, path analysis, Actor-Partner Interdependence Mediation Model (APIMeM)
BACKGROUND
Prostate cancer (PCa) is the most prevalent non-skin cancer and the second leading cause of cancer-related deaths among men in the U.S. [1]. Men with PCa often experience decreased emotional, social, physical, and functional well-being—that is, decreased quality of life (QOL)—and these effects persist long after treatments end [6]. PCa and its treatment-related side effects also negatively affect spouses [23], who sometimes report worse QOL than patients [30].
A meta-analysis has shown that patients and their spouses react to cancer as one “emotional system,” and that a reciprocal relationship exists between each person’s emotional response to illness [11]. Studies also indicate that their appraisals of psychosocial issues are positively correlated, as is their QOL [39, 40]. Yet little theory-driven research has examined how patients’ and spouses’ responses to PCa affect one another’s QOL over time, underscoring the need for dyadic interventions to improve QOL of both PCa patients and their partners. It is also important to understand the underlying mechanism through which antecedent factors affect outcomes to determine where along the pathway to target interventions.
Theoretical Framework
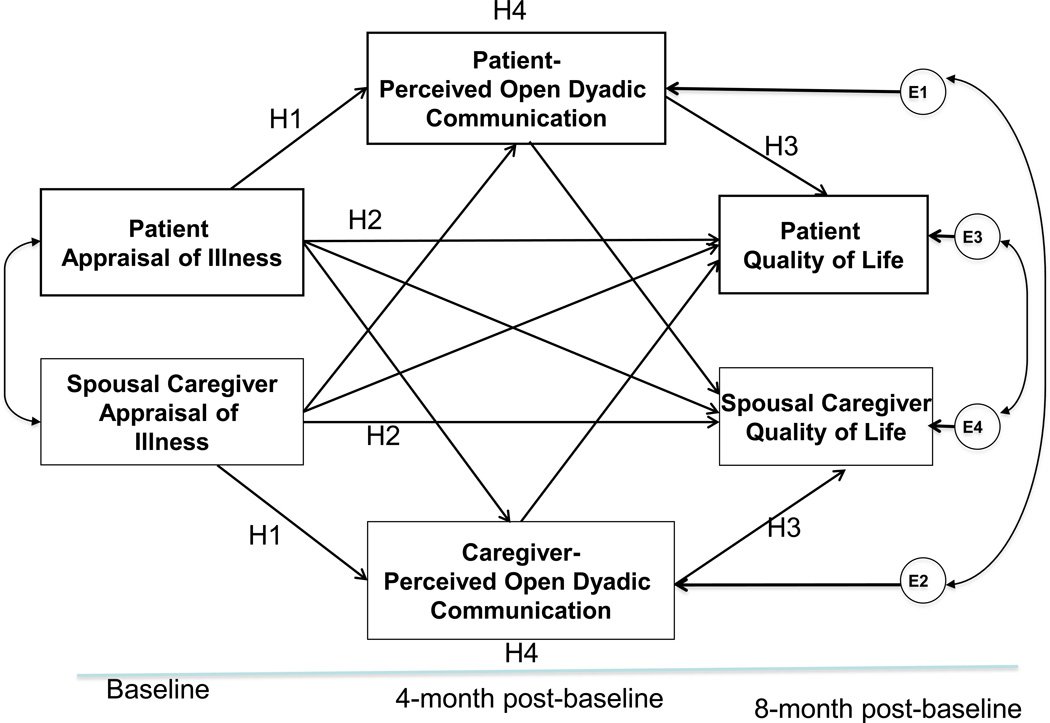
This study addressed these gaps by applying a conceptual framework (Figure 1) based on the transactional model of stress and coping [19] and interdependence theory [16]. The transactional model provides useful insights into an individual’s response to a stressor such as prostate cancer. This stressor triggers an appraisal and coping process in which individuals assess the degree of threat associated with the stressor and their resources to cope with it [19]. According to the model, appraisals concern the perceived seriousness of the stressor [19]. Those situations that cause more stress, and greater need for coping, are appraised as having greater potential to cause serious harm. When patients and spouses are faced with a PCa diagnosis, their appraisals of its seriousness can vary depending on treatment-related side effects, prognosis, and strains associated with receiving and providing care [8, 9]. Their negative appraisals are related to poorer QOL [10, 12, 18], consistent with the theoretical view that the stress and coping process extends over time and affects health outcomes [19]. Findings from family-based cognitive-behavioral interventions that promote positive reappraisal have reduced negative appraisals in cancer populations[28, 32].
Figure 1. Modified Family Stress-Coping Model.
Interdependence theory extends the transactional model’s focus on stress and coping to an interpersonal context, and appraisal and behavioral processes at a dyadic level (i.e., how each member of a couple responds to an event, how their responses interact with one another, and how their interactions influence each others’ outcomes) [16, 38]. This theory also suggests that accounting for both partners’ perspectives provides unique insight into individual and joint influences on their respective outcomes. In this study, it provides insight into a key coping resource available to couples managing PCa—their ability to communicate about PCa-related psychosocial issues (i.e., dyadic communication)[24]. More specifically, dyadic communication refers to the degree to which patients and their spouses each perceive that they openly communicate about issues related to PCa. Patients with PCa and their spouses often have difficulty communicating about cancer-related issues [8, 9]. However, cancer-related communication between patients and spouses is an important coping resource for managing the demands of cancer and the side-effects of treatment [21]. Communication enables them to understand and address each other’s fears and concerns, reframe negative effects of the illness, and coordinate their responses to stressors. More dyadic communication has been associated with better QOL in both patients and spouses coping with PCa [23, 40].
Our conceptual framework is consistent with the view that PCa diagnosis and treatment trigger patients’ and spouses’ appraisal and coping processes. One person’s appraisals and coping resources—in this case, the perception that it is possible to discuss important issues surrounding PCa with his/her spouse—interact with those of the other person to influence how well couples work together to manage emotional and practical challenges of the illness. Ultimately, the appraisals and coping resources of both members of the couple contribute to their respective health outcomes, including QOL. More negative appraisals of illness are expected to promote greater coping attempts, and for many couples those attempts will include efforts to discuss illness-related changes with each other. However, greater stress and more complicated issues surrounding PCa may interfere with their ability to communicate about PCa, gain mutual understanding, and support one another in a satisfactory and productive manner [42]. Consequently, patients’ and spouses’ perceived dyadic communication may help explain associations between their appraisals and QOL. More negative appraisals of PCa-related stress in one or both partners may be associated with each partners’ perception of poorer dyadic communication. As couples perceive PCa-related challenges to be more threatening, it may complicate their attempts to have open and constructive communication about PCa, and increase the likelihood that their communication falls into patterns shown to be malaptive) [37]. Poorer perceived dyadic communication would then be expected to reduce subsequent QOL [40].
Aims and Hypothesis
This longitudinal study prospectively examined interdependent associations between patients’ and spouses’ PCa appraisals, perceived dyadic communication, and QOL using the Actor-Partner Interdependence Mediation Model (APIMeM) [5]. The Actor-Partner Interdependence Model (APIM) allows simultaneous examination of the impact of a person’s causal variable on his or her own outcome (actor effect) and on the outcome of the partner (partner effect) [5]. APIMeM extends the standard APIM by adding a third variable pair to examine the mediation effects of dyadic communication [17]. Our conceptual framework hypothesized the following relationships (Figure 1).
Hypothesis 1: More negative appraisals in patients and spouses at baseline will be associated with poorer perceived dyadic communication about cancer in each person (actor effect) and in his/her spouse (partner effect) at 4-months follow-up.
Hypothesis 2: More negative appraisals in patients and spouses at baseline will be associated with worse QOL in each person (actor effect) and in his/her spouse (partner effect) at 8-months follow-up.
Hypothesis 3: Poorer perceived dyadic communication at 4-months in patients and spouses will be associated with worse QOL in each person (actor effect) and in his/her spouse (partner effect) at 8-months follow-up.
Hypothesis 4: Poorer perceived dyadic communication at 4-months will mediate the associations between patients’ and spouses’ appraisals at baseline and their QOL at 8 months follow-up (both actor and partner effects).
METHODS
Study Design and Sample
This was a secondary analysis of longitudinal data from a randomized controlled trial (RCT) that examined the effects of a couple-based intervention on QOL for PCa patients and their spouses [32]. Recruited from cancer centers and hospitals in the Midwest United States, patients were eligible if they were within 2–4 months of one of three PCa-related changes in their health status: a new diagnosis, biochemical recurrence (i.e., rising PSA), or progression of disease.
RCT procedures were approved by Institutional Review Boards at the study sites. Details about the study sample and procedures were reported previously [30, 32]. Among 429 patient-spouse dyads referred to the study, 263 were consented, enrolled (enrollment rate, 68.7%) and then randomized to a psycho-educational program or a usual care control condition [30]. The present study only included dyads from the control group (N=124) to eliminate any effects of the intervention on the study variables. Among the 134 dyads that completed the baseline assessment, ten patients died during the study period and were excluded from analyses.
Measurements
Patients and spouses independently completed questionnaires during in-person interviews in their home with a research nurse. PCa-related appraisals were measured at baseline using a 20-item Appraisal of Illness Scale, which assesses patients’ and spouses’ perceptions of the degree of threat associated with PCa and a broader perspective on their ability to manage the ramifications of PCa (e.g., “The situation threatens to overwhelm me”). Abstracted from the original 32-item patient version and the 27-item caregiver versions of the Appraisal Scales [33, 34], measurement items were identical for patients and spouses. The scale uses a 5-point Likert response scale ranging from 1 (very false) to 5 (very true) and mean scores were calculated.
Perceived dyadic communication about issues related to PCa (e.g., fears, concerns, illness management) was measured 4-months post-baseline with the 23-item Lewis Mutuality and Interpersonal Sensitivity Scale (MIS) [20] (e.g., “We spend a lot of time talking about how things are going with the cancer”; “We approach the cancer with the same thoughts and feelings”). The MIS uses a 5-point Likert response scale ranging from 1 (low) to 5 (high). Mean scores were calculated.
Quality of Life was measured 8-months post-baseline using the 27-item Functional Assessment of Chronic Illness Therapy general scale (FACT-G) [4]. With permission of FACIT.org, the spouse version of FACT-G was slightly modified so wording allowed partners to report their own QOL [29]. It has been used to measure partner QOL in multiple prior studies, with evidence of reliability and validity [28, 30, 31]. Patients and spouses reported their own general QOL in physical, social/family, emotional, and functional domains. The total scores were used.
We also included the baseline covariates. Patient PCa-specific symptoms were measured using the 26-item Prostate Cancer Index Composite (EPIC) [43], which include domains of urinary irritability and incontinence, bowel, sexual, and hormonal symptoms. The demographic data (e.g., age and education) were assessed using the Risk for Distress screening questionnaire [26].
Data Analysis
We used the APIMeM [17] and MPlus version 7 [27] to test hypotheses. We conducted analyses, using maximum likelihood estimation, to account for the interdependence of data gathered from dyads (e.g., patients’ and spouses’ appraisals and dyadic communication are related because of shared experiences). The model consisted of three pairs of variables: patients’ and spouses’ appraisals at baseline (predictors), perceived dyadic communication at 4-months (mediators), and QOL at 8-months follow-up (outcomes). The model also hypothesized potential direct effects (six actor and six partner effects) and indirect effects (eight mediation effects that indirectly linked appraisals with QOL through dyadic communication). The model estimated relationships between observed variables (appraisals, perceived dyadic communication, and QOL) and variances and covariances among these variables. Adequacy of model fit was evaluated using the following indices and criteria: a chi-square to degrees of freedom ratio (CMIN/DF) of less than 2; a CFI above .90; and a RMSEA value of .05 or less [15].
Bootstrapping was used to evaluate the significance of specific path parameters, as well as the direct, indirect (mediation), and total effects within a model [22]. Bootstrapped 95% confidence intervals (CI) that did not include zero indicated parameters and effects that were statistically significant. The total and direct effects between appraisals and QOL in patients and spouses (both the actor and partner effects) were estimated to calculate the percentage of effects that were mediated [22].
RESULTS
Characteristics of participants
Most patients (86.3%) and spouses (83.9%) were non-Hispanic White. Patients reported higher education levels than their spouses (p<.001) (Table 1). Patients were diagnosed with localized (60%), biochemical recurrent (15%), or advanced (25%) cancer. Table 2 displays the Cronbach’s alpha, descriptive results for patients’ and spouses’ appraisals, perceived dyadic communication, and QOL, and correlations among these variables.
Table 1.
Characteristics of patients and spouses (N=124 dyads)
| Patient (n=124) | Spouse (n=124) | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (Year) | 62.34 | 9.07 | 58.78 | 9.48 |
| Education (Year) | 16.10 | 3.66 | 14.86 | 2.68 |
| Length of relationship (years) | 31.70 | 14.13 | ||
| Time since diagnosis (months) | 26.41 | 38.13 | ||
| % (N) | % (N) | |||
| Race | ||||
| American Indian | 0.8% (1) | 1.6% (2) | ||
| Asian | -- | 0.8% (1) | ||
| Black/African American | 12.1% (15) | 12.1% (15) | ||
| White | 86.3% (107) | 83.9% (104) | ||
| Multiracial | 0.8% (1) | -- | ||
| Missing/not reported | -- | 1.6% (2) | ||
| Ethnicity | ||||
| Hispanic | 3.2% (4) | 1.6% (2) | ||
| Family Income (N=117) | ||||
| <$50,000 | 27.4% (34) | |||
| $50,001–$75,000 | 18.5% (23) | |||
| >$75,001 | 48.4% (60) | |||
| Phase of prostate cancer | ||||
| Localized | 59.7% (74) | |||
| Recurrent | 15.3% (19) | |||
| Advanced | 25% (31) | |||
Table 2.
Correlations among Patient Measures and Spouse Measures
| Measures a | Cronbach’s alpha |
Patient | Spouse | ||||
|---|---|---|---|---|---|---|---|
| Appraisal T1 |
Communica tion T2 |
QOL T3 | Appraisal T1 |
Communica tion T2 |
QOL T3 | ||
| Patient | |||||||
| 1. Appraisal T1 | 0.81 | 1 | |||||
| 2. Communication T2 | 0.92 | .241* | 1 | ||||
| 3. QOL T3 | 0.92 | .589*** | .456*** | 1 | |||
| Spouse | |||||||
| 4. Appraisal T1 | 0.79 | .210* | .161+ | .232* | 1 | ||
| 5. Communication T2 | 0.92 | .108 | .532*** | .294** | .229* | 1 | |
| 6. QOL T3 | 0.91 | .259** | .171+ | .315** | .456*** | .447*** | 1 |
| Mean | 2.63 | 3.58 | 87.91 | 2.77 | 3.66 | 83.86 | |
| SD | .92 | .69 | 11.29 | .76 | .66 | 14.19 | |
: Higher scores indicate more positive appraisals, perceived greater open PCa-related dyadic communication between patients and spouses, and better QOL.
T1=Time 1; T2=Time 2; T3=Time 3. QOL=quality of life.
p<.10;
p<.05;
p<.01;
p<.001.
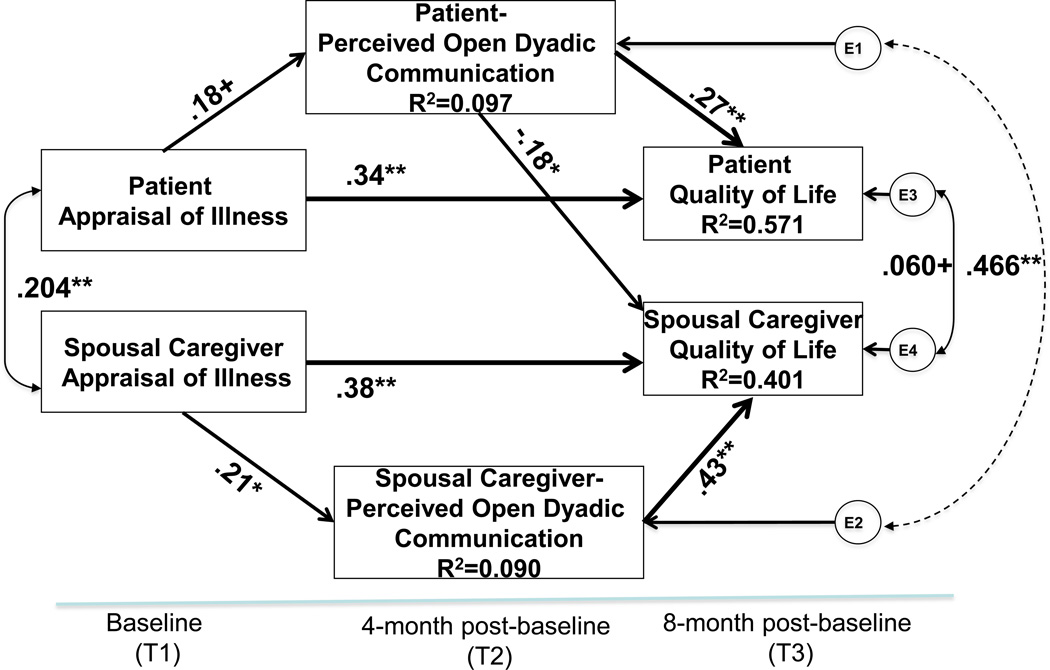
Results of APIMeM
Figure 2 provides standardized estimates for the APIMeM. The model fit was satisfactory: Chi-square=9.831, df=8, p-value=.2771; CMIN/DF=1.229; RMSEA=.043; CFI=.989; and SRMR=.019. Results indicated significant actor effects for patients and spouses (Hypotheses 1 and 2). Patients who held more negative appraisals at baseline reported worse QOL 8 months later (β=.336; p<.001). Furthermore, patients who had worse perceived dyadic communication at 4 months had worse QOL at 8 months post-baseline (β=.266; p=.004). There was weak evidence (β=0.184, p=0.060) for an association between patients' negative appraisals at baseline and their perceptions of worse dyadic communication 4 months later.
Figure 2. Path Analysis Results.
Note: Results are standardized. Control variables include age, education, and patient prostate cancer symptoms. RMSEA = .043; CFI = .989; CMIN/DF =1 .229. +p<.10; *p<.05; **p<.01.
The results also supported actor effects for spouses. Spouses who held more negative appraisals at baseline reported worse perceived dyadic communication 4 months later (β=.208; p=.049). Worse QOL in spouses at 8-month follow-up was predicted by their more negative appraisals at baseline (β=.379; p<.001) and worse perceived dyadic communication at 4-months post-baseline (β=.428; p<.001).
Among partner effects (Hypothesis 3), there is a weak level of evidence for an association between patient perception of worse dyadic communication at 4 months and better spouse QOL at 8 months (β= −.183; p=.050), contrary to expectations. Among the hypothesized mediation effects, only the relationship among spouses’ appraisals, perceived dyadic communication, and QOL met mediation criteria [2]; patient variables did not meet the criteria to assess mediation. We found no significant mediation effects among spouse variables (95%CI [−0.009, .211]).
Among all covatiates, patients’ urinary (β=.156; p=.050) and hormone symptoms (β=.218; p=.001) at baseline were significantly associated with their QOL at 8-months. The path model—including patients’ and spouses’ appraisals, perceived dyadic communication, and patient PCa urinary and hormonal symptoms—explained 57% of the variance in patients’ QOL and 40% of spouses’ QOL at 8 months.
DISCUSSION
This study was the first to use a dyadic approach to investigate prospective, interdependent relations between patients’ and spouses’ PCa appraisals (i.e., assessment of how stressful it was for each of them), their perceived dyadic communication, and each person’s QOL. We used a theory-based analytic approach to simultaneously examine the effects of patients’ and spouses’ appraisals and perceived dyadic communication on their own QOL (actor effects) and on their partner’s QOL (partner effects), and the mechanism underlying these relationships (mediation). Theorized partner effects and the mediating role of dyadic communication received only minimal support. Potential reasons for these findings are discussed below. However, most theorized actor effects were supported: each person’s own appraisals of illness and perceived dyadic communication about PCa were significantly associated with their own QOL. The appraisals of illness and perceived dyadic communication measures (together with urinary and hormonal symptom variables) explained 57% and 40% of the variances in QOL in patients and spouses, respectively.
The results indicated that appraisals of PCa at baseline were directly associated with QOL 8 months later for both patients and their spouses, consistent with existing evidence. In previous studies, less negative appraisals predicted better physical [18, 35] and emotional QOL [35] among patients; similarly, less negative appraisals predicted better QOL among spouses [7, 18]. Contrary to our hypotheses, actor effects predominated, indicating that each person’s appraisals were more likely to be important predictors of their subsequent QOL than the other person’s. Thus, helping each member of the couple reduce their own negative appraisals of PCa may be an effective intervention strategy to improve QOL for both patients and their spouses. It is possible to appraise a stressor such as PCa-related issues as negative, but relatively non-threatening (e.g., a manageable challenge rather than a threat) or less catastrophic (when facing end-of-life). To the extent this occurs, this person can seek ways to master the situation faced or replace their maladaptive thought patterns with more adaptive ones (e.g., use practical task-focused coping strategies) in order to gain or to restore his or her well-being [19].
A unique contribution of this study is that, in addition to appraisals, it also examined implications of an important aspect of the social context in which PCa unfolds—how couples communicate about PCa-related challenges. As with appraisals, actor effects prevailed: each person’s own perceptions of their dyadic communication about PCa predicted his/her own QOL, over and above any effects of appraisals. There are a number of potential explanations for the predominance of actor effects. First, couples do not completely share their perceptions at the degree to which they communicate openly about cancer (as shown by the moderate correlation between patients’ and spouses’ perceived dyadic communication). The fact that actor effects were stronger than partner effects is consistent with the fact that individuals’ own subjective experience of a situation (rather than their partner’s subjective experience of the situation) is more likely to guide their responses to that situation. The fact that PCa is a disease experienced primarily among aging persons is also potentially relevant [14]. Older people frequently interact with their families and, in light of the stress put upon the couple by PCa, their QOL may be closely related to the support, companionship, and assistance they get from these relationships. Future research should assess communication with family and friends in addition to communication with the spouse. Other theoretical models may also help understand the relatively weak partner effects, including Bodenmann’s stress cascade model [3], which posits that individuals in a couple first attempt to manage adverse effects of a stressor by coping individually, then turn to partners and others for support if they find that these initial coping efforts are inadequate.
Yet, quality communication between spouses is a critical strength for couples, including older adults (e.g., those in retirement years [25]). Dyadic communication becomes even more important when couples face a serious health-related stressor such as PCa, because it facilitates exchanges of emotional and tangible support [23]. Previous research has reported that dyadic communication predicted better QOL in both patients and spouses [41], less hopelessness in patients, and less uncertainty about the illness in the healthy spouses [18]. Results from our study put this finding in a larger context, are consistent with existing evidence, and suggest benefits of improving dyadic communication to promote better QOL for PCa patients and spouses. Interventions that employ strategies to enhance dyadic communication about cancer-related issues (while managing PCa-related symptoms) may promote better QOL for patients and spouses, even if each individual’s perception of that communication mainly affects his/her own QOL.
Interestingly, we did not find significant mediation effects—that is, perceived dyadic communication did not mediate effects of negative appraisals on QOL. This finding most likely reflects relatively weak associations between appraisals and dyadic communication for both patients and spouses. We had hypothesized that more negative illness appraisals would adversely affect perceived dyadic communication (e.g., by limiting each person’s ability or willingness to talk about challenges of PCa in an open and effective manner). Bivariate correlations supported the direction of this association, but were small in size. Yet, findings from our model indicated that individuals’ perceptions of dyadic communication were uniquely associated with their own QOL, over and above effects of their own and their spouses’ appraisals and their spouses’ perceived dyadic communication. Future research is needed to examine the interrelations among couples’ illness appraisals and perceptions of dyadic communications in couples coping with PCa.
We found one marginally significant partner effect: when patients perceived less dyadic communication at 4 months, their spouses reported better QOL at 8 months. This marginally significant finding needs to be viewed with caution until replicated, raising interesting questions for future research. Although counter to the association we hypothesized, past research has shown that not all communication about cancer is helpful. Certain types of communication (e.g., urging patients to increase healthy behaviors) have been associated with poorer physical and mental health [13], whereas communication of love and gratitude contributed to better QOL in patients [36]. It is also possible that spouses assumed that patients were having fewer problems when they had less communication about PCa, which bolstered spouses’ QOL. Qualitative research could explore the dynamics operating in these couples, providing useful insights into an individual’s experiences and how each person’s cognitive and emotional responses to PCa are perceived by the other person.
The dearth of partner effects indicated that each person’s appraisals and perceived dyadic communication had little effect on his or her partner’s subsequent QOL. One possible explanation is that patients and spouses were most aware of (and therefore most affected by), their own feelings about PCa, effects of its symptoms (e.g., urinary incontinence), and related experiences. To the extent this occurred, they would have been relatively unaffected by how their spouses responded to PCa. It is also possible that we used measures of dyadic communication rather each person’s own communication to captured dyadic interaction and interdependence, which may have hindered our ability to detect the partner effects. Future research is needed to examine whether and how perceptions of dyadic and individual communication are related.
This study has limitations. First, the sample was primarily non-Hispanic White, well-educated, and middle class. Our findings may not be generalizable to more diverse samples (e.g., dyads of minority racial groups or low socio-economic status). Second, all patients were males and all spouses were females. Findings should be interpreted in light of the fact that the stress-coping process at the intrapersonal and intracouple levels in female patients and their male spouses and/or in same sex couples may differ. Research examining these differences would provide valuable insight into gender versus role effects in the stress-coping process after a cancer diagnosis. We also used self-reported perceived dyadic communication instead of observed communication behaviors. Patients and spouses may have reported having more or less dyadic communication than what really happened because of social desirability.
CONCLUSIONS
Our findings underscore the importance of assessing both patients’ and spouses’ illness appraisals and perceived dyadic communication because both factors independently affected their QOL. Actor effects were more powerful than partner effects, suggesting that interventions may be most powerful in improving QOL for both patients with PCa and their spouses if they focus on reducing each person’s negative appraisals and enhancing dyadic communication. These findings also provide empirical evidence for dyadic-based cognitive-behavioral interventions that focus on positive reappraisal therapies in improving QOL for couples [28, 32].
Table 3.
Parameter Estimates
| The Paths | Estimate | 95% CI | p | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Actor Effects | |||||
| Patient | Appraisal -> Dyadic Communication | .18 | −.02 | .37 | .060 |
| Appraisal -> QOL | .34 | .21 | .45 | <.001 | |
| Dyadic Communication -> QOL | .27 | .12 | .47 | .004 | |
| Spouse | Appraisal -> Dyadic Communication | .21 | −.02 | .40 | .049 |
| Appraisal -> QOL | .38 | .19 | .62 | <.001 | |
| Dyadic Communication -> QOL | .43 | .20 | .61 | <.001 | |
| Partner Effects | |||||
| Patient Appraisal -> Spouse Dyadic Communication | .02 | −.18 | .18 | .832 | |
| Patient Appraisal -> Spouse QOL | .11 | −.04 | .29 | .212 | |
| Patient Dyadic Communication -> Spouse QOL | −.18 | −.37 | −.02 | .050 | |
| Spouse Appraisal -> Patient Dyadic Communication | .11 | −.14 | .33 | .363 | |
| Spouse Appraisal -> Patient QOL | −.01 | −.13 | .12 | .838 | |
| Spouse Dyadic Communication -> Patient QOL | .04 | −.12 | .18 | .576 | |
| Mediation Testing | |||||
|---|---|---|---|---|---|
| Relationships | Estimate | 95% CI | Percent of Total Effect |
||
| Lower | Upper | ||||
| Actor Effects | |||||
| Patient | Total effect (Direct + Indirect) | .39 | .26 | .52 | |
| Direct effect: Appraisal → QOL | .34 | .21 | .45 | 87.0%** | |
| Indirect effects (Mediation) | .05 | .001 | .14 | Na [2] | |
| Patient appraisal → Patient communication → Patient QOL | |||||
| Patient appraisal → Spouse communication→ Patient QOL | |||||
| Spouse | Total effect | .45 | .26 | .71 | |
| Direct effect: Appraisal → QOL | .38 | .19 | .62 | 84%** | |
| Indirect effects (Mediation) | .07 | −.01 | .18 | 16% [1] | |
| Spouse appraisal → Patient communication → Spouse QOL | |||||
| Spouse appraisal → Spouse communication → Spouse QOL | |||||
| Partner Effects | |||||
| Patient | Total effect | .09 | −.08 | .28 | |
| Direct effect: Appraisal → Spouse QOL | .11 | −.04 | .29 | Na[2] | |
| Indirect effects (Mediation) | −.03 | −.13 | .04 | ||
| Patient appraisal → Patient communication → Spouse QOL | |||||
| Patient appraisal → Spouse communication → Spouse QOL | |||||
| Spouse | Total effect | .02 | −.11 | .16 | |
| Direct effect: Appraisal → Patient QOL | −.01 | −.13 | .12 | Na[2] | |
| Indirect effects (Mediation) | .04 | −.03 | .14 | ||
| Spouse appraisal → Patient communication → Patient QOL | |||||
| Spouse appraisal → Spouse communication → Patient QOL | |||||
Note:
p<.05;
p<.01.
This mediation effect was not significant at 95% CI [−0.009, .211] and marginally significant at the 90% CI [0.008; 0.185].
Criteria for mediation testing were not met in these relationships, and thus, mediation effects were not tested.
Acknowledgments
The study was funded in part by a research grant from National Cancer Institute (R01CA10738, PI: Northouse), a Ruth L. Kirschstein National Research Service Award (NRSA) (F31NR010990, PI: Song), and a KL2 grant to Dr. Song (KL2TR001109) sponsored by the University of North Carolina Clinical and Translational Sciences Award (CTSA) (UL1TR001111, PI: Runge), and postdoctoral fellowships (Ellis) funded by a grant from the National Cancer Instititue (5T32CA128582-07, PI: Eng) and the UNC Center for Health Equity Research (CHER) (PI: Corbie-Smith). The authors are grateful for Dr. Darlene W Mood’s (Wayne State University College of Nursing, Detroit, MI) conceptual contribution to this paper.
Footnotes
Conflict of Interest Statement: None.
Contributor Information
Lixin Song, University of North Carolina School of Nursing, and Member, UNC Lineberger Comprehensive Cancer Center, Chapel Hill, NC, 27599..
Christine Rini, University of North Carolina at Chapel Hill, Gillings School of Global Public Health, and Member, UNC Lineberger Comprehensive Cancer Center, Chapel Hill, NC 27599.
Katrina R. Ellis, University of North Carolina School of Public Health, Chapel Hill, NC 27599.
Laurel L. Northouse, University of Michigan School of Nursing, Ann Arbor, MI, 48109.
References
- 1.American Cancer Society. 2012. Cancer Facts & Figures 2012, Atlanta. [Google Scholar]
- 2.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 3.Bodenmann G. Dyadic coping and its signi!cant for marital functioning. In: Revenson T, Kayser K, Bodenmann G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. Washington, D.C.: American Psychological Association; 2005. pp. 33–50. [Google Scholar]
- 4.Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 5.Cook WL, Kenny DA. The Actor-Partner Interdependence Model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 2005;29:101. [Google Scholar]
- 6.Crook JM, Gomez-Iturriaga A, Wallace K, Ma C, Fung S, Alibhai S, Jewett M, Fleshner N. Comparison of Health-Related Quality of Life 5 Years After SPIRIT: Surgical Prostatectomy Versus Interstitial Radiation Intervention Trial. Journal of Clinical Oncology. 2011;29:362–368. doi: 10.1200/JCO.2010.31.7305. [DOI] [PubMed] [Google Scholar]
- 7.Eisemann N, Waldmann A, Rohde V, Katalinic A. Quality of life in partners of patients with localised prostate cancer. Qual Life Res. 2014;23:1557–1568. doi: 10.1007/s11136-013-0588-1. [DOI] [PubMed] [Google Scholar]
- 8.Ezer H, Chachamovich JL, Chachamovich E. Do men and their wives see it the same way? Congruence within couples during the first year of prostate cancer. Psycho-oncology. 2011;20:155–164. doi: 10.1002/pon.1724. [DOI] [PubMed] [Google Scholar]
- 9.Galbraith ME, Fink R, Wilkins GG. Couples Surviving Prostate Cancer: Challenges in Their Lives and Relationships Seminars in Oncology Nursing. 2011;27:300–308. doi: 10.1016/j.soncn.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Green HJ, Wells DJN, Laakso L. Coping in men with prostate cancer and their partners: a quantitative and qualitative study. European Journal of Cancer Care. 2011;20:237–247. doi: 10.1111/j.1365-2354.2010.01225.x. [DOI] [PubMed] [Google Scholar]
- 11.Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Harden JK, Sanda MG, Wei JT, Yarandi H, Hembroff L, Hardy J, Northouse LL. Partners' long-term appraisal of their caregiving experience, marital satisfaction, sexual satisfaction, and quality of life 2 years after prostate cancer treatment. Cancer nursing. 2013;36:104–113. doi: 10.1097/NCC.0b013e3182567c03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Helgeson VS, Novak SA, Lepore SJ, Eton DT. Spouse Social Control Efforts: Relations to Health Behavior and Well-Being among Men with Prostate Cancer. Journal of Social and Personal Relationships. 2004;21:53–68. [Google Scholar]
- 14.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA, Edwards BK. SEER Cancer Statistics Review, 1975–2008. Bethesda MD: National Cancer Institute; 2011. http://seer.cancer.gov/csr/1975_2008/, posted to the SEER web site, 2011. [Google Scholar]
- 15.Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 16.Kelley HH, Thibaut JW. New York: Wiley; 1978. Interpersonal relations : a theory of interdependence. [Google Scholar]
- 17.Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. New York, NY: The Guilford Press; 2006. [Google Scholar]
- 18.Kershaw T, Mood D, Newth G, Ronis DL, Sanda M, Vaishampayan U, Northouse LL. Longitudinal analysis of a model to predict quality of life in prostate cancer patients and their spouses. Annals of Behavioral Medicine. 2008;36:117–128. doi: 10.1007/s12160-008-9058-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- 20.Lewis FM. Family Home Visitation Study Final Report. National Cancer Institute, National Institutes of Health; 1996. Family Home Visitation Study Final Report. [Google Scholar]
- 21.Lewis FM. The Family's "Stuck Points" in Adjusting to Cancer. In: Holland JC, Breitbart WS, Jacobsen PB, Lederberg MS, Loscalzo MJ, McCorkle R, editors. Psycho-oncology. New York: Oxford University Press; 2010. pp. 511–515. [Google Scholar]
- 22.Macho S, Ledermann T. Estimating, testing, and comparing specific effects in structural equation models: the phantom model approach. Psychological methods. 2011;16:34–43. doi: 10.1037/a0021763. [DOI] [PubMed] [Google Scholar]
- 23.Manne S, Badr H, Zaider T, Nelson C, Kissane D. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. J Cancer Surviv. 2010;4:74–85. doi: 10.1007/s11764-009-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCubbin HI, Thompson AI. Family typologies and family assessment. In: McCubbin HI, Thompson AI, editors. Family Assessment Inventories for Research and Practice. Madison, Wisconsin: The University of Wisconsin-Madison; 1991. [Google Scholar]
- 25.McCubbin MA, McCubbin HI. Family Stress Theory and Assessment. In: McCubbin HI, Thompson AI, editors. Family Assessment Inventories for Research and Practice. Madison, Wisconsin: The University of Wisconsin-Madison; 1991. [Google Scholar]
- 26.Mood D, Song L, Kershaw T, Northouse L. Assessing risk for distress in cancer patients and family caregivers. Oncology Nursing Forum. 2007;34:233. [Google Scholar]
- 27.Muthen L, Muthen B. Mplus User's Guide. Sixth. Los Angeles: 2015. Mplus User's Guide. [Google Scholar]
- 28.Northouse L, Kershaw T, Mood D, Schafenacker A. Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psycho-oncology. 2005;14:478–491. doi: 10.1002/pon.871. [DOI] [PubMed] [Google Scholar]
- 29.Northouse LL, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, Galvin E, Decker V. Quality of life of women with recurrent breast cancer and their family members. Journal of Clinical Oncology. 2002;20:4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- 30.Northouse LL, Mood D, Montie JE, Sandler HM, Forman JD, Hussain M, Pienta K, Smith DC, Sanda MG, Kershaw T. Living with Prostate Cancer: Patients' and Spouses' Psychosocial Status and Quality of Life. Journal of Clinical Oncology. 2007;25:4171–4177. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- 31.Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, Lorusso P, Hayes DF, Hussain M, Ruckdeschel J, Fendrick AM, Trask PC, Ronis DL, Kershaw T. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psycho-oncology. 2013;22:555–563. doi: 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Northouse LL, Mood DW, Schafenacker A, Montie JE, Sandler HM, Forman JD, Hussain M, Pienta KJ, Smith DC, Kershaw T. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007;110:2809–2818. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- 33.Oberst M. Appraisal of Caregiving Scale: Manual for Use. Detroit: Wayne State University; 1991. Appraisal of Caregiving Scale: Manual for Use. [Google Scholar]
- 34.Oberst M. Appraisal of Illness Scale: Manual for Use. Detroit: Wayne State University; 1991. Appraisal of Illness Scale: Manual for Use. [Google Scholar]
- 35.Penedo FJ, Benedict C, Zhou ES, Rasheed M, Traeger L, Kava BR, Soloway M, Czaja S, Antoni MH. Association of stress management skills and perceived stress with physical and emotional well-being among advanced prostrate cancer survivors following androgen deprivation treatment. Journal of clinical psychology in medical settings. 2013;20:25–32. doi: 10.1007/s10880-012-9308-1. [DOI] [PubMed] [Google Scholar]
- 36.Prince-Paul M. Relationships among communicative acts, social well-being, and spiritual well-being on the quality of life at the end of life in patients with cancer enrolled in hospice. Journal of Palliative Medicine. 2008;11:20–25. doi: 10.1089/jpm.2007.0119. [DOI] [PubMed] [Google Scholar]
- 37.Regan TW, Lambert SD, Kelly B, Falconier M, Kissane D, Levesque JV. Couples coping with cancer: exploration of theoretical frameworks from dyadic studies. Psycho-oncology. 2015 doi: 10.1002/pon.3854. [DOI] [PubMed] [Google Scholar]
- 38.Rusbult C, Van Lange P. Interdependence processes. In: Higgins E, Kruglanski A, editors. Social psychology: Handbook of basic principles. New York: The Guilford Press; 1996. pp. 564–596. [Google Scholar]
- 39.Segrin C, Badger TA, Harrington J. Interdependent psychological quality of life in dyads adjusting to prostate cancer Health psychology : official journal of the Division of Health Psychology. American Psychological Association. 2012;31:70–79. doi: 10.1037/a0025394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Song L, Northouse LL, Braun TM, Zhang L, Cimprich B, Ronis DL, Mood DW. Assessing longitudinal quality of life in prostate cancer patients and their spouses: a multilevel modeling approach. Qual Life Res. 2011;20:371–381. doi: 10.1007/s11136-010-9753-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Song L, Northouse LL, Zhang L, Braun TM, Cimprich B, Ronis DL, Mood DW. Study of dyadic communication in couples managing prostate cancer: a longitudinal perspective. Psycho-oncology. 2010;21(1):72–81. doi: 10.1002/pon.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Traa MJ, De Vries J, Fau - Bodenmann G, Bodenmann G, Fau - Den Oudsten BL, Den Oudsten BL. Dyadic coping and relationship functioning in couples coping with cancer: a systematic review. doi: 10.1111/bjhp.12094. [DOI] [PubMed] [Google Scholar]
- 43.Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]