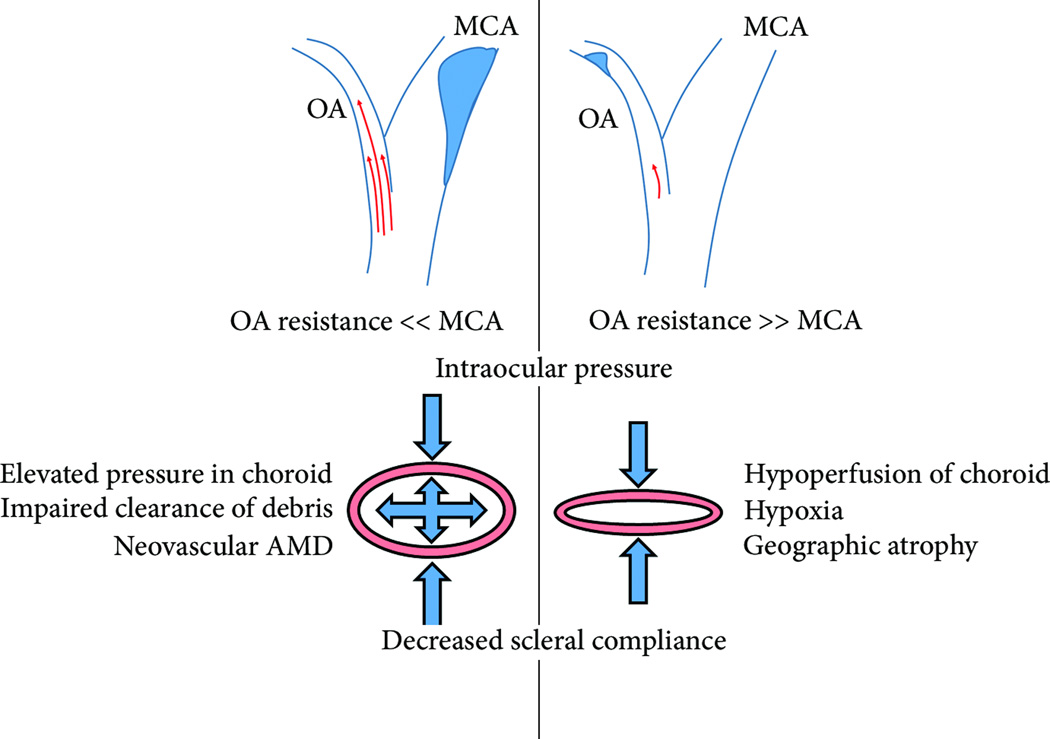
Figure 2. Friedman’s Hemodynamic Theory of AMD.
In 1998 Friedman formally postulated that increased stiffness of the sclera, (supportive fibrous structure that lies posterior to the choroid), and BM, promotes AMD pathogenesis. By this model, the progression towards ‘wet’ or ‘dry’ AMD depends on whether the ophthalmic artery (OA), which provides blood the retinal and choroidal circulations, or the middle cerebral artery (MCA) provides greater vascular resistance. In the case where the OA provides less resistance due to intimal constriction of the the MCA, results in elevated blood pressure in the choroidal vasculature. Because of increased scleral stiffness to the posterior, and intraocular pressure to the anterior, elevated pressure within the choroidal vasculature results in hydrostatic pressure. Friedman postulated that this elevated hydrostatic pressure prevents the clearance of debris from the RPE layer to the choroid, and that this was the cause of neovascular AMD. If, on the other hand, the OA provides more resistance due to intimal constriction of the MCA, the choroid is hypoperfused. The choroid thins or collapses between intraocular pressure and a rigid sclera. Friedman postulated that choroidal hypoperfusion caused hypoxia and was responsible for geographic atrophy.