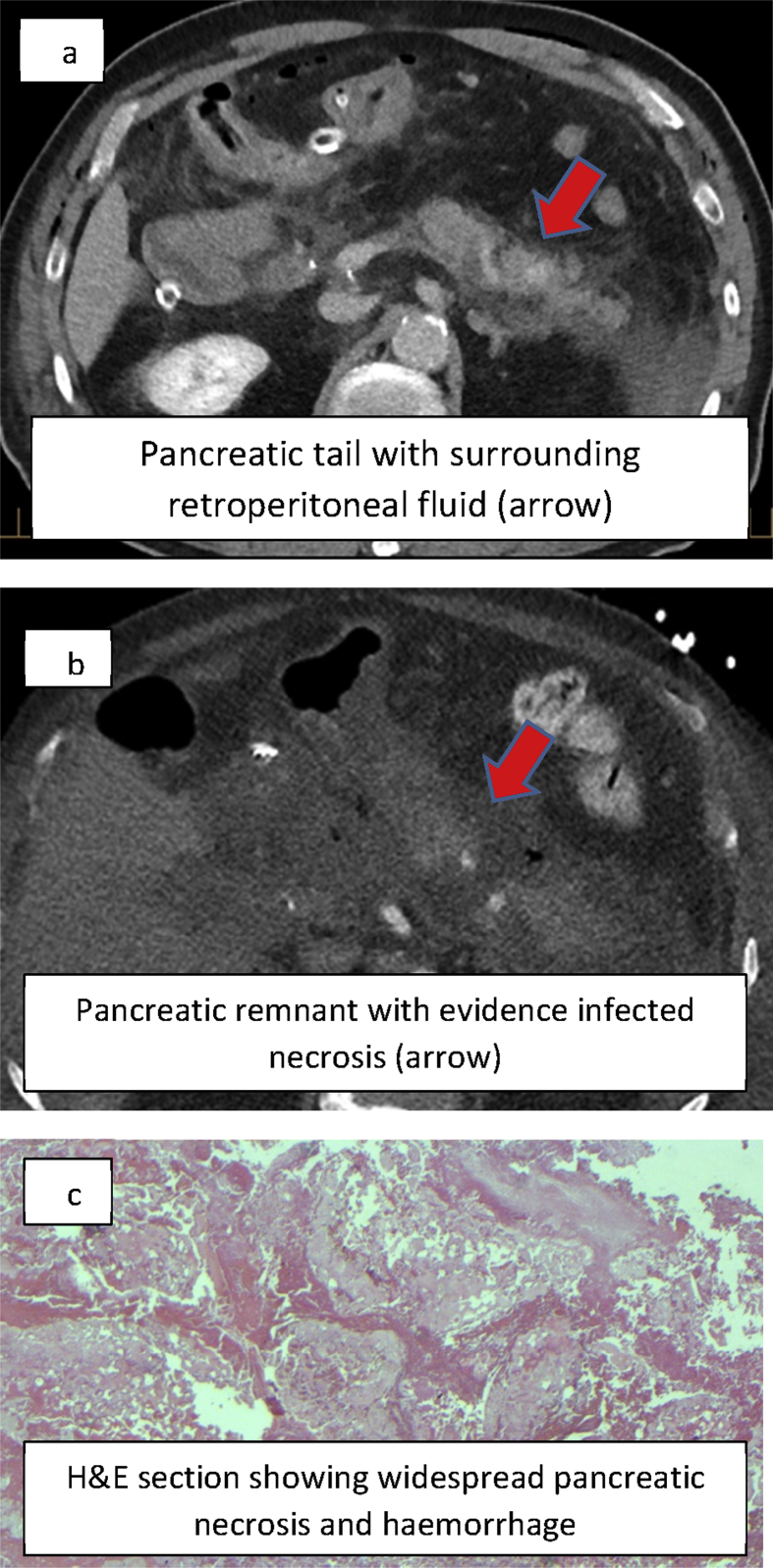
Figure 1.
A 71 year old man who underwent pancreaticoduodenectomy (PD) for T1 N0 duodenal carcinoma. Anaerobic threshold unknown. Intrathecal morphine was used. No somatostatin analogues or perioperative NSAID's were administered. Standard dissection for PD was performed. Fistula risk score was six. Pancreatic neck was transected by ligasure. Binding pancreaticogastrostomy was performed. Post-operative day (POD) 1 patient was confused, tachycardic, serum amylase 7 x > upper limit normal. Urinary TRP2 was not measured. POD 1 CT scan showed evidence of post-operative pancreatitis (Fig. 1a). POD 2 CRP was 359 mg/L. POD 17 patient became increasingly unwell. Repeat CT showed evidence of infected pancreatic necrosis (Fig. 1b). POD 17 operative findings were of intact anastomosis but segmental pancreatic necrosis. Partial pancreatectomy by debridement (anastomosis taken down) and wide bore drainage to remnant pancreatic bed. Initial clinical improvement followed by clinical deterioration at POD 27. Completion pancreatectomy performed. Histologically confirmed pancreatic necrosis within the remnant (Fig. 1c)