Figure 1. The Retina-Choroid Interface in AMD: Schematic Diagram of the Choroid and Retina in the Eye.
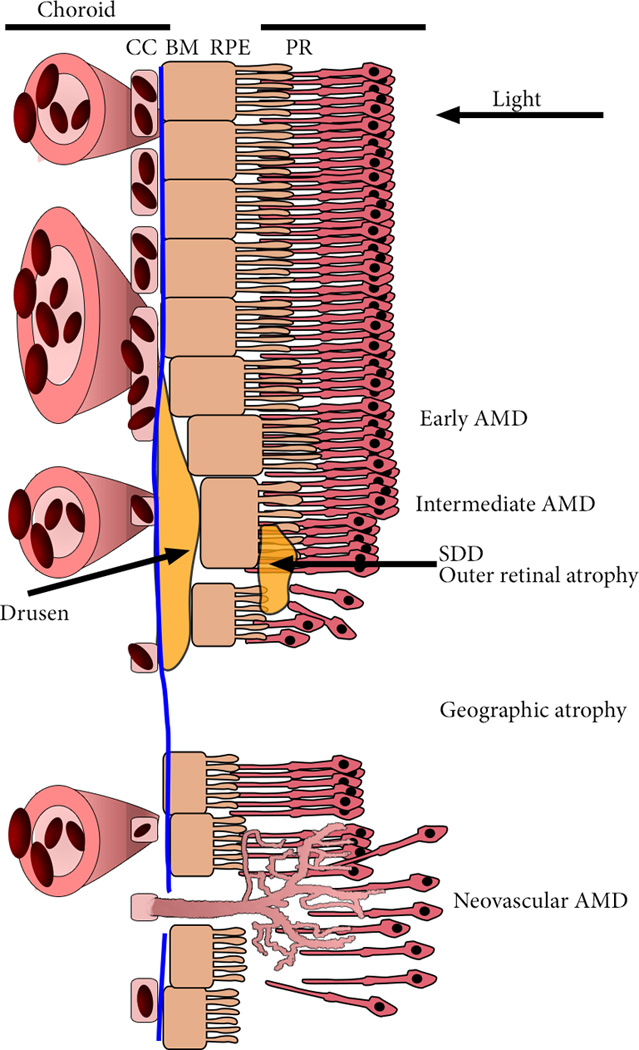
Light entering from the right is focused on the outer retinal photoreceptors (PR). PR are supported by the retinal pigmented epithelium (RPE) and the choroidal vasculature. The innermost layer of the choroid is the choriocapillaris (CC), a thin, dense, highly anastomotic microvascular structure. Between the RPE and the CC is Bruch’s membrane (BM), a specialized multi-layered extracellular matrix that divides the ‘inside’ and ‘outside’ of the eye. The first clinical presentation of AMD is the presence of drusen, extracellular debris that most often develop basal to the RPE, in between CC lumens, and subretinal drusenoid deposits (SDD) that develop between the RPE and photoreceptor layer, and cause outer retinal degeneration. AMD progresses to either geographic atrophy (GA), the gradual atrophy of the choroid, RPE and photoreceptors, and neovascular AMD, aberrant angiogenesis of the choroid through ruptures in BM and the RPE to the PR. Leakage of blood constituents into the retina causes disorganization and swelling of the retina, frequently incompatible with vision.
